|
Size: 14667
Comment:
|
Size: 14748
Comment:
|
| Deletions are marked like this. | Additions are marked like this. |
| Line 2: | Line 2: |
| = Adipose Tissue as an Endocrine Organ = '''Introduction: During the past 20 years studies have shown the importance of white adipose tissue (WAT) as an endocrine organ (Proenca, et al., 2014). WAT is responsible for secreting biological active cytokines termed adipokines. Adipokines have various roles in different processes in the body ranging from regulation of hunger/satiety via the hypothalamus, pro inflammation, etc. (Khan and Joseph, 2014). Adipokines act as endocrine hormones via blood circulation, binding to receptors in different tissues leading to a cascade of different processes in the various body parts. Adipose tissue (AT) has a part in initiating metabolic syndrome by e.g. inducing insulin- and leptin resistance, which is thought to be a risk factor promoting obesity. ''' |
= The endocrine effects of adipose tissue on obesity = Introduction: During the past 20 years studies have shown the importance of white adipose tissue (WAT) as an endocrine organ (Proenca, et al., 2014). WAT is responsible for secreting biological active cytokines termed adipokines. Adipokines have various roles in different processes in the body ranging from regulation of hunger/satiety via the hypothalamus, pro inflammation, etc. (Khan and Joseph, 2014). Adipokines act as endocrine hormones via blood circulation, binding to receptors in different tissues leading to a cascade of different processes in the various body parts. Adipose tissue (AT) has a part in initiating metabolic syndrome by e.g. inducing insulin- and leptin resistance, which is thought to be a risk factor promoting obesity. |
| Line 31: | Line 31: |
| Line 32: | Line 33: |
| {{attachment:Adipokines.jpg}} ----- |
{{attachment:Adipokines1.jpg}} |
| Line 51: | Line 52: |
| Line 53: | Line 55: |
| B. Antuna-Puente, B. Feve, S. Fellahi, and J.-P. Bastard. ”''Adipokines: The missing link between insulin resistance and obesity.''” Diabetes & Metabolism, nr 34 (2008): 2-11. | B. Antuna-Puente, B. Feve, S. Fellahi, and J.-P. Bastard. ”''Adipokines: The missing link between insulin resistance and obesity.''” Diabetes & Metabolism, nr 34, pg. 2-11. (2008). |
| Line 55: | Line 57: |
| S. Golbidi, and I. Laher. ”''Exercise Induced Adipokine Changes and the Metabolic Syndrome.''” Journal of Diabetes Research, 2014: 1-16. | S. Golbidi, and I. Laher. ”''Exercise Induced Adipokine Changes and the Metabolic Syndrome.''” Journal of Diabetes Research, pg. 1-16. (2014). |
| Line 57: | Line 59: |
| M. Khan, and F. Joseph. ”''Adipose Tissue and Adipokines: The Association with and Application of Adipokines in Obesity''.” Scientifica, 2014: 1-7. | M. Khan, and F. Joseph. ”''Adipose Tissue and Adipokines: The Association with and Application of Adipokines in Obesity''.” Scientifica, pg. 1-7. (2014). |
| Line 59: | Line 61: |
| V. de Oliveira Leal, and D. Mafra. ”''Adipokines in obesity''.” Clinica Chimica Acta, nr 419 (2013): 87-94. | V. de Oliveira Leal, and D. Mafra. ”''Adipokines in obesity''.” Clinica Chimica Acta, nr 419, pg. 87-94. (2013). |
| Line 61: | Line 63: |
| A.R.G. Proenca, R.A.L. Sertié, A.C. Oliveira, A.B. Campaña, R.O. Caminhotto, P. Chilin, and F.B. Lima. ”''New concepts in white adipose tissue physiology.''” Brazilian Journal of Medical Biological Research, nr 47 (2014): 192-205. | A.R.G. Proenca, R.A.L. Sertié, A.C. Oliveira, A.B. Campaña, R.O. Caminhotto, P. Chilin, and F.B. Lima. ”''New concepts in white adipose tissue physiology.''” Brazilian Journal of Medical Biological Research, nr 47, pg.192-205. (2014). '''Figures''': Fig 1 - Made by A. Gloveus |
The endocrine effects of adipose tissue on obesity
Introduction: During the past 20 years studies have shown the importance of white adipose tissue (WAT) as an endocrine organ (Proenca, et al., 2014). WAT is responsible for secreting biological active cytokines termed adipokines. Adipokines have various roles in different processes in the body ranging from regulation of hunger/satiety via the hypothalamus, pro inflammation, etc. (Khan and Joseph, 2014). Adipokines act as endocrine hormones via blood circulation, binding to receptors in different tissues leading to a cascade of different processes in the various body parts. Adipose tissue (AT) has a part in initiating metabolic syndrome by e.g. inducing insulin- and leptin resistance, which is thought to be a risk factor promoting obesity.
