Itt írjon a(z) Pain_physiology-ról/ről
Physiology Of Pain
Project by: Jad El Hawly, Alice Taube, Oscar Joseph Ullomi
Supervisor: Dr. Zoltan Balazs Barany
Physiology Department, University of Veterinary Medicine, Budapest
Contents
What is pain?
Pain is defined by the International Association for the Study of Pain (IASP) as "an unpleasant sensory and emotional experience associated with actual or potential tissue damage". Therefore it holds functions in creating awareness of, and behaviours and reactions to avoid or terminate, stimuli which can cause harm to the organism. The sensory and emotional aspects go to make up the subjective experience of pain, creating a strong and lasting learnt avoidance reaction against similar stimuli that may be encountered in the future. This involves processing of the novel sensory input with memories and established emotional patterns.
The nerve endings sensing painful stimuli are distinct from those which detect other sensations, such as light touch. (Julius and Basbaum, 2001). These nerve endings lead to specific primary sensory afferent nerve fibres termed nociceptors, which transmit the stimulus to the dorsal horn of the spinal cord. Here it will synapse to a secondary afferent neuron in the ascending pathway to the brain. The detection of pain itself is termed Nociception, and can be classed as a sense similar to vision or olfaction due to its selectivity for stimuli, in this case those that are harmful not benign (Julius and Basbaum, 2001).
There are two types of pain occurring in response to injury. The first is acute, fast pain which is well localised, the second is slow pain, which tends to be dull with a longer duration, and to be less well localised Fig. 3.. In response to acute injury there will first be acute first pain indicating the location of injury, and a need to remove or avoid the damaging stimulus. This will be followed by the second pain, which has a function in changing behaviour, such as inducing cleaning behaviours such as licking, and avoiding pressure or impact which could affect the healing and recovery of the injured area.
Pain Terminology
The pain Terminology can be classified to:
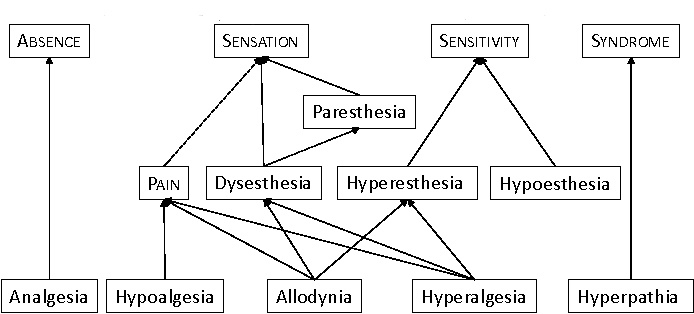
Fig 1.
Figure 1. Pain Terminology Hierachy
⇒Analgesia: occurs when there is lack of pain sensation.
⇒Anesthesia: occurs when there is lack to any sensation.
⇒Allodynia: when the pain due to non-harmful stimulus.
⇒Hyperalgesia: increased response to harmful stimulus.
⇒Hyperesthesia increase sensitivity to stimulation.
⇒Hyperpathia it is a painful syndrome due to an abnormally painful reaction to stimulus.
⇒Hypoalgesia pain in response to a normally painful stimulus.
⇒Neuralgia: painful site innervated by a nerve or group of nerves.
⇒Dysesthesia unpleasant abnormal sensation. (IASP)
The Pain Process
- The pain process is made up of four steps (1) transduction, (2) transmission, (3) modulation, and (4) perception
|
1-Transduction:
Transduction is a process of converting noxious stimuli to a neuronal signal. Receptors for noxious stimuli can be generally categorized as cation channels which de-polarise the peripheral terminals of nociceptors, creating an action potential (Du and Gamper, 2013). Nociceptor terminals may require intense stimulation to generate the action potential, meaning that the threshold potential that must be reached is high. There are several types of noxious stimuli that elicit a pain reaction in the peripheral tissues. These include heat, cold, mechanical, and chemical. Mechanical, heat and cold stimuli are generally short lasting, but chemical stimuli last longer and can also represent the reactions within the tissues to the injury, such as inflammation, contributing to the slow-type second pain.
►Heat
Studies on the sensing of heat induced pain have suggested several specific receptors that may be involved in initiating the pain pathways.
⇒ TRPV1,2,4 - transient receptor potential TRP – Vanilloid receptors. These are receptive to vanilloid compounds such as Capsaicin. Capsaicin is the compound found in chilli peppers that activates the same receptors as high temperatures, leading to “heat”. These receptors act as a plasma membrane channel for cations that are only activated above certain temperatures. The temperature varies based on the specific receptor type (Julius and Basbaum, 2001), (Basbaum et al. 2009).
⇒ VRL1 - Vanilloid receptor like channels. These are similar to vanilloid receptor channels but don’t respond to vanilloid compounds, only to heat. The temperature of activation is 52°C (Julius and Basbaum, 2001).
►Cold
The receptors and afferents involved in nociception of cold stimuli are different and less numerous than those implicated in the detection of heat (Julius and Basbaum, 2001). Menthol and eucalyptol are chemicals used in the detection of cold based pain, as they contain similar properties.
