|
Size: 30560
Comment:
|
Size: 30671
Comment:
|
| Deletions are marked like this. | Additions are marked like this. |
| Line 5: | Line 5: |
''Cormac Timothy Kiely and Sigridur Audna Gudgeirsdottir Hjardar'' ''Supervisor: Dr Jócsák Gergely'' |
Itt írjon a(z) Microbiome_CNS-ról/ről
Microbiome and The Central Nervous System
Cormac Timothy Kiely and Sigridur Audna Gudgeirsdottir Hjardar Supervisor: Dr Jócsák Gergely
Contents
Introduction
The mammalian body is a complex physiological system with many intertwining pathways. The nervous system, in particular, intersects with most of the other functions and oversees many of the mechanisms that maintain homeostasis. The endocrine and immune systems are two that have the most interactions with the nervous system however, this article will investigate the interactions between the nervous system and the microbiome of gut flora that reside within the digestive system.
We will first analyse the influence certain species of certain bacteria have on the ability of the organism to respond to stressful situations; their ability to form and retain certain memories; and their ability to manage long term anxiety and general mental wellbeing.
Following this, we will then focus our attention to certain pathological diseases within the nervous system and investigate whether gut flora can help alleviate the symptoms. The pathologies we investigated were: Strokes and Alzheimer’s Disease.
With all of the above investigated topics, we will break this article into two parts: the interactions with physiology, and the influence on pathological diseases. We will give a brief description of the physiological pathways and try to aid the reader in their understanding of the mechanisms involved. In the pathological chapters, we will also explain the negative changes of the physiology caused by the particular diseases. This will also help the reader to visualise the effects the gut flora has on these pathways.
In the research we conducted, two genera of bacteria stood out: Bifidobacteria spp. and Lactobacillus spp. In the first section, some of the trials that utilised these species of bacteria showed very promising results for the wellbeing of the animal’s mental health.
In short, what we discovered from both parts was that the microbiome has indisputable effects on the nervous system. Some were positive: B. longum, B. breve, Lactobacillus spp. and some were negative: Enterobacteria spp. and H. pylori. What cannot be stressed enough is the variety of responses experienced in the physiology of the animal, suggesting that all these effects are strain dependent.
Commensal gut microbiota has been referred to as a crucial part in modulating the gut-brain axis, through various pathways. They lead to an increase in interest in modulating the gut microbiota to target CNS functions, especially in areas like stress, anxiety, mood and cognition. Moreover, many preclinical studies have shown that probiotics that act through the gut-brain axis can affect brain development, function and behavior.
PART ONE: PHYSIOLOGICAL INTERACTIONS
Stress Management
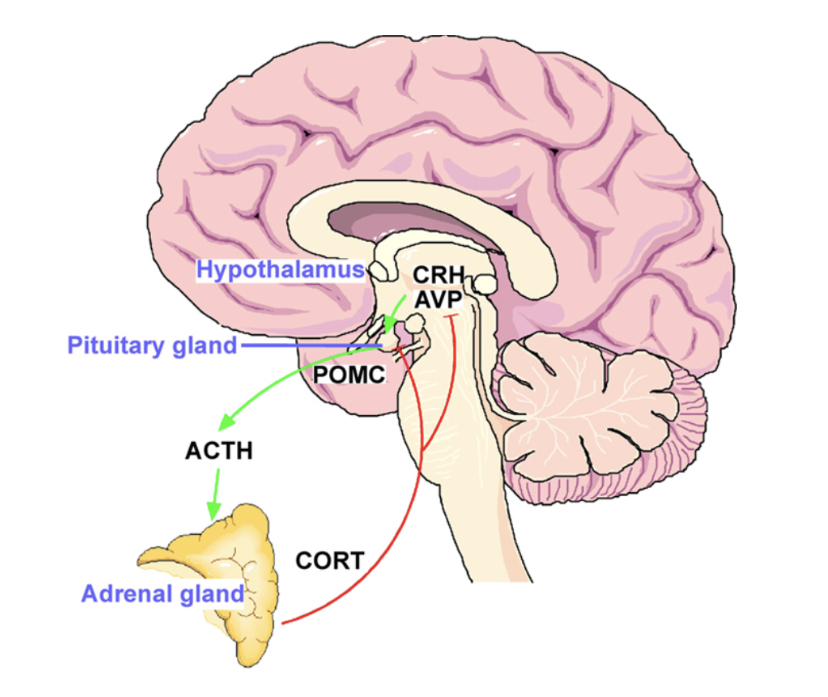
Stress can materialise in many ways and can evoke a response within the organism that is either specific i.e. antibody-antigen complex, or non-specific. The latter usually causes the same physiological response within the organism. On top of the Catecholamines (Epinephrine, Norepinephrine) being immediately released from the adrenal medulla, there are also factors that have a more long lasting effect on the body. Adrenocorticotropic Hormone (ACTH) is released from the adenohypophysis in response to the stimuli and will activate the G-Protein mediated adenylate cyclase pathway for the activation of Protein Kinase A (PKA) in the adrenal cortex. This PKA will then mobilise the cascade of enzymatic reactions that result in the synthesis and release of Glucocorticoids, specifically Cortisol and Corticosterone. This pathway is illustrated in Fig. 1: HPA axis.