Metabolic syndrome:
When referring to the metabolic syndrome numerous different symptoms are included. These consist of insulin resistance, high blood pressure, dyslipidemia, thrombosis and obesity (Antuna-Puente, et al., 2008). Metabolic syndrome increases the risk of developing type II diabetes, cardiovascular disease and cancer. This has become one of today’s biggest health issues both in developed and developing countries (Golbidi and Laher, 2014).
Insulin:
Is one of the body’s three most important hormones and the lack of it leads to death. It is produced by the beta-cells in the endocrine parts of the pancreas, the Islets of Langerhans. The main function of insulin is storage and boosted glucose oxidation. Secretion is biphasic, stimulated by both feed-forward mechanism of enteroglucagon and GIP (gastric inhibitory peptide), and the increase of blood glucose levels. Adipokines both have an indirect and direct effect on the resistance of insulin (may be due to down regulation or malfunction of insulin receptors in insulin dependent tissues). Hyperglycemia is one of the results of insulin resistance entailing risks of cardio vascular disease and diabetes mellitus.
Adipose tissue (AT):
The tissue that is usually considered fat is of two origins, abdominal or visceral and subcutaneous or peripheral. The two types display different ratios of adipokines thereby showing different functions. Subcutaneous fat is responsible for 80% of all leptin secretion and visceral only 20% (Leal and Mafra, 2013), also adiponectin is found in higher concentrations in subcutaneous compared to visceral. Both TNF-alpha and IL-6 are found primarily in visceral fat, TNF-alpha exclusively (Antuna-Puente, et al., 2008). AT is composed of adipocytes divided into two main groups: White adipose tissue (WAT) and brown adipose tissue (BAT). In WAT the adipocytes are composed of a single lipid droplet containing triacylglycerol (TAG). TAG is composed of three fatty acids and a glycerol. The fatty acids are collected from an external source such as VLDL and chylomicrons (Proenca, et al., 2014). WAT is considered as the largest energy reservoir, which can be utilized during starvation and large energy consumption (lipolysis, mainly TAG, further enabling gluconeogenesis). The other part of AT is Brown adipose tissue (BAT) which is composed of several lipid droplets having brownish color. This is due to the high concentration of cytochrome oxidase. BATs main function is thermogenesis, especially in newborns, rodents and hibernating animals.
Adipokines:
Adipokines are cytokines, which are cell signaling proteins, secreted and synthesized by adipose tissue. Many processes are inhibited or stimulated by the effects of the different adipokines (Leal and Mafra, 2013). The physiological processes effected consists of the regulation of hunger/ satiety, increase and decrease of blood pressure, inducing acute phase response, crosslinking immune system and endocrine system and major metabolic processes such as lipid metabolism and glucose homeostasis. The different known adipokines are as followed: Leptin (Leptin resistance is one of the major theories for obesity), Adiponectin (known as the positive adipokine), TNF-alpha (important component of acute phase response and regulator of lipolysis and lipogenesis), IL-6 (has effect on inducing insulin-resistance), Angiotensinogen (precursor of the renin-angiotensin system regulating blood pressure), Resistin (induces insulin-resistance by acting on AMPK-pathway in liver), Plasminogen activator inhibitor-1 (PAI-1; unsure but may have effect on insulin resistance and thereby obesity), and Vaspin (been shown to improve insulin sensitivity and glucose tolerance) (Antuna-Puente, et al., 2008).
