Long-term effects of different diets on the central nervous system
Introduction
The food we consume does not only provide our body with the necessary energy for anabolic processes and to perform daily tasks. Its nutritious factors have complex biochemical interactions with the molecular mechanisms in each cell, tissue and organ. The central nervous system is strongly affected by diet. The lack or abundance of certain nutrients can alter cognition, and cause or worsen neurological disorders. Most importantly, certain diets can improve brain health and prevent the development of neurological disorders.
We will discuss common diets such as the Standard American (Western) diet, the Mediterranean diet, the Plant-Based diet and the Pescatarian diet, as well as less widespread diets, such as the Ketogenic and Palaeolithic diets.
Standard American Diet
The standard American diet (SAD) is high in refined carbohydrates/sugars and animal-based products such as meats, dairy and eggs. It lacks in whole grains, fruits and vegetables while being high in saturated fat, processed/convenience foods and sodium (Grotto and Zied, 2010). The diet is also high in omega-6 fatty acids and low in omega-3 fatty acids. (Cordain et al, 2005). SADs are correlated to obesity, diabetes type II and hypercholesterolemia (Okręglicka, 2015).
The SAD has been linked to changes in appetite and behaviour. High-calorie foods induce behavioural changes due to the release of dopamine upon consumption. As dopamine is a “feel good” neurotransmitter this can cause addiction-like behaviour and affect the hippocampus and the hypothalamus which have roles in memory and food intake. Once these foods are not consumed, the individual may experience changes in their dopamine levels, receptors, mood and the dopamine-mediated reward system (Johnson and Kenny, 2010; Edward et al, 2011; Reichelt and Rank, 2017).
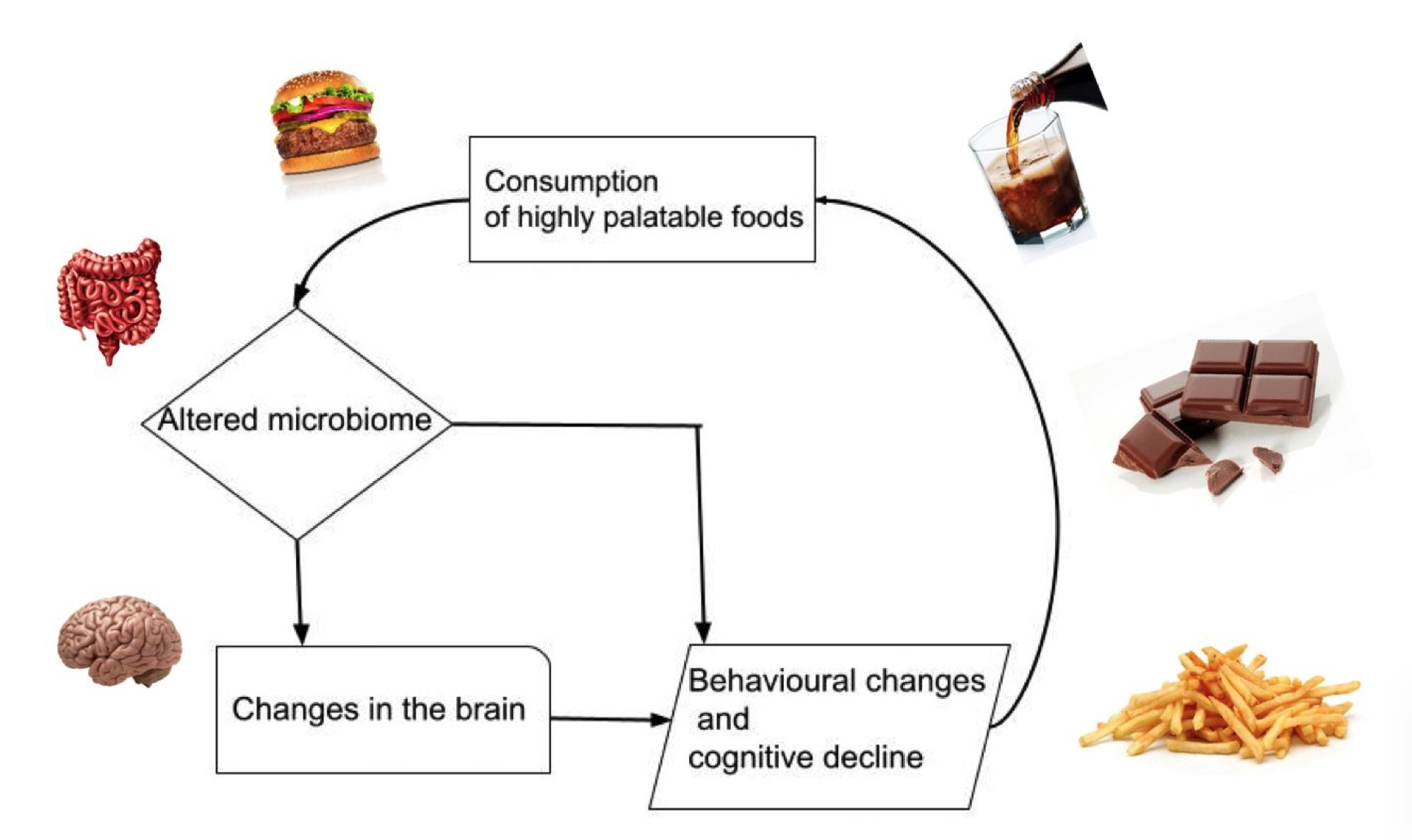
The disturbance of the hypothalamus due to the SAD causes increased appetite (Kanoski et al, 2010; Stevenson et al, 2020). This cycle repeats leading to decreased cognition and a further increase in food intake (Kanoski and Davidson, 2011), as shown in figure 1.
|
Figure 1 The Cycle of Overconsumption of Highly Palatable Foods and the Effects on the Brain. |
The high sugar and fat intake of the SAD also alters memory and contributes to the progression of some neurological disorders. People consuming the SAD are shown to have smaller hippocampi (Jacka et al, 2015), causing changes in memory (Ke et al, 2020). The negative effects on memory can occur even after short-term SAD consumption with participants fed a SAD performing worse in memory tasks compared to control groups (Francis and Stevenson, 2011).
