THE ROLE OF HYPOXIA/OXYGEN IN THE TREATMENT OF TUMORS
Introduction
Hypoxia is the deficiency of oxygen in the body, and low oxygen tension (pO2) defines tumour hypoxia with pO2<10mmHg (Bredell et al, 2016). As a tumour develops, it will rapidly outgrow its blood supply (Brown and Bicknell, 2001). Abnormalities of the newly formed blood vessels (neovascularization) can cause malfunction creating a hypoxic environment, which is related to malignant progression and resistance to treatment such as chemotherapy and radiation (Brown and Bicknell, 2001). Therefore, tumour hypoxia is important in the prognosis of the disease in survival rate and also the expected disease-free time. It is important to know how the cancer cells change under these conditions, so we understand the impact they have on different therapeutic methods (Moen and Stuhr, 2012) . Figure 1 shows the main effects occurring in the tumour during hypoxia.

Figure 1 The main effects of Hypoxia (Mckenna et al, 2018)
HIF-1
Birner et al (2000) describes HIF-1 (hypoxia inducible factor 1) as a transcription factor made of an alpha and a beta subunit. The alpha subunit is oxygen regulated, which means that the alpha subunit will determine HIF-1 activity. This transcription factor is essential for tumour growth and progression, and can thus be used in prognosis of the disease, because it is known that a strong HIF-1 alpha expression will lower the survival rate and decrease the disease-free time (Birner et al, 2000).
Oxidative stress
Oxidative stress is caused by reactive oxygen species (ROS), which are oxygen radicals that damage DNA, causing mutations and then later malignant progression (Brown and Bicknell, 2001). Tumour cells are known to overproduce ROS (Brown and Bicknell, 2001). The oxidative stress cause resistance to apoptosis, which cause treatment failure (Brown and Bicknell, 2001). Therapies like chemotherapy and radiotherapy are dependent on apoptosis as a response to oxidative stress and ROS induced DNA damage caused by the treatment (Brown and Bicknell, 2001).
VEGF and angiogenesis
Jain et al (2007) describes that the growth of both primary and metastatic tumours relies on their own ability to take over the host vessels, forming new vessels (from preexisting vessels) by angiogenesis and/or by recruiting bone-marrow-derived cells (vasculogenesis). Vascular endothelial growth factor (VEGF) has a major role in neovascularization, and can stimulate these tumors to form new blood vessels (Jain et al 2007). These formed vessels ends up being anatomically and physiologically abnormal and contributes to a hostile microenvironment. This microenvironment present increased interstitial fluid pressure and decreased oxygen tension, which leads to increased lethality and even more malignant phenotype (Jain et al (2007).
Types of treatment
Hyperbaric oxygen treatment
Hyperbaric oxygen treatment (HBO) is used for treating hypoxia and ischemia (lower oxygen level than normal), to increase the amount of dissolved oxygen in the blood plasma and the oxygen delivery to the tissues (Moen and Stuhr, 2012) . The administration of HBO is 100% oxygen at a higher than normal atmospheric pressure (Moen and Stuhr, 2012).
HBO in relation to cell death, shows that hyperoxia over a longer period of time elevate the reactive oxygen species (ROS) (Moen and Stuhr, 2012). To ensure the survival of the cells during oxygen treatment, cell type, concentration of oxygen used and the duration of the exposure should be carefully monitored (Moen and Stuhr, 2012).
Moen and Stuhr, 2012 explains that angiogenesis in tumours is an important factor for growth and metastasis. HBO has shown to have an antiangiogenic effect in mammary tumour models and in glioma. At the same time, several other studies showed no particular change in angiogenesis with oxygen treatment (Moen and Stuhr, 2012).
A recent study showed that HBO leads to a mesenchymal to epithelial transition, reducing the aggressiveness of the tumours phenotype in mammary tumours, therefore also reducing the metastasis and invasiveness of the cells (Moen and Stuhr, 2012).
Research studies shows that HBO has an effect on some types of cancer, reducing growth rate of tumours. This was shown in breast cancer, while bladder and cervical cancer did not show any difference in growth rate after HBO treatment. HBO did not show the ability to cure cancer as the only method of therapy, but it can be a powerful supplement to conventional therapy in some types of cancer (Moen and Stuhr, 2012).
Radiation Therapy
Radiation therapy uses ionizing radiation to kill cancer cells in two ways; direct and indirect. Directly it can kill cells by damaging the DNA, and indirectly it damages the water molecules in the cells, which leads to production of free radicals (Desouky et al, 2015). Free radicals are small, independent molecules that contains an extra electron which makes the free radicals very reactive to other molecules (Desouky et al, 2015).
Rockwell et al (2009) showed that cells that are well supplied with oxygen makes the radiation more effective, and the range of DNA damage and killing cancer cells is high. In hypoxic areas the radiation is half as effective, which enables some cancer cells to survive radiation therapy, and this is one of the reason for patients with cancer to receive radiation therapy in several cycles (Rockwell et al, 2009). Almost all cancer patients receives radiation therapy at some point in their treatment, and the ability for hypoxic cancer cells to resist the radiation is a serious problem (Rockwell et al, 2009). The hypoxic cancer cells that do survive- can lead to recurrence of the tumor and, in worst case, development of and even more aggressive tumor phenotype (Rockwell et al, 2009). Figure 2 Shows how radio sensitivity declines when tumor pO2 is <25-30mmHg.
Harrison et al (2004) showed that hypoxia may generate tumor resistance to radiation therapy directly and indirectly. Directly it induce tumor resistance through the elimination of molecular oxygen. Indirectly it stimulates or inhibits post transcriptional effects and gene expression, and by that change the cell-cycle position or numbers of cells existing in the G0-phase of cell division (Harrison et al, 2004).