⇒ TRPM8 – Transient receptor potential (Menthol) - a channel that is sensitive to both cold and menthol.
⇒ TRPA1 – Transient receptor potential that may detect cold below 15°C. This channel is sensitive to icilin and menthol at high concentrations.
⇒ KCNK – a family of voltage gated K+ channels, including KCNK2 (TREK-1) and KCNK4 (TRAAK) which have some function in nociception, including possible response to cold (Basbaum et al. 2009).
►Mechanical
Mechanical pain can be due to such stimuli as intense pressure, deformation, destruction of tissue, or swelling. There are several candidate mechanisms and receptors which may be responsible for mechanical nociception. These include mechanosensitive (channels opened by cell membrane deformation) and mechanochemical (releasing chemical messenger in response to stretching or deformation)(Julius and Basbaum 2001).
Another possible way that mechanical nociception can occur is through the release of ATP through a damaged or distorted cell membrane, which when existing extracellularly can function in ATP gated ion channels, or G-protein coupled ATP receptors, leading to the activation of surrounding nociceptor terminals in the tissues (Julius and Basbaum,2001).
Other suggested receptor mechanotransducers include:
⇒ ASIC1,2,3 – Acid sensing ion channels. These are expressed in mechanosensitive neurons but their role in nociception hasn’t been proven.
⇒ TRPV2,4 – These are heat/vanilloid receptors which can also respond to stretching stimuli.
⇒ KNCK2,4 – these are also implicated in cold nociception but may have a mechanoreceptor role too. KNCK18 responds to compounds in Szechuan peppercorns which cause tingling sensations, but beyond this mechanoreceptive response to noxious mechanical stimuli hasn’t been proven. (Basbaum et al. 2009).
⇒ Piezo1, Piezo 2 - Transmembrane proteins important in mechanotransduction of signals (Coste et al. 2010).
►Chemical
Chemical nociception takes place as a result of environmental irritants or physiological stress (Basbaum et al. 2009). Some receptors for plant derived chemical irritants have already been mentioned in the context of temperature based nociception, for example TRPV1 (capsaicin), and TRPM8 (menthol).
Physiological stress can involve the chemical factors involved in inflammation, of which they or their precursors are released by cells in response to tissue damage, and are known collectively as “inflammatory soup”. Components of the inflammatory soup include H+ ions K+ ions, histamines, ATP and serotonin which affect neuronal excitability, and Bradykinin, prostaglandins and nerve growth factors/neurotrophins which bind to receptors which are metabotropic (leading to second messenger cascades) (Julius and Basbaum, 2001). One of the effects of these chemicals is to create a long lasting secondary pain sensation, leading to behavioural protection of the healing tissues.
2-Transmission:
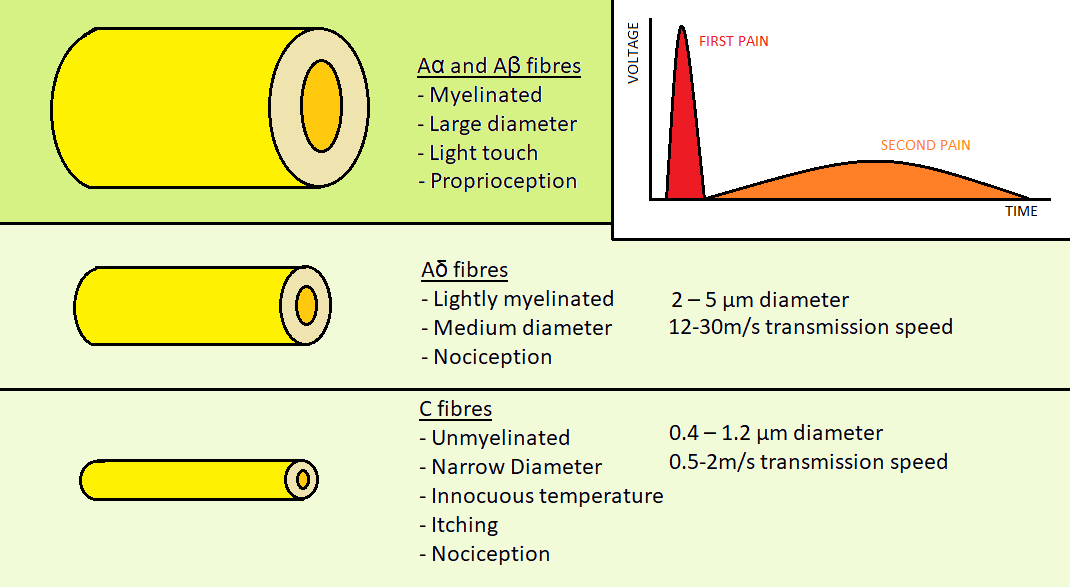
Fig 3.
Figure 3: Aα, Aβ, Aδ & C fibers
After stimulation of the peripheral nerve ending a depolarisation will occur in the nociceptor axon. As previously mentioned there are nociceptor fibres for acute first pain, and others for slower, dull second pain. There are four different types of primary afferent fibres for skin sensation, two of which are involved in nociception. Aα and Aβ fibres are myelinated fibres with a large diameter that are involved in transmission of stimuli from light, non-painful touch.