Leptin:
16-kDa hormone secreted from AT. Leptin acts on the hypothalamus (HT), suppressing appetite and increase the energy expenditure through metabolism as well as modulating bodyweight and lipid storage. It acts in the HT by inhibiting the release of Neuro peptide-Y (NP-Y), GABA, Proopiomelanocortin (POMC) and also directly on skeletal muscle, increasing fatty acid oxidation via AMPK-activation. Other tissues such as placenta, mucosa of gastric fundus, skeletal muscle and mammary gland epithelial cells also express leptin. Leptin receptors are called Ob-R, primarily found in the brain but also in several peripheral tissues including AT, placenta, adrenal medulla, liver, pancreatic Beta cells, lung, intestinal cells, blood mononuclear cells, articular chondrocytes, hearth and skeletal muscle (Proenca, et al., 2014). These receptors are important because they bind leptin and can transport leptin trough the blood brain barrier (BBB) (Golbidi and Laher, 2014). Without this, leptin will not be able to enter the brain and inhibit the hunger center in the HT. Six types of leptin receptors are known so far. All encoded on the same gene. Plasma leptin levels depend on the total adipose tissue mass. Large depots of adipose tissue result in high levels of blood leptin, which may lead to leptin resistance due to down regulation of receptors. Leptin itself exerts a positive effect on suppressor of cytokine signaling (SOCS)-3. Which may inhibit insulin signaling within the cell and effect insulin receptors and therefor insulin resistance. Insulin resistance will increase blood glucose level and hyperglycemia. A state in which leptin promotes platelet aggregation as well as cholesterol uptake into macrophages (Antuna-Puente, et al., 2008).
Adiponectin:
Is a 30-kDa polypeptide. This is a hormone exclusively secreted by the WAT and it is also known to be the beneficial adipokine as it usually improves insulin sensitivity. There are two different types of receptors, these are called adipo-R1 and adipo-R2. Adipo-R1 is associated with the activation of the AMPK-pathway, which will decrease gluconeogenesis enzyme expression. Adipo-R2 activates the PPAR alpha-pathway, which reduces inflammation and oxidative stress. Which means non-functioning adiponectin receptors lead to reduced insulin sensitivity, inflammation and oxidative stress (Golbidi and Laher, 2014). It does this by acting on the AMP-protein kinase. Adiponectin mainly affects liver, skeletal muscle, vascular wall and endothelial cells. The AMPK-pathway in the liver activated by adiponectin results in various metabolic effects for example, insulin sensitivity and the increase in fatty acid oxidation. Adiponectin will act on the intravasal wall by inhibiting cell adhesion of, for instance monocytes, by decreasing the cell adhesion it also decreases the transformation of macrophages into foam-cells. Foam cells are lipid-filled macrophages induced by inflammation. Foam cells could lead to atherosclerosis. It stimulates the formation of new blood vessels as well as increasing the production of nitric monoxide, a vasodilator (Khan and Joseph, 2014). Additionally adiponectin acts in reducing inflammatory response by endothelial cells, through acting negatively on TNF-alpha.
