Circadian rhythm and its effects on food intake
Contents
Intro
This essay will explore the relationship between circadian rhythms and the regulation of metabolism focusing on the effects it has on food intake. Circadian rhythms are defined as any cycle which has a duration of 24 hours, with endogenous cues, but influenced by exogenous zeitgebers (cues). This includes the sleep-wake cycle and its regulation by melatonin, influenced by fluctuations in daylight. A fundamental characteristic of living animals is rhythmicity which is ensured by the circadian and sleep-wake cycles. An essential role of the circadian rhythm is to organise the body’s metabolism with the day/night alteration (sleep-wake cycle).
The sleep-wake cycle is basically defined by the awakening of an animal and their sleeping cycle. It usually revolves around a 24-hour clock but some research has shown that it could be shorter or longer depending on the individual (Garbazza et al., 2016). The molecular mechanisms by which hypothalamic neurons regulate the sleep-wake cycle with appetite and metabolism remain unclear (Starling, 2019). New research (Chen, 2019) suggests a transcriptional basis for the rhythmic control of hunger by the Agouti-related protein (AgRP) neuron molecular clock.
Homonal physiology of food intake regulation
Traditionally food intake is regarded as being controlled by endogenous endocrine factors which are released in response to a meal. Today, research has shown that exogenous factors such as social meal times, and the role of certain neurotransmitters is undeniable. As such, appetite was considered to be induced during a fasting period, when glucagon’s effects could no longer satisfy the metabolic needs of the organism. Today, many factors are taken into account when explaining food-intake regulation. Firstly, the endocrine endogenous mechanisms are explained below. As with all conscious behaviours, the brain is the first to respond to the sensory input which food represents. Chemo and mechanoreceptors in the gastrointestinal tract also relay sensory input to the brain via the autonomic nervous system.
Following a meal, Cholecystokinin (CKK) is released following the presence of (mainly) lipid and protein-filled chyme in the duodenum. Not only does it stimulate the digestion of proteins and lipids by increasing pancreatic and hepatic secretions, but it acts as a hunger suppressant via vagal afferent fibres. (Goes to the nucleus tractus solitarius)
Glucagon-like peptide (GIP) is secreted by intestinal enteroendocrine cells in response to food intake. Its role is to stimulate the secretion of insulin (incretin), lowering blood sugar as a result. It also reduces gastric emptying, secretion, and motility, which promotes satiety.
Peptide - Y is released from endocrine cells in ileum and proximal segments of the large intestine mostly after a meal. It reduces gastric emptying (activates ileal brake) thus also promoting satiety.
Amylin is secreted from the endocrine pancreatic islets. It is co-secreted with insulin from B-cells, supplementing its response to hyperglycemia and also inhibiting the release of Glucagon from A-cells in order to continue lowering blood glycaemia.
Ghrelin is released from enteroendocrine cells of the G.I.T. Its role is to ‘prepare’ the digestive system for food intake by increasing gastric motility and secretions just before a meal. Not only does it have significant endocrine effects on the GIT, but it also widely impacts neural processes, particularly the hypothalamus (nucleus arcuatus). Grelin will cause the release of neuropeptide-Y which then stimulates appetite. Its role is mainly short-term.
Leptin is synthesized by enterocytes and adipose tissues; its primary function is to regulate adipose tissue mass and hunger. It acts directly on leptin receptors of cells, and indirectly mediates the effects of other endocrine food-intake/metabolism regulators. Leptin’s action in the hypothalamus via leptin receptors inhibits hunger sensations. Leptin’s exact mechanism is complex, and not completely understood. (Hopkins et al., 2000; Klok et al., 2007)
Increased levels of melatonin cause a down-regulation of leptin. Sleep-deprivation associated with low leptin. (Kus et al., 2004)
Only recently has the role of a circadian rhythm in feeding behavior been considered (explained later).
Pathology
Behavioral changes
Disturbed circadian rhythm has many negative effects on the metabolism of different organ systems, and on food intake behavior. On the behavior side, humans who have their circadian rhythms disrupted (kept awake in light conditions for an entire night) show a marked preference for higher-fat foods than those that have maintained a normal light-dark and sleep-wake cycle. (Cain et al., 2015) This can lead to obesity and related illnesses in those who frequently have disturbed circadian rhythms.
Digestive effects
In the digestive tract itself it has been found that disrupted circadian rhythms cause increased permeability of the intestinal epithelial layer in mice, causing gut leakiness. (Summa et al., 2013) This can lead to increased gut inflammation, as well as a change in the microbiome of the gut. This increased intestinal permeability also allows for the damage of other organs, such as liver cells, when harmful materials are able to leave the digestive tract. Disrupted circadian rhythms also have an impact on the skeletal system, specifically the joints.