The two fibres involved in nociception are the Aδ and C type fibres Fig. 3..
⇒ Aδ fibres are the fibres which transmit the acute first pain. They are myelinated for the sending of rapid impulses and thinner than non-nociceptor fibres, at 2 – 5 µm in diameter. The rate of conduction s 12-30m/s.(Julius and Basbaum, 2001)
⇒ C type fibres are unmyelinated. They are the thinnest primary afferents at 0.4 – 1.2 µm in diameter. The rate of conduction is 0.5-2m/s, significantly slower than the Aδ fibres. They can be further subdivided into peptidergic and non-peptidergic fibres. (Julius and Basbaum, 2001)
The primary afferent nociceptors are defined as pseudo-unipolar, as they feature central and peripheral terminals, and can receive analgesics at both ends (Basbaum et al 2009). The soma, or cell body of the sensory neuron is located in the dorsal root ganglion of the spinal cord for innervation of the body, and the axon projects a branch to the periphery and a branch into the spinal cord. For facial innervation the soma of the neuron cell is located at trigeminal ganglia (Julius and Basbaum, 2001).
The dorsal horn of the spinal cord is divided into layers known as laminae. These are where the sensory afferent fibres project to. There are 5 laminae altogether. Lamina 1 is where Aδ fibres project, Lamina 2 is where C fibres project. Laminae 3 and 4 are where Aβ non nociceptive sensory fibres project. Lamina 5 receives fibres from Aδ and Aβ fibres (Julius and Basbaum, 2001).
The main neurotransmitter chemicals that are responsible for stimulating nerve terminals and bridging synapses include Glutamate and Substance P. Glutamate receptors are widely present in the body while Substance P is very specific to nociceptive signalling (Zieglgänsberger, 2019).
Transmission of the pain signal along the fibres occurs through the movement of ions through voltage gated ion channels, generating action potentials:
⇒ Voltage Gated Sodium Channels
There are two classes of Sodium ion channels: tetrodotoxin (TTX) sensitive, or tetrodotoxin resistant. Tetrodotoxin is a toxin present in some species of marine fish which specifically blocks the sodium ion channels, and has been used to differentiate channel types (Basbaum et al. 2009). The TTX resistant channels NAV1.8 an NAV1.9 are involved in nociception. NAV1.3 is TTX sensitive and has been suggested to sustain high frequency action potentials in chronic pain, due to faster recovery from stimulation (Lee and Ruben, 2008)
⇒ Voltage Gated Potassium Channels
Potassium channels when open maintain the normal excitability of neurons and are believed to spontaneously induce pain when blocked (Du, Gamper, 2013).
⇒ Voltage Gated Calcium Channels
Like sodium channels, calcium channels are classified based on their sensitivity to pharmacological agents, being subdivided into L, N, P/Q, R, T type channels. All are involved in nociception, with the N-type channels playing a prominent role. These channels are active in the dorsal root ganglion and in synapses, where they are stimulated by action potentials to assist the release of vesicles into the synaptic cleft.(Park and Luo, 2010)
3-Modulation:
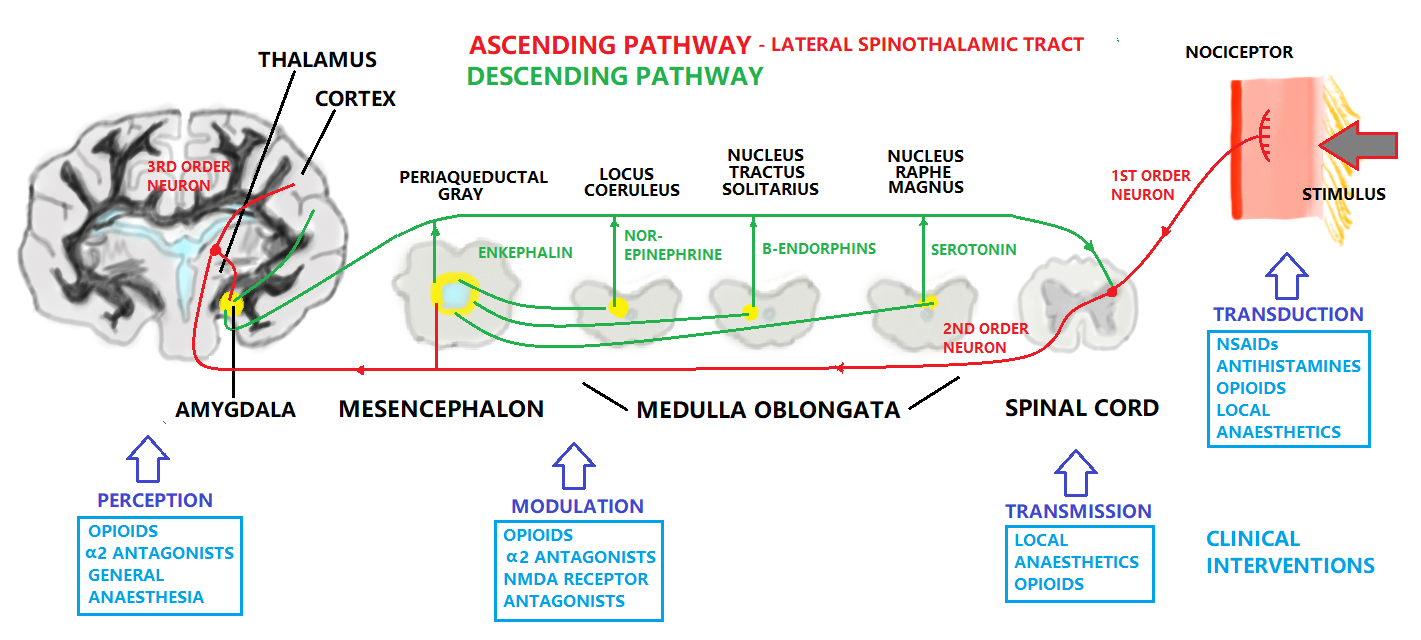
Modulation refers to the processing of the pain signal, and will attenuate or strengthen the effects that are consciously experienced due to the stimulus. The ascending pain pathway refers to the path of the pain signal from the site of stimulus towards the spinal cord via primary axon fibres, and then consequently the brain via secondary axon fibres in the spinothalmic tract. The spinothalmic tract terminates at the thalamus. The thalamus sends on the signal through tertiary axons to the area of the somatosensory cortex corresponding to the affected body part, where the pain is perceived. The descending pain pathway is responsible for modulation of the ascending pathway Fig. 2..