|
Figure 1: Hypothalamo-Pituitary-Adrenal (HPA) Axis |
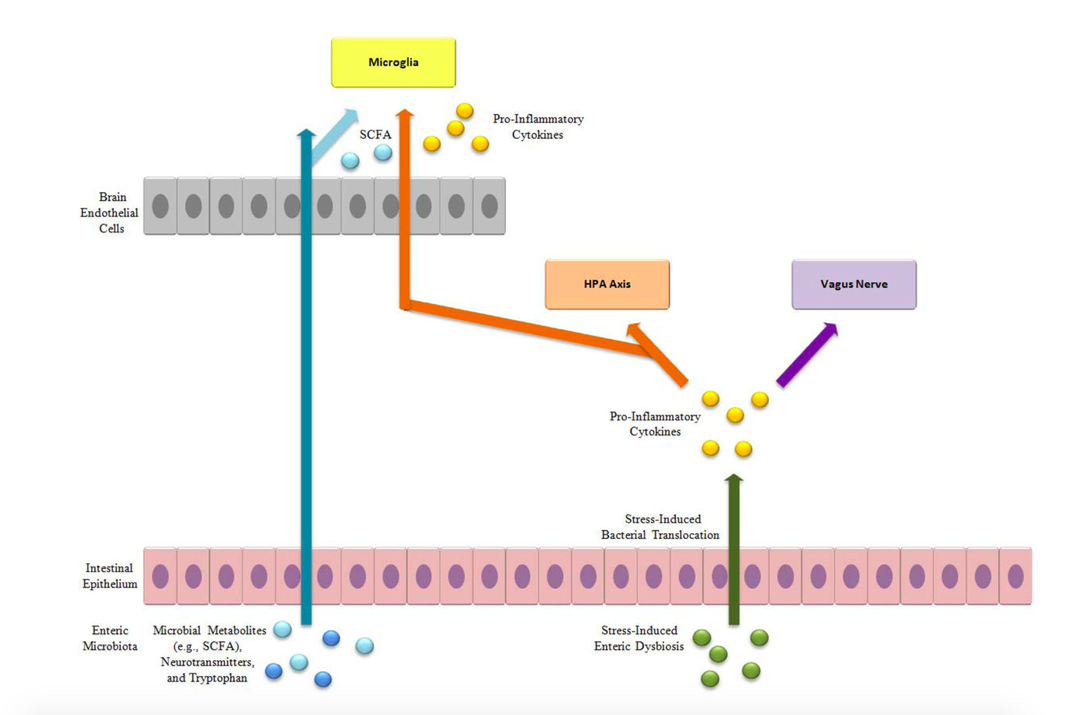
Furthermore, Savignac et al (2014) have stated that the spectrum of bacterial flora in the gut, henceforth referred to as microbiome, is a major contributor to the manifestation of stress and psychiatric disorders. This is a direct consequence of the gut-brain axis and illustrates that the physiological systems are far from being isolated entities. We can see from Fig. 2 how this mechanism of interaction takes place. Moreover, their study has shown how the stress brought on by this axis or otherwise can be controlled with different genera of bacteria; in particular Bifidobacteria longum and B. breve.
|
Figure 2: Gut-Brain Axis |
Controlling this ability, the use of probiotics in the treatment of mental disorders carries major potential in the area of mental health. Moreover, Savignac et al (2014) continue by saying that members of the Lactobacillus family have shown evidence of normalizing the levels of gluccorticoids in the blood, specifically corticosterone.
It must be stressed however, that the mechanisms behind this control is poorly understood and is therefore educated speculation that requires more research. In the above study (Savignac et al, 2014), it was emphasized that there is a strong and complex interaction between the microbiome, the gut epithelial cells and the immune system of the host; this interaction will then influence the gut-brain axis. Altering this community with exogenous bacteria such as B. longum will cause a response in favor of stress management. This particular species has a fermentation product that inhibits the firing of the enteric nerves and thus communication with the CNS.