TNF-alpha (Tumor necrosis factor-alpha):
26-kDa transmembrane protein that is going to activate stress related kinases which would mobilize fat deposits from periphery to center. It is also going to increase the fatty acid uptake in the liver, which could result in fatty liver (hepatic steatosis). Furthermore it will increase insulin resistance. It is a pro inflammatory cytokine, produced by various cells but mainly macrophages and lymphocytes. Hypertrophy in adipose tissue may lead to inflammation, accumulating the aggregation of macrophages and thereby increasing the secretion of TNF-alpha. TNF-alpha’s main role is pro-inflammatory. It has a central role in chronic inflammatory state in obesity and an increasing effect on Leptin expression, IL-6 production is enhanced and a reducing effect on adiponectin secretion. It will also have a major role in cell death (Apoptosis). TNF-alpha stimulates cell adhesion, which may lead to atherosclerosis, opposite effect of adiponectin. (Golbidi and Laher, 2014)
IL-6 (Interleukin-6):
IL-6 is a cytokine produced by various cells such as fibroblasts, endothelial cells, monocytes and adipose tissue. IL-6 has different effects, pro inflammatory as well as regulator of lipid metabolism. IL-6 secretion and expression is directly proportional to insulin resistance, glucose tolerance and degree of obesity (Khan and Joseph, 2014). High concentration of IL-6 is going to impair the insulin receptor, this is carried out by either inhibiting the tyrosine phosphatase or inhibiting intracellular SOCS signaling affecting the insulin receptor (Leal and Mafra, 2013). IL-6 will stimulate the secretion of C-reacting protein from the liver. C-reacting protein is inflammatory. There is a direct correlation between high levels of adipose interleukine-6 levels and blood c-reacting protein (CRP), which can further lead to cardiovascular disease.
Effects of training on adipokines and obesity:
The general effects of training are none or very limited in a short-term perspective. However over a longer period of time, the positive effects on the metabolic syndrome are many. Burning of fat will lead to a lower expression of inflammatory adipokines (TNF-alpha and IL-6) in circulation and lower leptin resistance (Golbidi and Laher, 2014).
Leptin:
Many studies have been conducted concerning exercise and its effect on leptin plasma levels. However the results have been inconclusive due to human factors. But what can be shown is that strenuous exercise in the long term does have a slight effect on leptin levels, through lipolysis induced during exercise. The burning of fat (producer of leptin) will increase, decreasing leptin in blood. Diabetic patients showed better response than none diabetic control group.
Adiponectin:
As it has been established that exercise reduces insulin resistance and enhances glucose metabolism. Studies have been made trying to correlate exercise, adiponectin levels and insulin function. Also here results have been hard to interpret due to the different human factors. Summation of results show that in overweight individuals with adequate intensity workout might lead to an increase in adiponectin blood plasma level. More research is however needed.
TNF-alpha:
One of the main effects of this adipokine is its role in inducing insulin resistance. With training a reduction of circulating TNF-alpha can be seen decreasing the risk of TNF-alpha prompted insulin resistance. Further, via adipose tissue atrophy, infiltration of immunocytes into the AT will decrease, thereby resulting in a decreased expression of TNF-alpha.
IL-6:
Just as in the case of TNF-alpha, the release of AT derived IL-6 will be lowered as the inflammation of adipose tissue diminishes. Not only adipose tissue will produce IL-6 but also muscle cells. Training and a greater muscle mass will increase production of muscle derived IL-6 (pro inflammatory) during exercise. This will mediate an increase in additional anti-inflammatory cytokines. However, the amount of IL-6 (adipokine) in circulation will decrease as an effect of training in the metabolic syndrome and in obese patients.
Summation:
Adipose tissue has long been known to release signaling peptides. The idea of adipokines was first suggested in 1948. However it was not until leptin was discovered 1994 that WAT started to be considered as an endocrine organ and the presence of adipokines was confirmed (Khan and Joseph, 2014). Since then many more adipokines have been found and are still being found and explored. Reason for regarding AT as an endocrine organ are many, e.g. the way it connects the immune system and the endocrine system or the fact that it effects distant parts of the body through its secretion of adipokines into circulation. Not only does AT stimulate effects on many parts of the body through the release of adipokines. But, they also display receptors for cytokines that act on AT through autocrine, paracrine and endocrine pathways by modulating adipogenesis, apoptosis, lipogenesis, lipolysis and affecting AT´s secretion of adipokines (Proenca, et al., 2014). Through exercise an increase in release of various cytokines from different tissues will further stimulate AT and thereby enhancing its functions (Golbidi and Laher, 2014). Hypertrophy of AT may illicit hypoxia. Increasing inflammatory response and secretion of TNF-alpha and IL-6, repressing production of adiponectin (the good adipokine) (Khan and Joseph, 2014). Based on the current studies that display an overview on the endocrine functions of AT, it can be seen that more research is needed to fully elucidate and understand the subject.