One of the most important discoveries in pain research to see if the brain contains substances that have the same pharmacological properties as synthetic opioid drugs and plant-derived opiates. These substances, called endogenous opioid peptides, are present within nerve cells of the peripheral and central nervous systems (Palkovits,1984).The opioid peptides modulate nociceptive input in two ways: (1) inhbition of Ca2+ influx into presynaptic termnial by blocking the neurotransmitter, or (2) the potassium channels will open, which hyperpolarizes neurons and inhibits spike activity. They act on various receptors in the brain and spinal cord, three classes of opioid receptors have been identified: μ-mu, δ-delta and κ-kappa. So it can be divided to Peripheral or Central modulation. The modulation of pain occurs always peripherally at the nociceptor, in the spinal cord or in some other cases in the supra spinal structures. This modulation can either inhibit or facilitate pain (Osterweis, 1987).
In central modulation there are several areas of the brain that are implicated in pain modulation, some responsive to opioids, and some apparently responsive to the “placebo or nocebo effect”. Fields and Basbaum (1984) proposed the structural components of the descending opioid-related pain inhibitory system. They indicate that several centers are involved in generating analgesia, periventricular and periaqueductal grey, the rostral ventral medulla, and the spinal cord, these three received extensive investigation. Periaqueductal gray lines the mesencephalic aquaduct between the third and fourth ventricles, and is responsible for modulation of the descending pain signal, as well as fear and some autonomous responses. The rostral ventral medulla features several nuclei involved in pain modulation, including Locus Coeruleus, Nucleus Raphe Magnus, and Nucleus Tractus Solitarius. The nucleus raphe magnus sends axons to the dorsal horn of the spinal cord to provide inhibition to the synapse of the ascending pathway. It also stimulates opioid releasing interneurons, which inhibit the release of substance P neurotransmitter. The descending pain modulation system compared to the afferent input is less well known, but hypothalamic and amygdala inputs are involved. The amygdala is part of the limbic system controlling emotions, and the thalamus is a relay station for the sensory pathways of the nervous system, which enables focusing on relevant or imminent information. Due to extensive collaterals to different parts of the brain, the pain experienced can be altered by emotional state, expectation, and level of cognition/excitement (Ossipov et al. 2010). Descending pain modulation neurons form a network that extends from the fontal cortex and hypothalamus down through the periaqueductal grey (PGA) to the rostral ventral medulla and then to the spinal dorsal horn downward (Fields and Basbaum, 1984).
4-Perception:
In the brain, pain can be nociceptive input . New data suggest that there is no single, precise location where pain perception occurs so instead pain perception involves several brain structures.It is known that the brain is necessary for pain perception hence no brain, no pain. Lack of a behavioral response to a noxious stimulus does not indicate that their is lack of pain perception (Osterweis, 1987). Moreover perception can be defined as central processing of nociceptive impulses in order to interpret pain.In the perception neurons are located in the thalamus and project to somatosensory areas II and I in the post-central gyrus and superior wall of the sylvian fissure. The perception & discrete localization of pain can take place in mentioned cortical areas. Some of the fibres project to the anterior cingulated gyrus and can mediate the suffering and emotional components of the pain. Also it is the end result of the neuronal activity of pain transmission and where pain becomes a conscious multidimensional experience. The multidimensional experience of pain has effective-motivational, sensory-discriminative, emotional and behavioral components (Osterweis, 1987).