It was speculated that the afferent fibers of the N. Vagus (X) are the major connection between the enteric mucosa and the CNS. As the nucleus of the Vagus nerve is located within the brain stem, its effect on the associated structures is plausible. Therefore, it can be expected that it is also involved in anxiety levels and that this activity of the host is influenced by gut bacteria, either infectious or symbiotic.
Further study showed that the strains of B. longum and B. breve had different effects on the CNS, suggesting that these results are strain specific. Activation of the immune system in the periphery will induce a specific cytokine release into the blood plasma and thus different strains of bacteria may evoke a specific response in the brain via hormonal or neural pathways.
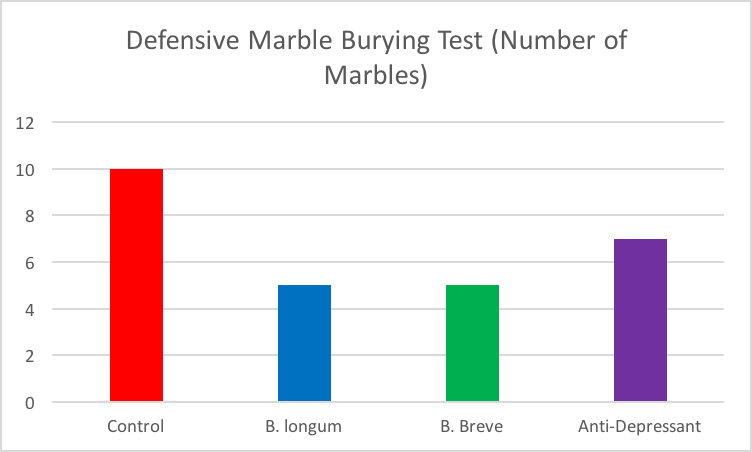
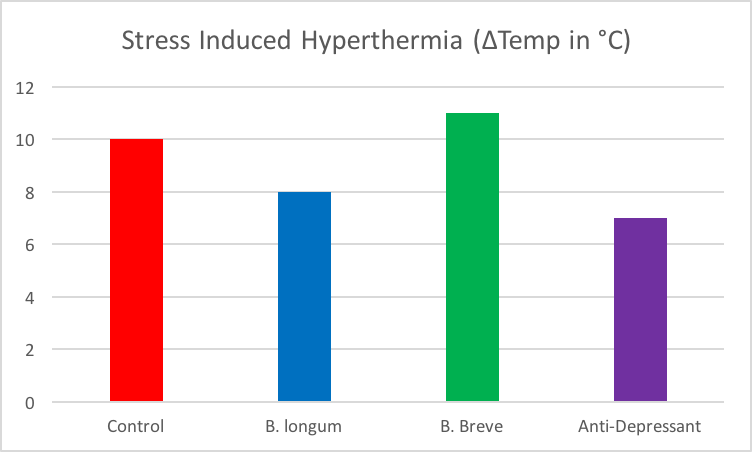
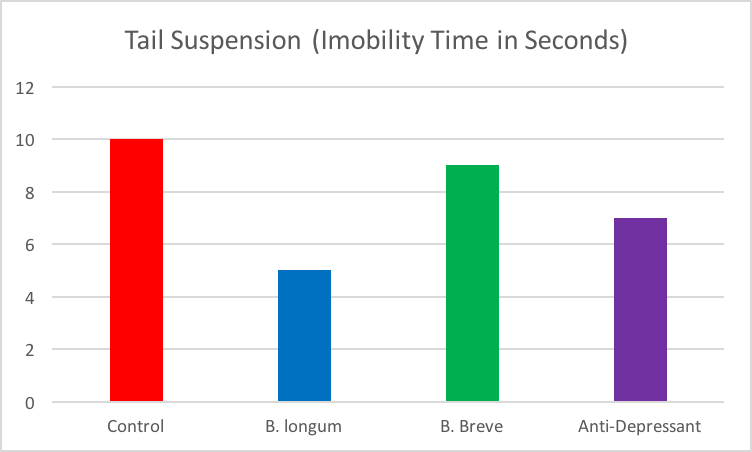
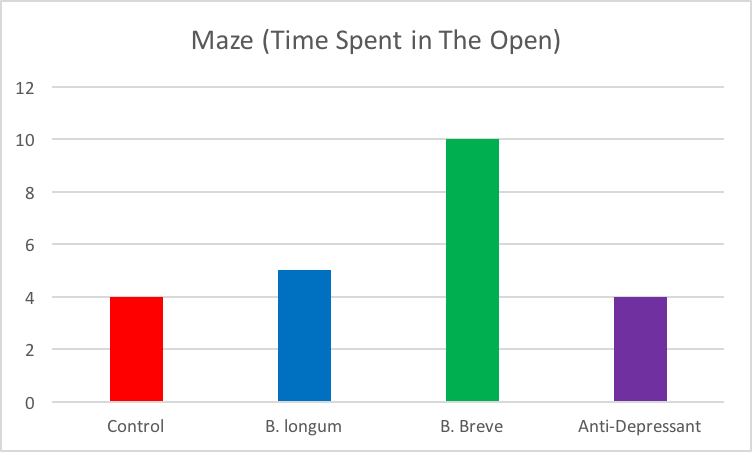
In the study, the subjects (mice) were subjected to stressful stimuli involved with different conditions (suspension by tail, hyperthermia, mazes, marble burying) and their behavior analysed. Treatments to test were the two Bifidobacteria strains, an anti-depressant, and a control. Results show that both B. longum and B. breve were able to reduce anxiety in the marble burying test (Fig. 3), however only B. longum showed a decrease in stress from hyperthermia (Fig. 4) and the tail suspension (Fig. 5) and B. breve showed a reduction in stress and anxiety in the maze (Fig. 6).