SAD-associated conditions such as diabetes type II and hypercholesterolemia are linked with cognitive decline and brain disorders such as Alzheimer's disease (AD) (Xue-shan et al, 2016; Guo et al, 2016). Thus, AD may be improved with insulin treatment (Hölscher, 2020). Furthermore, lower consumption of high-fat dairy products and meat showed a lower risk of AD (Gu et al, 2010). As more countries adopt a more westernised diet they have seen increases in AD and dementia (Grant, 2014), showing the direct correlation between AD and the SAD.
Attention is also significantly impaired in those individuals on the SAD. Consumption of a high-fat diet leads to increased simple reaction time and decreased attention in study participants (Edwards et al, 2011) and is associated with a higher prevalence of attention deficit hyperactivity disorder (Howard et al, 2011).
Other overall harmful effects of SAD on the CNS include neuroinflammation, brain tissue damage (Pistell et al, 2010) and which may explain why individuals on the SAD experienced prolonged recovery, after traumatic brain injuries (Wu et al, 2003).
Mediterranean diet
The Mediterranean diet (MD) is a traditional diet high in unprocessed plants (grains, vegetables, fruits, legumes, nuts, and seeds), moderate in seafood, and low in animal-based foods and discretionary foods. Extra virgin olive oil and red wine consumption are also characteristic (Radd-Vagenas et al, 2018).
MD has been suggested to reduce systemic inflammation and improve metabolism, which could improve symptoms of Alzheimer’s Disease. MD displays anti-inflammatory, antioxidant, and beneficial microbiome effects which can reduce cognitive decline and improve various neurological functions, such as memory and learning (Radd-Vagenas et al, 2018). Restoring glucose metabolism by reducing plasma glucose levels can reduce the risk for Alzheimer’s Disease and improve cognitive function during ageing (Huhn et al, 2015; Radd-Vagenas et al, 2018). Furthermore, MD can have favourable effects on lipid metabolism, including reducing plasma LDL, and VLDL, and increasing HDL levels. These effects can decrease the risk of strokes (Demarin et al, 2011).
Higher adherence to MD relates to larger grey matter volume, cortex thickness and total brain volume (Gu et al, 2015). Additionally, it decreases amyloidosis and tau pathology, both of which are involved in many neurodegenerative diseases (Ballarini et al, 2021). An improvement in Parkinson's patients was observed, where mean scores of executive function, language, attention, concentration, and memory were higher than in the control group (Paknahad et al, 2020).