So as a summary for the above four steps; for an animal to experience pain, nociceptive information must be sent to higher centers in the CNS to be integrated, modulated, and interpreted into the conscious perception of pain. Noxious stimuli ( which are heat, cold, mechanical, chemical) activate the free sensory nerve endings which are known as nociceptors. A-δ and C-fibers transmit the sensory information from nociceptors to the spinal cord (dorsal horn part), which directs and modulates input from the periphery. The nociceptive information arriving in the dorsal horn of the spinal cord can activate the motor neurons which are responsible for the reflex of noxious stimuli.
The General Pain Pathway
Within the pain pathway there are three orders of neurons which are respossible for the action potential(s):
First order → The pseudo unipolar neurons which have cells bodies within the dorsal root ganglion, they have one axon which splits into two branches, a peripheral and a central branch.
Second order → The cell bodies of these neurons are found in the Rexed laminae of the spinal cord so decussate in the anterior white commissure and ascend cranially in the spinothalamic tract.
Third order → The cell bodies of these neurons lie on VPL of the thalamus and they will project via the posterior limb of the internal capsule to terminate in the ipsilateral of postcentral gyrus.
Types of Pain
Physicians & neuroscientists generally classify pain into different ways as the following:
►Acute pain
Simple difintion is that acute pain is caused by an injury in the body. Acute pain syndromes have clear etiologies and respond readily to appropriate therapy. The presence of acute pain warns of potential damage that requires action by the brain, and it can develop slowly or quickly and goes away when the injury heals. They are frequently caused by tissue damage such as bone, organs, muscle, for example broken bones / surgery / burns (Brandner, 2010). This pain is also often accompanied by acute distress and anxiety.
►Chronic pain
Chronic pain will serves less of a warning function and may become part of the patient's life. This type persists long after the trauma has healed and in many cases, it occurs in the absence of any trauma, it does not warn the body to respond, and it usually lasts longer than acute pain. Some examples that can illustrate chronic pain include: arthritis pain / nerve damage pain / vertebrates pain. Several reasons for the occurrence of chronic pain have been proposed. These include spontaneous inflammatory pain arising from damaged receptors, spinal changes in plasticity due to prolonged pain experiences, and damaged opioid systems (Curatolo et al. 2006).
Chronic pain syndromes can be divided into three categories: (1) those associated with clinically significant structural disease (e.g., rheumatoid arthritis, cancer pain); (2) those associated with a history of structural disease but with psychological factors that predispose to physiologic alterations, (e.g. muscle spasm in lower back) ; (3) those with no physiologic or anatomic basis for the patient's complaints, and can be exemplified by the somatoform disorders. Tilll now the time frame for the development of chronic pain is not exact.
|
|||
Type |
Duration |
Characteristics |
Management |
Acute Pain |
<3 months |
Severe, but usually manageable such pain from injuries |
by anesthesiologist pain, + opioids |
Chronic Pain |
>3-6 months |
Difficult to treat, drug-seeking |
by analgesics, antidepressants + anticonvulsants |
Table 1 Comparison between Acute & Chronic pain |
|||
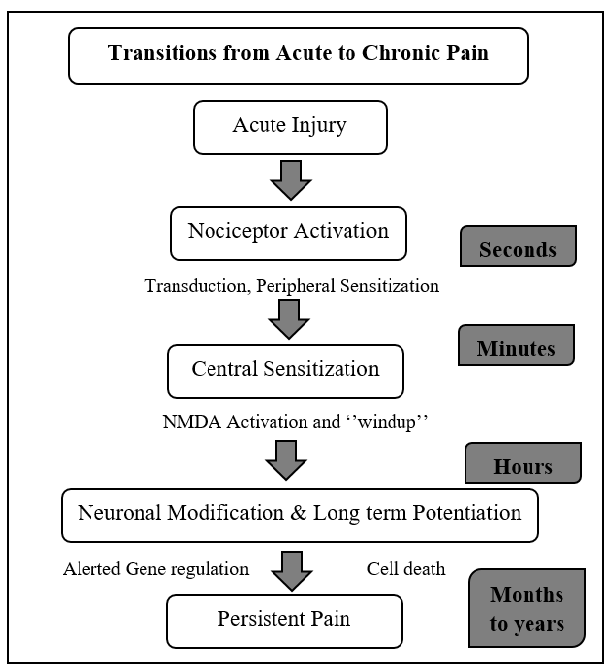
Transition from Acute to Chronic Pain:
This process can be seen below in Fig. 4..
When there is an acute injury this injury will activate the nociceptor, leading to windup of central sensitization and long term potentiation, ending with presistent pain which lasts for months or years.
|
►Nociceptive pain
This is the pain detected by nociceptors around the body. There are three types of nociceptive pain:
- Radicular pain occurs only when the nerve roots are irritated. It goes on forlimb or hindlimb through a nerve that comes from the the spinal cord.
- Somatic pain occurs when any of the pain receptors are in tissues, such as bone, muscles, or skin, are activated. It is stimulated by movement.