|
Figure 3: Marble Burying Test |
Fig. 3 Explanation: Less marbles burried indicated lower stress levels. Source of data: Savignac et al, 2014. Adapted for simplicity.
|
Figure 4: Hyperthermia |
Fig. 4 Explanation: Lower temperature changes indicates lower stress levels. Source of data: Savignac et al, 2014. Adapted for simplicity.
|
Figure 5: Tail Suspension Test |
Fig. 5 Explanation: Lower time spent immobile indicates lower stress levels. Source of data: Savignac et al, 2014. Adapted for simplicity.
|
Figure 6: Maze Test |
Fig. 6 Explanation: More time spent in the open indicates lower stress levels. Source of data: Savignac et al, 2014. Adapted for simplicity.
In 2019, the same bacterial strains were used for human evaluation. These studies have shown that the probiotic strain, B. longum, reduces stress-related behaviors, improves stress responses and also improves cognitive function in healthy individuals.
When investigating the effect of B. longum (Wang et al, 2019) on brain function when responding to social stress, magnetoencephalography (MEG) can be used to measure the response. Social stress is induced and during the stressor, there are alterations in neural oscillations on certain brain areas, e.g. alpha band power in frontal cortex and theta band power in the anterior cingulate cortex and insula.
The induction of stress can be done with standardized “Cyberball game” which involves inclusion and exclusion. After the game, the participants were to answer three questionnaires in order to evaluate the level of acute stress. • The Need Threat Scale - it is designed to measure the feelings and emotional consequences of social rejection, • The Mood Questionnaire - used to evaluate mood through eight questions and • The Subjective “Exclusion Perception” - it is used to record participants’ feeling of being included or excluded.
The intervention went on for four weeks where two groups were compared through the experiment, one group was given B. longum and the other group was given the placebo. There was an interesting contrast which showed the treatment group (B. longum) had increased theta band power (Learning, memory and intuition) and alpha band power (Relaxation), with reduced beta-2 power (Anxiety) when compared with the control (placebo) group.
The data from the study suggests that the probiotic strain might be modulating relevant processes for managing stress responses. The increase and decrease in band powers was associated with increase in perceived vitality levels, which was assessed with SF36 (36-item short-form health survey that each participant answered), suggesting that the probiotic strain alters neural activities with enhanced vitality and reduced mental fatigue. It reduced participants’ stress response and they were able to manage the increased distress level by “up-regulating” processes that evaluate stressful events and “down-regulating” negative emotions.
B. longum has shown anti-stress and precognitive effects in healthy mice and it can also improve the physiological and psychological response to an acute stressor in healthy human adults (Allen et al, 2016)
The Paired Associate Learning test (PAL) performance is dependent upon the hippocampus, which has a high proportion of receptors for glucocorticoids, and PAL performance is poorer in subjects with stress-related disorders with associated hypothalamic-pituitary-adrenal axis dysfunction, such as Irritable Bowel Syndrome (IBS). The PAL performance can be slightly improved by the strain (Allen et al, 2016).
Cognition
The role of bacterial strains and the microbiome-brain axis on cognition is largely unexplored according to Savignac et al (2015). The two main strains mentioned above, B. longum and B. breve, were investigated in the area of cognition, already knowing their effects on stress and anxiety from a previous study. This may suggest some degree of relationship between stress and cognitive functions.