The MD ensures the intake of a large range of vitamins and minerals through vegetables, beans, grains, and fruits that nourish the nervous system. Antioxidant properties can be found in phenols, vitamin C, vitamin E, and carotenoids, while vitamin C is especially neuroprotective by eliminating reactive oxygen species and controlling neuroinflammation (Gu et al, 2010; Siervo et al, 2011).
Omega-3 fatty acids (such as DHA) derived from fish have been correlated to improved learning and memory in rodents. It also affects neuronal differentiation and synaptogenesis in the brain. Fish and cereals may reduce the prevalence of Alzheimer’s Disease in the elderly (Panza et al, 2004). Red wine and fruits contain plant polyphenols which act as antioxidants leading to enhanced cognition and reduced risk of age-related cognitive decline. Further neuroprotective properties of polyphenols include decreased mitochondrial dysfunction, hyperglycaemia, and chronic inflammation (Huhn et al, 2015). Potent antioxidants (such as catalase) and oleocanthal (ibuprofen-like compound) can also be found in freshly produced extra virgin olive oil which reduce brain inflammation (Siervo et al, 2011). A French cohort consuming three to four glasses of red wine per day showed lower risks of Alzheimer’s disease compared to non-alcohol drinkers (Panza et al, 2004).
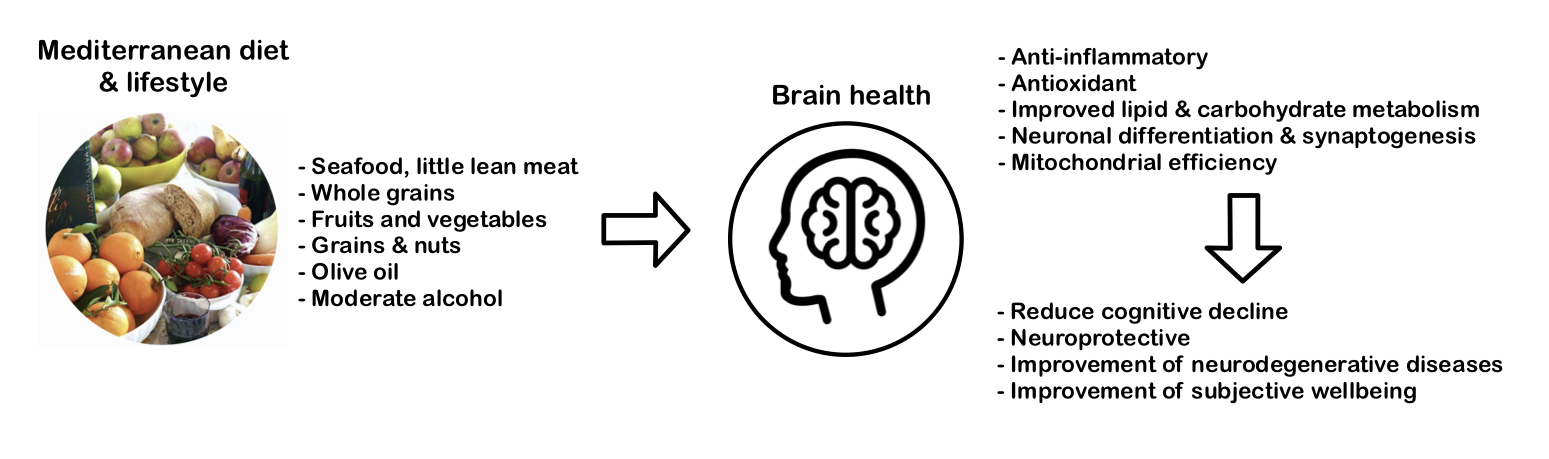
Stand-alone research found that adolescents adhering to MD had higher academic performance (maths, language, GPA) compared to the poor adherence group (Esteban-Cornejo, 2016). Another study with adolescents was conducted using the “Subjective happiness and health-related quality of life” (HRQOL) scores. They found that high adherence to MD was associated with higher scores in areas such as psychological well-being and better mood (Ferrer-Cascales et al, 2019). The figure 2 below demonstrates the composition and effects of MD on the brain.
|
Figure 2 The Components of a Mediterranean Diet, its Neurological Effects and Benefits. |
Most studies have pointed out that clinical trials suffer from inconsistent results due to differences in diet. Most results also rely on animal experiments instead of clinical observations (Féart et al, 2013; Huhn et al, 2015; Siervo et al, 2021). Crichton et al (2013) were one of the research groups that found no correlation between MD and higher cognitive function. A reason could be that MD is less of a diet and more of a culture that includes healthy habits, lifestyle, and social factors. This was shown by the association between MD and overall mental health in a community in Croatia (Andrade et al, 2020).