Visceral pain occur in internal organs, such as involuntary muscles in the heart it usually described as aching (Dubin, 2010). It utilises similar nociceptors to second pain, and as such tends to be dull and poorly localized.
|
|||
Type |
Characteristics |
Mechanism |
Pharmacologic Treatments |
Radicular Pain |
localized & diffuse pain |
Associated with localized inflammation |
NSAID, steroid, opioids |
Somatic Pain |
Superficial or deep pain |
Mechanical, thermal, or chemical stimuli |
NSAID, antispasmodics |
Visceral Pain |
Constant & poorly localized |
Visceral distension |
NSAID, steroid |
Table 2 Comparison between Nociceptive pain types |
|||
►Neuropathic pain
After disappearance of inflammation and complete healing of tissue damage, the brain may become hypersensitive to the slightest pain signals. Nociceptive pain is often associated with tissue damage where as neuropathic pain is one that involves the nervous system. Neuropathic pain involves pain pathways that have become ingrained and reinforced for a long time. This pain results from damage to a nerve or some other part of the central nervous system, and it is not frequently diagnosed in veterinary medicine, mainly because animals cannot communicate a problem such as a tingling sensation (Holland, 2017).
►Cancer pain
Or it can be named as malignant this pain is associated with malignant tumors. Cancer pain can also be associated with invasive procedures or treatments and note that some neuroscientists classify cancer pain with chronic pain (Curatolo et al. 2006).
►Referred pain
Referred pain is pain that is felt on other areas of the body from where the signal originates, usually a peripheral pain sensation indicating a visceral origin. These tend to be consistently corresponding defined areas known as "head zones". Referred pain can be misleading but with understanding of the different head zones can be utilised in the diagnoses of illnesses, a common example would be pain in the chest and left arm, indicating pathologies of the heart in humans. There are four physiological mechanisms have been proposed to explain referred pain (Osterweis, 1987):
- Activity in sympathetic nerves - Sympathetic nerve projections can sensitize peripheral nociceptor terminals as part of the sympathetic response.
- Peripheral branching of primary afferent nociceptors - The brain may have errors in differentiating between nociceptor branches.
- Convergence projection - A nerve cell in the spinal cord may receive projections from both visceral and peripheral terminals, and may not differentiate.
- Convergence facilitation - Pain projection neurons in the spinal cord can be sensitized by afferent nociceptor messages from another part of the body, leading to raising of the resting sensitivity.
Clinical aspects of Pain, and Therapeutic Methods
Understanding pain physiology and how biochemical mediators are responsible for pain sensation can be of critical importance in as far as pain management is concerned. Firstly, the physician has to understand the cycle of pain and what happens to the body at each step and what biochemical changes occur. In doing so, then it would be so easy to understand what will actually happen for every intervention that is to be used Fig. 2.. This knowledge is also significant for understanding why chronic pain for instance, may not respond to the commonly used non-steroidal anti-inflammatory drugs (NSAIDs) in pain alleviation. Pain can be reduced or rather gotten rid of by interventions that are aimed at inhibiting the activation of nociceptors, blocking impulse transmission, stimulating the body’s own pain modulation system. Stimulation of other senses such as massaging, warm or cold compresses help in relieving pain activation of gate cells which can inhibit neurotransmitter release from pain fibres through encephalin which acts on opioid receptors and inhibit substance P. According to the University College of Dublin (2018/19), it is reported that acupuncture increases opioid release, Aspirin inhibits the activation of nocireceptors by reducing the release of prostaglandins, local anaesthesia blocks action potential conduction in pain fibres, Morphine inhibits signal transmission by binding to opioid receptors. Post-operative pain can be reduced by combing both local and general anaesthesia during the operation. In South Africa, pain management strategies are based on traditional analgesics, that is, paracetamol and non-steroidal anti-inflammatory agents. These drugs are mostly used for acute pain (Wren et al. 2019) . In the South African schools where the studies were conducted, teachers or nurses sometimes only offered children a glass of water as an alternative to pain medication (Adolfsson et al. 2018; Nilsson et al. 2016).
|
|||
Pharmacological interventons |
Methods of Interventions |
Non-pharmacological interventions |
Rehabilitation |
NSAIDs, Opioids |
Local anaesthesia, injections |
Acupuncture, massage, music therapy |
Physical therapy, Music therapy |
Table 3. Clinical interventions for pain |
|||
Pain Scoring
In human medicine, pain determination is based on self-reporting. Veterinary patients however are non-verbal and in order for the practitioner to determine the presence and severity of pain there are some scoring systems used in practice. There is not currently a universally accepted scoring system, as it is difficult to achieve complete objectivity. One type of scoring system commonly implemented is the Simple Scoring System. This attributes a numerical value (usually ranging 1-4 or 1-6) to a range which spans from the absence of pain to extremely severe debilitating pain. A similar type of scoring system is the Visual Analogue Scale which is non-numerical, but allows the practitioner to assign a degree on a scale of severity. The scoring will be assigned to the state of the animal based on the presence or absence of several parameters which vary according to the species (Bloor, 2017) .