The main anatomical centers for learning are the Amygdala and the Hippocampus in the Limbic System and the Prefrontal Cortex of the brain. These structures are important for the expression of emotion and since the Rhinencephalon (center of olfaction) is in close proximity and in direct connection to the Limbic System, the triggering of certain memories is aided by certain odors. This type of memory is an evolutionary memory for aggression, fear and sexual behavior triggered by distinct pheromones. It also helps with the spatial awareness and helps the animal to adapt to their surroundings by retrieving long term memories that were stored.
Creating memories firstly involves a stimulus to create awareness and repetition of this stimulus in the immediate or short term memory will allow the transfer into long term memory. This repetition will “restructure” the brain by increasing the amount of post-synaptic receptors: the NMDA-linked cation receptors are released from the magnesium inhibition. This gives that particular pathway more plasticity and the memory will be retrieved more easily; this is known as Long-Term Potentiation.
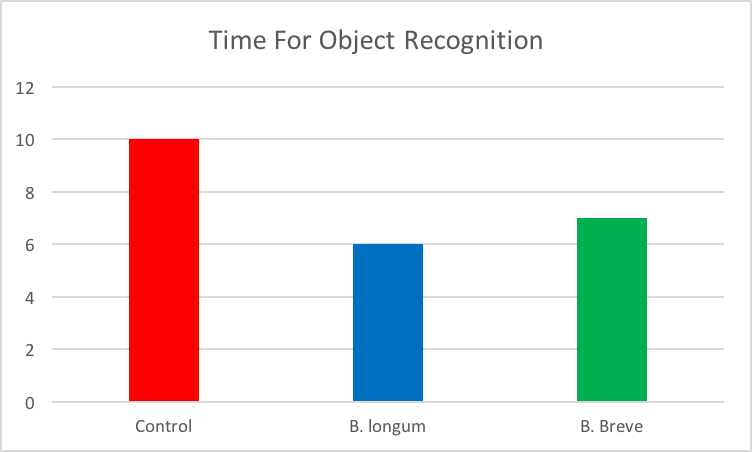
Savignac et al (2015) were able to show that the B. longum and the B. breve fed mice showed an increase in their ability to discriminate between objects, with the greater effect shown in the former species. This is shown clearly in Fig. 7, whereby the shorter time determines faster learning. Similarly, the mice made fewer errors in a Barnes maze. These two tests of cognition showed a high degree of influence from the bacteria on the mice’s learning abilities.
|
Figure 7: Object Recognition |
Fig. 7 Explanation: Less time spent sniffing indicates faster learning. Source of data: Savignac et al, 2015. Adapted for simplicity.
The mechanisms at work were only hypothesized and the requirement for further neurobiological and biochemical research is required. As mentioned before, certain strains of bacteria have specific cytokine stimulation within the immune system. They speculated whether this immune response was transpired to the microglia and a consequential restructuring of the nucleus accumbens of the Hippocampus which also reduced amygdala inhibition of the hippocampus and prefrontal cortex, resulting in an improved learning ability. Furthermore, it was also speculated whether the signal originated via the enterochromaffin cells, which contain a large reserve of Serotonin and Glutamate (as well as GABA and Ach) in which the former is involved in serotonergic facilitating interneurons and the latter directly in the long term potentiation of memories.
Anxiety and Mental Health
Preclinical research (Allen et al, 2016) have showed that administering probiotic for longer time can reduce behavior that indicates anxiety and depression. It can even normalize associated physiological outputs, for example corticosterone, norepinephrine, brain-derived neurotrophic factor and immune function. Most of the studies have been done on animals but specific probiotic strains have shown potential in altering hypothalamic-pituitary-adrenal axis activity and cognition.
However, studies on healthy human volunteers have shown that multistrain probiotics, fermented drinks containing probiotics or prebiotics can alter resting brain activity, cognitive performance, baseline physiological stress outputs and self-reported physiological variables. In one particular study (Allen et al, 2016), The Socially Evaluated Cold Pressor Test (SECPT) was used as a combined psychological and physiological stressor procedure, which doesn’t induce hypothalamic-pituitary-adrenal axis habituations across repeated exposures.
The stressor increased salivary cortisol significantly. Following psychobiotic intervention, cortisol output during the test was lower and the increase in self-reported anxiety was no longer significant. Overall stress, as measured by areas under the curve for glucose (AUCg), was significantly lower, while using B. longum when compared to the placebo group. Stress induced Glucocorticoid release has a mobilizing effect on Glucose metabolism, specifically stimulation of hepatic gluconeogenesis.