Skeletal effects
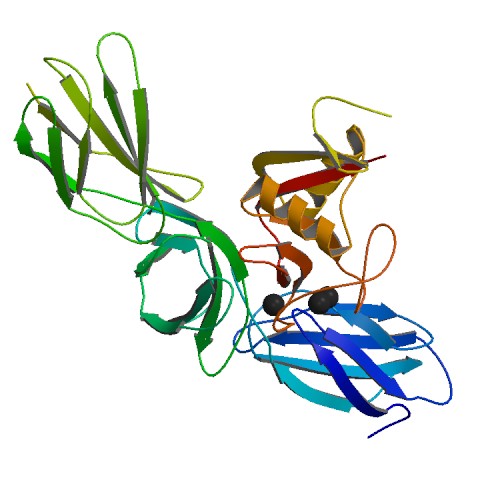
Disrupted circadian rhythms also have an impact on the skeletal system, specifically the joints. In a study by Kc et al. (2015) when mice were fed a high fat diet, those who’s circadian rhythms were artificially shifted showed an increased progression of osteoarthritis over their non-shifted counterparts. There were also more pronounced signs of knee osteoarthritis in shifted mice fed a normal diet over their non-shifted counterparts. Cartilage is formed by both collagen and proteoglycans, which are mucopolysaccharide bonded proteins found in connective tissue. They serve to fill in the gaps between an organism's cells and regulate the movement of molecules through the cell matrix.
|
Figure 1 Aggrecan, the major proteoglycan in cartilage, has 2316 amino acids |
Both sets of mice with a shifted circadian rhythm had decreased proteoglycans in their joints, but those fed a high fat diet show a much more pronounced proteoglycan decrease, as well as increased joint fibrillation. Neither set of non-shifted mice showed significant proteoglycan changes. When histopathological osteoarthritis grading was performed, with a higher score indicating more severe pathology, normal-diet non-shifted mice scored lower than normal-diet shifted mice, and high fat diet shifted mice scored higher than normal-diet shifted mice. High fat diet shifted mice showed proteoglycan loss and pathological changes in several joints, including the lumbar spine and glenohumeral joint; but non-shifted high fat diet mice did not show changes in joints other than the knee.
In addition to proteoglycan loss, shifted mice had significant disruptions in cartilage homeostasis. This was seen as a reduction in chondroprotective enzymes; as well as abnormally increased levels of chondrocyte hypertrophy markers and matrix degrading enzymes, which were even more elevated in the high fat shifted group. These changes cause a faster breakdown of joint cartilage, without sufficient growth of replacement cartilage.
Taken together these findings show that a shifted circadian rhythm speeds joint degradation and when coupled with a secondary stressor, such as a high fat diet, the effects can be even more profound. The high fat diet as a stressor is particularly important due to the increased preference of high fat foods in animals with a disrupted circadian rhythm, as both conditions are likely to appear together.
Diabetes
Conclusion
Bibliography
Cain, S.W., Filtness, A.J., Phillips, C.L., Anderson, C., 2015. Enhanced preference for high-fat foods following a simulated night shift. Scand. J. Work. Environ. Health 41, 288–293. https://doi.org/10.5271/sjweh.3486
Chen, Z., 2019. Temporal Control of Appetite by AgRP Clocks. Cell Metab. 29, 1022–1023. https://doi.org/10.1016/j.cmet.2019.04.009
Garbazza, C., Bromundt, V., Eckert, A., Brunner, D.P., Meier, F., Hackethal, S., Cajochen, C., 2016. Non-24-Hour Sleep-Wake Disorder Revisited – A Case Study. Front. Neurol. 7. https://doi.org/10.3389/fneur.2016.00017
Hopkins, M., Blundell, J., Halford, J., King, N., Finlayson, G., 2000. The Regulation of Food Intake in Humans, in: Feingold, K.R., Anawalt, B., Boyce, A., Chrousos, G., Dungan, K., Grossman, A., Hershman, J.M., Kaltsas, G., Koch, C., Kopp, P., Korbonits, M., McLachlan, R., Morley, J.E., New, M., Perreault, L., Purnell, J., Rebar, R., Singer, F., Trence, D.L., Vinik, A., Wilson, D.P. (Eds.), Endotext. MDText.com, Inc., South Dartmouth (MA).
Kc, R., Li, X., Forsyth, C.B., Voigt, R.M., Summa, K.C., Vitaterna, M.H., Tryniszewska, B., Keshavarzian, A., Turek, F.W., Meng, Q.-J., Im, H.-J., 2015. Osteoarthritis-like pathologic changes in the knee joint induced by environmental disruption of circadian rhythms is potentiated by a high-fat diet. Sci. Rep. 5, 1–7. https://doi.org/10.1038/srep16896
Klok, M.D., Jakobsdottir, S., Drent, M.L., 2007. The role of leptin and ghrelin in the regulation of food intake and body weight in humans: a review. Obes. Rev. Off. J. Int. Assoc. Study Obes. 8, 21–34. https://doi.org/10.1111/j.1467-789X.2006.00270.x
Kus, I., Sarsilmaz, M., Colakoglu, N., Kukne, A., Ozen, O.A., Yilmaz, B., Kelestimur, H., 2004. Pinealectomy increases and exogenous melatonin decreases leptin production in rat anterior pituitary cells: an immunohistochemical study. Physiol. Res. 53, 403–408.
Starling, S., 2019. Neuronal clock coordinates appetite. Nat. Rev. Endocrinol. 15, 253–253. https://doi.org/10.1038/s41574-019-0196-4
Summa, K.C., Voigt, R.M., Forsyth, C.B., Shaikh, M., Cavanaugh, K., Tang, Y., Vitaterna, M.H., Song, S., Turek, F.W., Keshavarzian, A., 2013. Disruption of the Circadian Clock in Mice Increases Intestinal Permeability and Promotes Alcohol-Induced Hepatic Pathology and Inflammation. PLoS ONE 8. https://doi.org/10.1371/journal.pone.0067102