There can be inferred a motor response to pain, causing complex behaviors that are different in each species. For this reason, behavioral changes have been recognized as the indicators of pain animals, where this unpleasant emotional changes in the behavior which lead to show the location and severity of where the pain is .(León-Olea, 2002). Some examples of behavioral changes that must be taken in consideration for animals are self multilation, aggression, vocalizations, restlesssness, changes in social interaction, sleep alteration. A good knowledge of the species normal behaviour is required in order to assign the pain score, and in some cases a behavioral history of the patient will also need to be considered. Some species hide pain extremely well until it becomes critical, for example rabbits and ferrets.
Some examples of the parameters indicating pain are:
⇒ Facial expression, such as squeezed eyes and open mouth. Facial “grimace” scales are often used in research.
⇒ Body movement and posture, such as tucking of abdomen, clenching of digits, limping.
⇒ Response to pressure on different parts of the body, conducted by palpitation.
⇒ Vocalisation, degree and type such as crying and hissing.
⇒ Behaviour, such as restlessness, excessive sleeping, irritability.
⇒ Physiological markers, such as heart rate, blood pressure, breathing, pulillary diameter.
⇒ Biological markers, such as cortisol and adrenaline in body secretions.(Bloor, 2017)
The physiological parameters for animals when they feel pain can be altered as an autonomic response to the nociception. However, these parameters are affected by many factors as fear and stress (Cambridge, 2000; Franzini de Souza, 2000). In the case of animals that suffer chronic pain, these variations tend to be less evident (McKune CM). The Biological parameters can include the measurement of chemical mediators and the hormonal concentrations. For example the changes in plasma hormone concentrations like cortisol, β-endorphins and catecholamines, which have been considered as indirect indicators of pain. Only weak correlations of behavior and increases in plasma levels of the mentioned hormones have been determined (Gutiérrez, 2017) more over, it is well-known that the relation among physiological stress pain and behavioral disorders is complex; so stress responses that may not always be related directly to pain.
Conclusion
It is the professional obligation of the veterinarian to alleviate suffering in their patients that may come from injury or illness. Pain is also sometimes an unavoidable consequence of necessary veterinary interventions, such as surgeries. It's important in a clinical setting to have a good appreciation of pain physiology, in order to understand the causes and select appropriate therapies for pain management. Reducing pain improves patient outcomes, quality of life, and enhances the relationship between the practitioner, client and patient (AAHA, 2015) .
References:
Articles:
Allan I. Basbaum, Diana M. Bautista, Grégory Scherrer, David Julius. (2009). Cellular and Molecular Mechanisms of Pain. CELL. 139 (2), 267–284.
Brody H. (1982) The lie that heals: the ethics of giving placebos. Annals of Internal Medicine. 97, 112–118.
Cambridge, Tobias, Newberry, Sarkar. (2000) Subjective and objective measurements of postoperative pain in cats. Journal of American Veterinary Medicine Association. 217(5), 685-690.
Casey, Minoshima, Morrow, & Koeppe. (1996). Comparison of human cerebral activation pattern during cutaneous warmth, heat pain, and deep cold pain. Journal of Neurophysiology, 76, 571-581.
Bertrand Coste, Jayanti Mathur, Manuela Schmidt, Taryn J. Earley, Sanjeev Ranade, Matt J. Petrus, Adrienne E. Dubin, Ardem Patapoutian. (2010). Piezo1 and Piezo2 are essential components of distinct mechanically-activated cation channels. Science. 330 (6000), 55–60.
Michele Curatolo, Lars Arendt-Nielsen, Steen Petersen-Felix. (2006). Central Hypersensitivity in Chronic Pain: Mechanisms and Clinical Implications. Physical Medicine Rehabilitation Clinic of North America. 17, 287–302.
Xiaona Du, Nikita Gamper. (2013). Potassium Channels in Peripheral Pain Pathways: Expression, Function and Therapeutic Potential. Current Neuropharmacology. 11 (6), 621–640.
Dubin, Patapoutian (2010) Nociceptors: the sensors of the pain pathway. Journal of Clinical Investigation. 120. 3760-3772.
David Julius, Allan I. Basbaum. (2001). Molecular mechanisms of nociception. NATURE. 413, 203-210.
Franzini de Souza, Penteado Martins Dias, Nascimento de Souza, Alvesde Medeiros. (2000) Use of behavioural and physiological responses for scoring sound sensitivity in dogs. Plos One. 13 (8).
Katon W, Kleinman A, Rosen G. (1982) Depression and somatization: a review. The American Journal of Medicine. 72:127 (35), 241–347.
Chong Hyun Lee, Peter C. Ruben. (2008). Interaction between voltage-gated sodium channels and the neurotoxin, tetrodotoxin. Channels. 2 (6), 407-412.
Levine J. (1984) Pain and analgesia: the outlook for more rational treatment. Annals of Internal Medicine. 10, 269–76.
Melzack R, Wall PD. (1965) Pain mechanisms: a new theory. Science. 150, 971–979.
Michael H. Ossipov, Gregory O. Dussor, Frank Porreca. (2010). Central modulation of pain. The Journal of Clinical Investigation. 120 (11), 3779-3787.
John F Park, Z David Luo. (2010). Calcium channel functions in pain processing. Channels. 4 (6), 510-517.