PART TWO: INFLUENCE ON PATHOLOGICAL DISEASES
Strokes
With age, the risk of ischemic stroke is said to significantly increase. Gastrointestinal complications are proportionately common with stroke patients and recent research assume that the “brain-gut axis” plays a role in these complications (Tan et al, 2019). The axis seems to be influenced by gut microbiota dysbiosis (disturbance in the microbiome structure) and other complications, e.g. dysphagia and constipation.
The gut-brain axis (GBA) consists of a two-way communication network between the gastrointestinal tract and the brain. This network links together the central cognitive and emotive centers of the brain with the peripheral intestines and their processes. The axis helps to regulate homeostasis, inflammation and the immune responses. These balances are adjusted by signaling pathways, involving the central, autonomic and also enteric nervous systems alongside with the hypothalamic-pituitary-adrenal axis.
Trimethylamine N-oxide (TMAO) is a metabolite of the gut flora and it is the most well-studied connection between gut flora and stroke risk. Studies have shown (Tan et al, 2019) that the production of TMAO from dietary phosphatidylcholine is dependent on metabolism by the intestinal microbiota. Elevated TMAO levels have been associated with an increased risk of major cardiovascular events, e.g. stroke.
The mechanism about how TMAO elevates cardiovascular risk isn’t well understood. However, one suggested mechanism is the TMAO-mediated increase of pro-inflammatory monocytes and vascular inflammation, where increased TMAO levels demonstrate a dose-dependent association with the risk of repetition of a stroke. Plasma TMAO levels have also been connected with other risk factors of ischemic stroke, e.g. diabetes mellitus, which can, on their own, increase stroke risk.
There have also been studies that explore the mechanisms that changes the gut flora and how it affects poststroke neuroinflammation and the impacts this has on the outcome of the stroke. In a study with mice (Tan et al, 2019), microbiota from post-stroke mice was transplanted into germ-free mice. In the recipient mice, cortical strokes were induced and the study showed that the mice that received the microbiota from post-stroke mice had significantly larger infarct volumes compared to placebo transplant mice. The first group also had higher expression of inflammatory T-cells, Th1 (Host defense against intracellular pathogens) and Th17 (Host defense against extracellular pathogens). When investigated further, fluorescent-labeled immune tissue was used, and it revealed that the T-cells from the post-stroke mice microbiota had migrated to the brain few days after the stroke, causing grievous neurological injury.
Tan et al (2019) researched another study on mice, broad-spectrum antibiotics was used to alter the intestinal microbe diversity before stroke. It indicated that the antibiotics had anti-inflammatory neuroprotective effect and decreased infarct volume of the affected mice by 60% and preserved the sensorimotor function. The antibiotic use caused an intestinal dysbiosis and adjustments of the neuroinflammatory response after stroke by T-cell mediated mechanisms.
Gut microbiota and its relation to stroke pathogenesis has been researched and the outcomes could be the start of therapeutic target. Previous studies have suggested that the development of powerful inhibitors of gut-microbiota-dependent TMAO generation, could be able to decrease thromboses and risk of stroke.
Tan et al (2019) continued their research into this area: Animal experiments show that fecal transplantation and colonization with normal stool microbiota can improve stroke outcome. Probiotics are capable of altering the gut flora, adjust cytokine release, have an impact on neuroinflammatory response, and with these influences, be a therapeutic strategy for acute stroke. Another animal study did suggest that treatment with the probiotic Clostridium butyricum reduced cerebral ischemia injury in mice.
Research on the interaction between gut flora and central nervous system, both with health and diseases, has been showing an increase in interest and more focus is being put into them. It has showed that gastrointestinal complications are common in patients after stroke. Gut microbiota alterations, with expression and suppression of many biomarkers, are starting to undergo extensive evaluation. However, it must be taken into consideration that the understanding that is known about the GBA and its relations to stroke, come from animal studies, even though human studies are becoming more frequent in this field to gain more understanding.
Alzheimer’s Disease
This neurodegenerative disease mainly affects the patient’s ability to retrieve long term memories rather than destroying the part of the brain where they are stored. Therefore, it is speculated that a reduced efficiency in the synaptic connection is most likely.
The disease is characterised by an accumulation of amyloid in the brain, partnered with a defected tau protein (Pluta et al, 2020). Amyloid is converted to beta-amyloid peptide in the brain and the monomer will create fibrils and plaques (Kumar et al, 2016). This fibrillation is the major driver of the onset of Alzheimer’s disease. Moreover, tau proteins are part of the brain’s normal physiology and bind to the microtubules in the nerve and glial cells for efficiency. However, dysfunctional tau proteins dissociate from the microtubules and form agglutinating fibril networks (Uddin, 2020).