Plant-Based (Vegetarian and Vegan) diet
The Plant-Based Diet (PBD) is a diet that excludes meat. Veganism, vegetarian, lacto-vegetarianism, and lacto-ovo-vegetarianism are versions of this diet. Fruit, vegetables, legumes, nuts, grains, and soy are typically dominant in this diet (McEvoy et al, 2012).
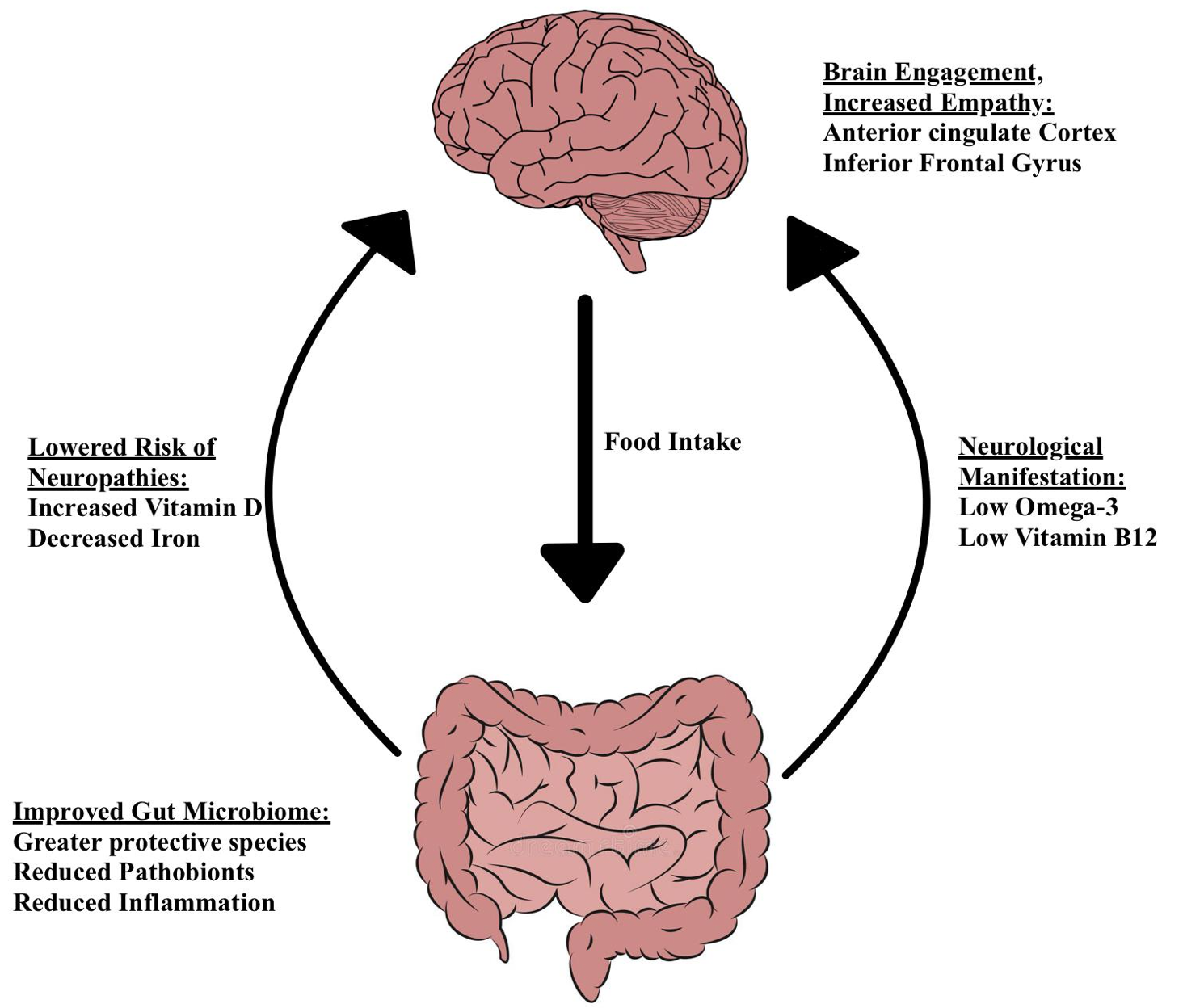
The structure and activity of bacteria in the human gut are influenced by long-term nutrition (David et al, 2013). PBD causes a major shift in the microbiota composition (Zimmer and colleagues, 2011). The gut profiles of PBD show fewer pathogens, more defensive species, and less inflammation (Yeh and Glick-Bauer, 2014). Changes in the gut-brain axis mediate pathogenesis and pathophysiology of psychiatric and neurologic pathologies (Martin et al, 2018), as shown in figure 3.