W. Zieglgänsberger. (2019). Substance P and pain chronicity. Cell and Tissue Research. 375 (1), 227–241.
Books:
Multidisciplinary Pain Management for Pediatric Patients with Acute and Chronic Pain: A Foundational Treatment Approach When Prescribing Opioids DeGowin EL, DeGowin RL. Bedside diagnostic examination. New York: Macmillan, 1981.
Fields H. L., & Basbaum, A. L. (1984). Central nervous system mechanisms of pain modulation. In M. R. Wall PD (Ed.), Textbook of pain (3rd ed. ed., pp. 243-257). New York: Churchill Livingstone.
Fields HL, Levine JD. Pain: a clinical approach based on physiological principles. In: Isselbacher KJ, et al., eds. Harrison's principles of internal medicine. Update II. New York: McGraw-Hill 1982;205–20.
McKune CM, Murrel JC, Nolan AM. Nociception and pain In: Grimm KA, Lamont LA, Tranquili WJ, et al, editors. Lumb and Jones Veterinary anesthesia and analgesia.
Posner JB. Disorders of sensation. In: Wyngaarden JB, Smith LH, eds. Cecil textbook of medicine. 17th ed. Philadelphia: W.B. Saunders, 1985.
L Bromley, B Brandner Oxford University Press (2010), Acute pain OPML, ISBN 978-0-19-923472
Other Publications:
Mark Epstein, Ilona Rodan,Gregg Griffenhagen, Jamie Kadrlik, Michael Petty, Sheilah Robertson. (2015). 2015 AAHA/AAFP Pain Management Guidelinesfor Dogs and Cats. American Animal Hospital Association, Practice guidelines.
Osterweis M, Kleinman A, Mechanic D, (editors) (1987). Institute of Medicine (US) Committee on Pain, Disability, and Chronic Illness Behavior. Pain and Disability: Clinical, Behavioral, and Public Policy Perspectives. Washington (DC): National Academies Press (US).
IASP Newsletter, 3, 3-5. Jones, A. K. P. (1997). Pain, its perception, and pain imaging.
Websites:
Claire Bloor. (2017). Pain scoring systems in the canine and feline patient . Available: https://www.theveterinarynurse.com/review/article/pain-scoring-systems-in-the-canine-and-feline-patient. Last accessed April 2020.
Peter Dudley, (2018) Teach me physiology-pain, Available: https://teachmephysiology.com/nervous-system/sensory-system/pain-pathways/ .Last accessed April 2020.
International Association for the Study of Pain (2018) Available: https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698. Last accessed April 2020.
Alyson Lozicki, PharmD (2017) — Written by Kimberly Holland Available: https://www.healthline.com/health/pain-relief/oxycodone-vs-hydrocodone. Last accessed April 2020.
Merck & Co.,(1955)Inc,. Kenilworth NJ, USA is a global healthcare leader workingAvailable: https://www.merckvetmanual.com/SearchResults?query=pain. Last accessed April 2020.
Merskey H, Bogduk N. (1994) Classification of chronic pain. 2nd ed. Seattle: IASP Press; Available: https://www.physio-pedia.com/Pain_Mechanisms. Last accessed April 2020.
Daniel Murrell, MD on April 12, (2017) — Written by Neel Duggal Available: https://www.healthline.com/health/somatic-vs-visceral-pain#overview1. Last accessed April 2020.
Deborah Weatherspoon, PhD, RN, CRNA on October 12, (2017) — Written by Ian Franks Available: https://www.healthline.com/health/nociceptive-pain. Last accessed April 2020.
WebMD. (2019). Pain Management Terms. Available: https://www.webmd.com/pain-management/glossary-pain-management. Last accessed April 2020.
Figures:
♦Figure 1: Schematic drawing by us {Adapted from International Association for the Study of Pain (IASP-1986)}
♦Figure 2: Hand drawn figure by us {Adapted from: 1. Walter J. Jermakowicz, Ian D. Hentall, Jonathan R. Jagid, Corneliu C. Luca, James Adcock, Alberto Martinez-Arizala, Eva Widerström-Noga. (2017). Deep Brain Stimulation Improves the Symptoms and Sensory Signs of Persistent Central Neuropathic Pain from Spinal Cord Injury: A Case Report. Frontiers in Human Neuroscience. 11 (177). 2. Michael H. Ossipov, Gregory O. Dussor, Frank Porreca. (2010). Central modulation of pain. The Journal of Clinical Investigation. 120 (11), 3779-3787. 3. Dureja, Gur & Iyer, Rajagopalan & Das, Gautam & Ahdal, Jaishid & Narang, Prashant. (2017). Evidence and consensus recommendations for the pharmacological management of pain in India. Journal of Pain Research. Volume 10. 709-736.}
♦Figure 3: Hand drawn figure by us {Adapted from David Julius, Allan I. Basbaum. (2001). Molecular mechanisms of nociception article. NATURE. 413, 203-210 }
♦Figure 4: Schematic drawing by us {Adapted from Woolf and Salter Science 2000:288:1765}