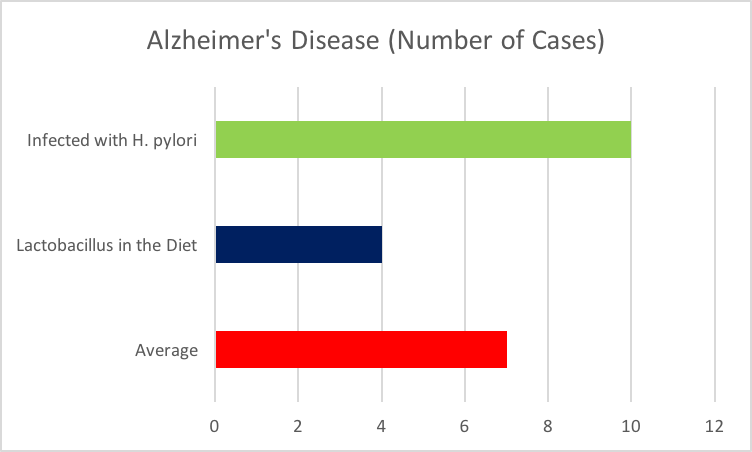
As shown by Ozawa et al (2014) (cited by Pluta et al, 2020), the cases of confirmed Alzheimer’s Disease was greatly reduced in those patients who consumed more dairy products. This opens the realm of the association of certain microbes on the development of this disease. Moreover, Heliobacter pylori, an infectious bacteria, was demonstrated as having a positive proportion in the number of cases (Roubaud-Baudron et al, 2012). These trends, both positive and negative, are illustrated in Fig. 8. This expands on the idea that certain strains can influence the response that occurs in the brain. The latter case may also propose that an inflammatory response is the causative reaction that accelerated the development of Alzheimer’s Disease.
|
Figure 8: Alzheimer's Disease |
Fig. 8 Explanation: Influence of infectious and beneficial bacteria species on the progression of Alzheimer's Disease. Source of data: Pluta et al, 2020. Adapted for simplicity.
Pluta et al (2020) investigated the mechanisms behind these responses and concluded that as the gut-brain axis exists via activity in the endocrine and immune systems, an interaction may also exist with the different levels of metabolites secreted from the commensal or infectious bacteria. For example, Enterobacterial spp. may increase the amount of amyloid depositions in the brain and thus increase the local inflammatory response and reducing cognitive functions.
Moreover, the microbiome spectrum may produce a variety of short chain fatty acids that regulate the development and maturation of the microglia; reducing the ability of the brain’s local immunity and resulting in the reduction in phagocytosis of amyloid and tau protein fibrils. In addition, Valeric acid was shown to completely inhibit the deposition of b-amyloid in the brain.
B. breve and other lactic acid bacteria were shown to reduce the cognitive impairment in older people with this disease as they suppressed the inflammation of neural tissue, most significantly in the Hippocampus. It was also noted that in certain bacterial strains, a reduction in the amyloid plaque formation can be shown (Pluta et al, 2020).
It can be concluded that a dysbiosis can result in a pro-inflammatory response that manifests locally within the brain tissue. These certain metabolites may be involved in the increased permeability of the blood-brain barrier permitting an exaggerated immune response and increase amyloid deposition. More research is required in the mechanisms of these responses but it can be stated that fluctuations in the microbiome can be reflected within the progression of this disease.
Conclusion
From the above evidence, it can be indisputable that a connection between the gut and the brain exists. This axis has a major influence on the functioning of the brain by using strain specific compounds to trigger a response within the immune system. This response is well manifested within the brain tissue and can have a positive or negative effect on the well being of the animal. Moreover, neural excitation via metabolites can have a somewhat direct effect on the brain via the enteric nervous system and the Vagus Nerve (X).
These above mechanisms permit research into the specific responses that will be seen in the brain. It was concluded that the by-products of the microbiome are not homogenous and will have specific responses in the host. Altering the balance of the microbiome spectrum will elevate (or introduce) certain specific metabolites and their effect on the brain can be monitored. With saying this, probiotics or “psychobiotics” can be extremely useful in the manipulation of the brain chemistry as with regular treatments, they provide a controlled microbiome equilibrium in favour of the beneficial responses. In effect, the commensal bacteria spectrum was improved.
The Bifidobacterium spp. and Lactobacillus spp. investigated in this essay have shown to be beneficial to the host, therefore probiotics will favour these species for commercial and medical use. However, the Enterobacterium spp. and the H. pylori were shown to have an overwhelming negative effect on the host. These contrasting conditions has shown that the gut brain axis does in fact exist, and that certain bacteria have the ability to inflict damage on the host while others have the ability to create a response that aids the organism’s ability to maintain homeostasis.