Reference list:
B. Antuna-Puente, B. Feve, S. Fellahi, and J.-P. Bastard. ”Adipokines: The missing link between insulin resistance and obesity.” Diabetes & Metabolism, nr 34, pg. 2-11. (2008).
S. Golbidi, and I. Laher. ”Exercise Induced Adipokine Changes and the Metabolic Syndrome.” Journal of Diabetes Research, pg. 1-16. (2014).
M. Khan, and F. Joseph. ”Adipose Tissue and Adipokines: The Association with and Application of Adipokines in Obesity.” Scientifica, pg. 1-7. (2014).
V. de Oliveira Leal, and D. Mafra. ”Adipokines in obesity.” Clinica Chimica Acta, nr 419, pg. 87-94. (2013).
A.R.G. Proenca, R.A.L. Sertié, A.C. Oliveira, A.B. Campaña, R.O. Caminhotto, P. Chilin, and F.B. Lima. ”New concepts in white adipose tissue physiology.” Brazilian Journal of Medical Biological Research, nr 47, pg.192-205. (2014).
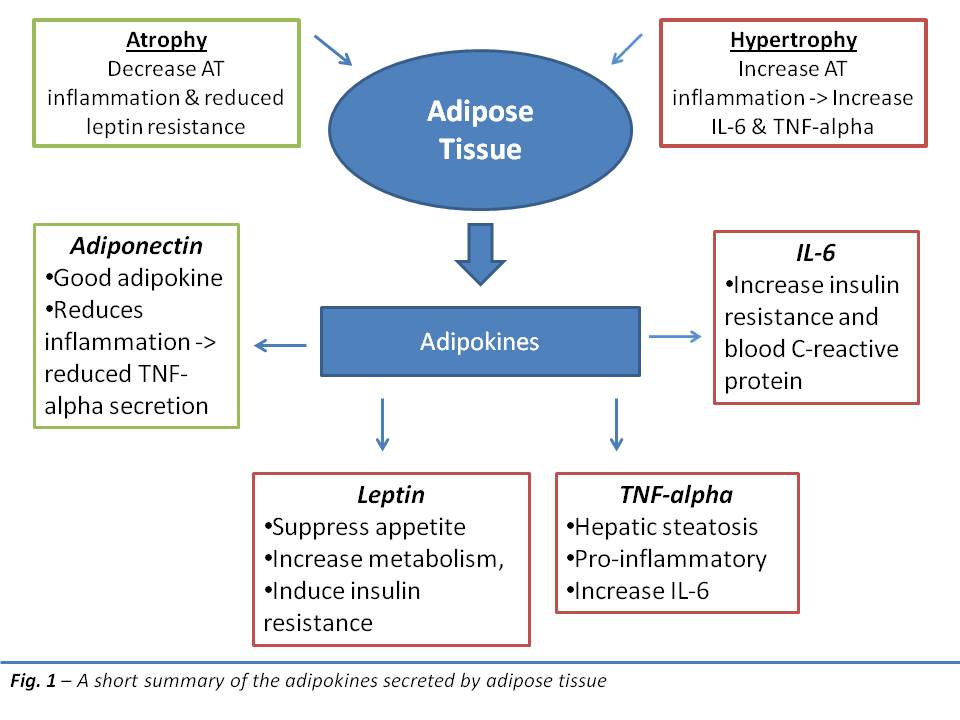
Figures:
Fig 1 - Made by A. Gloveus