Individuals on a PBD are at high-risk for vitamin B12 deficiency. The degenerative abnormalities in the CNS are responsible for the neurological signs of vitamin B12 deficiency (Kapoor et al, 2017). PBD causes decreased iron reserves (McEvoy et al, 2012). This can be beneficial since increased iron concentrations have been linked to neuropathologies like Alzheimer's, Parkinson's, and multiple sclerosis (Ward et al, 2014).
Vitamin D deficiency is more common in strict PBD, especially those who live in northern latitudes (McEvoy et al, 2012). Vitamin D deficiency is linked to neurological illnesses (Moretti et al, 2018).
PBD may have fewer Omega-3 fatty acids (N-3) and more Omega-6 fatty acids (N-6) than meat-based diets (McEvoy et al, 2012). Low N-3 levels compared to N-6 levels are linked to a higher risk of suicide attempts and suicide (Liu et al., 2015) (Sublette et al, 2006). Sufficient N-3 can be obtained from plant sources, such as algae, however, most people consume an abundance of N-6 containing foods (Doughman et al, 2007). Thus, it is not necessarily the lack of N-3 that poses a threat to health, but rather the imbalance in the N-3:N-6 ratio (Liu et al, 2015).
Vegetarians and vegans, regardless of species, engage more empathy-related regions (anterior cingulate brain and inferior frontal gyrus) when seeing distressing scenarios (Filippi et al., 2010).
PBD can cause neuropathies, although these can be easily mitigated with the right supplementation. Those who followed a nutritious PBD had a lower incidence of total stroke (Baden et al, 2021). Medawar et al. (2019) conducted a systematic evaluation of clinical studies and found evidence supporting the health and disease benefits of a PBD. More research is needed to better understand mental and cognitive consequences of PBD.
|
Figure 3 The Neurological Effects of a Plant Based Diet on the Gut-Brain Axis. |
Pescatarian diet
The pescatarian diet resembles the vegetarian diet however, it incorporates seafood. Fish meat contains two polyunsaturated omega 3 fatty acid: eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).
EPA and DHA are essential components of membranes in the body, including membranes of human neurons (Valentine and Valentine, 2004). They, therefore, have an important role in neuronal function.
It is important to note that EPA and DHA may be synthesised from alpha-linolenic acid acquired from non-fish food sources. However, this is not very efficient and relying on this may lead to a deficiency of these fatty acids (Gerster, 1998).
DHA and EPA are essential in the development and function of the brain. Women who were supplemented with fish oil during pregnancy were shown to have children with better cognitive skills (Judge et al, 2007; Helland et al, 2003) and hand-eye coordination (Dunstan et al, 2006) when compared to control groups.
Due to DHA and EPA making up a large amount of the neuron membrane phospholipids, they have been linked with neurological and cognitive disorders such as Alzheimer’s disease (AD). Patients with AD were shown to have had lower levels of omega-3 fatty acids in the blood than those without the disease (Tully et al, 2003). Similarly, Gu et al (2010) found that diets high in DHA and EPA were inversely correlated to the risk of AD. Other studies that supplemented patients with fish oil as a treatment showed potentially promising results in mild cases of AD. Cases of moderate to severe AD did not show significant improvement when compared to the control group (Freund-Levi et al, 2006).
Studies in both rats (Naliwaiko et al, 2004) and humans (Mocking et al, 2016) used omega-3 fatty acids as a treatment for depression. The combination of EPA with antidepressants has been shown to aid in depression treatment. (Mocking et al, 2016).
Zanarini and Frankenburg (2003) found that EPA may be an effective treatment for borderline personality disorder while Montgomery and Richardson (2008) found it reduced depressive symptoms in bipolar patients however both studies contained a small sample size.
Due to the exclusion of meat in this diet, from a neurological view, the pescatarian diet has all the benefits of a vegetarian diet with additional benefits of higher amounts of EHA and DHA. The findings of the studies above are demonstrated in figure 4.