References
• Allen, A. P.; Hutch, W.; Borre, Y. E.; Kennedy, P. J.; Temko, A.; Boylan, G.; Murphy, E.; Cryan, J. F.; Dinan, T. G.; Clarke, G. (2016): Bifidobacterium longum 1714 as a translational psychobiotic: modulation of stress, electrophysiology and neurocognition in healthy volunteers. Translational Psychiatry 6:(11) e939–e939. https://doi.org/10.1038/tp.2016.191
• Kumar, D. K. V.; Choi, S. H.; Washicosky, K. J.; Eimer, W. A.; Tucker, S.; Ghofrani, J.; Lefkowitz, A.; McColl, G.; Goldstein, L. E.; Tanzi, R. E.; Moir, R. D. (2016): Amyloid-β peptide protects against microbial infection in mouse and worm models of Alzheimer’s disease. Science Translational Medicine 8:(340) 340ra72-340ra72. https://doi.org/10.1126/scitranslmed.aaf1059
• Pluta, R.; Ułamek-Kozioł, M.; Januszewski, S.; Czuczwar, S. J. (2020): Gut microbiota and pro/prebiotics in Alzheimer’s disease. Aging 12:(6) pp5539-5550. https://doi.org/10.18632/aging.102930
• Savignac, H. M.; Kiely, B.; Dinan, T. G.; Cryan, J. F. (2014): Bifidobacteria exert strain-specific effects on stress-related behavior and physiology in BALB/c mice. Neurogastroenterology & Motility 26:(11) 1615–1627. https://doi.org/10.1111/nmo.12427
• Savignac, H. M.; Tramullas, M.; Kiely, B.; Dinan, T. G.; Cryan, J. F. (2015): Bifidobacteria modulate cognitive processes in an anxious mouse strain. Behavioural Brain Research 287: 59–72. https://doi.org/10.1016/j.bbr.2015.02.044
• Tan, Benjamin, Y. Q.; Paliwal, P.; Sharma, V. (2019): Gut Microbiota and Stroke. Annals of Indian Academy of Neurology 23:(2) pp155–158. https://doi.org/10.4103/aian.AIAN_483_19
• Uddin, Md. S.; Kabir, Md. T.; Niaz, K.; Jeandet, P.; Clément, C.; Mathew, B.; Rauf, A.; Rengasamy, K. R. R.; Sobarzo-Sánchez, E.; Ashraf, G. M.; Aleya, L. (2020): Molecular Insight into the Therapeutic Promise of Flavonoids against Alzheimer’s Disease. Molecules 25:(6) 1267. https://doi.org/10.3390/molecules25061267
• Wang, H.; Braun, C.; Murphy, E. F.; Enck, P. (2019): Bifidobacterium longum 1714TM Strain Modulates Brain Activity of Healthy Volunteers During Social Stress. The American Journal of Gastroenterology 114:(7) 1152–1162. https://doi.org/10.14309/ajg.0000000000000203
Figures
DISCLAIMER: Figure 1 and Figure 2 were taken directly from freely usable media sites (Wikimedia Commons). No changes to the original content were made. Links to the original figures are provided.
Link to original of Figure 1: https://commons.wikimedia.org/wiki/File:Hypothalamo%E2%80%93pituitary%E2%80%93adrenal_(HPA)_stress_axis.jpg?fbclid=IwAR1-hracDXOeJlPWTDjfzTyvOWY7aCdzNBsCuA2Jwp6dkgcXGpAMY5FP3EQ
Link to original of Figure 2: https://commons.wikimedia.org/wiki/File:Liu_gut-brain-axis_schema.png?fbclid=IwAR19ekbwVqHf30orMnOMLMzt9B_HonSV2XNH3q6jgLKvyV8QJohthNwZo8o
DISCLAIMER: The following figures (Fig. 3-8) are only a demonstration of the results. In no way were they copied directly. Furthermore, the values presented are not a representation of the values in the experiments; they are merely a relative comparison for aiding the reader’s understanding. Further citation should not include these values but instead refer to the cited papers for accurate results.
Figure 3 Source of data: Savignac et al, 2014. Adapted for simplicity.
Figure 4 Source of data: Savignac et al, 2014. Adapted for simplicity.
Figure 5 Source of data: Savignac et al, 2014. Adapted for simplicity.
Figure 6 Source of data: Savignac et al, 2014. Adapted for simplicity.
Figure 7 Source of data: Savignac et al, 2015. Adapted for simplicity.
Figure 8 Source of data: Pluta et al, 2020. Adapted for simplicity.