Figure 2 Radiosensitivity (Harrison et al, 2004) |
Chemotherapy
Chemotherapy is the use of drugs to treat a disease (Moen and Stuhr, 2012). This kind of therapy will be able to work in the whole body, so it will be a good way to reach not only the primary growth site, but also reach metastasized tumour cells (Harrison et al, 2004).
Altered cellular metabolism can reduce the chemicals cytotoxicity, some substances need a sufficient supply of oxygen to be maximally cytotoxic (Moen and Stuhr, 2012). Lack of oxygen will also make the availability of the tumour less efficient, and thus the administration can be affected. Use of hyperbaric oxygen treatment could increase the tumour perfusion and the cellular sensitivity to the drugs (Moen and Stuhr, 2012). Since the tumour is harder to reach through the circulation when in hypoxic conditions, there have been research on bioreductive chemotherapeutic drugs targeting hypoxic cells (Mckenna et al, 2018). Hypoxia activated prodrugs (HAPs) are reduced and activated in hypoxic conditions, and will therefore target the hypoxic regions in the body. A useful HAP will have the ability to reach hypoxic cells, have features that makes it easy to metabolise, and have a long lasting effect on tumour cells (Mckenna et al, 2018). This strategy combined with radiation or conventional chemotherapy could be a good strategy to treat tumours (Mckenna et al, 2018).
Surgery
During surgery the tumour and surrounding tissue is removed. Its immediate efficiency will not be altered by the effects of hypoxia and ROS, but as cancer is known to spread quicker and more frequently under these conditions, surgery as treatment will still have a higher risk of failure compared to non-hypoxic and ROS affected cancer types (Höckel et al, 1996).
The role of Hypoxia in Cancer types
Vaupel et al (2007) posted a clinical study describing detection and characterization of tumor hypoxia using Eppendorf pO2 Histography in various organs. Figure 3 shows the organs they studied - normal vs tumor hypoxia, and most of these cancer types will be focused on throughout this text.

Figure 3 Tissue oxygenation (Vaupel et al 2007) |
Pancreatic cancer
About 85% of the pancreatic tumors develops in the exocrine tissues of the pancreas, and around 5% in the endocrine tissues (Ilic, 2016). Vast majority of the tumors developing in the exocrine tissue is know as Pancreatic Adenocarcinoma, and they develop in the epithelial cells lining the pancreatic ducts (Ilic, 2016). These tumors usually form in the head and neck of the pancreas, but sometimes also in the tail (Ilic, 2016).
In Figure 4 Erkan et al (2015) shows the complex relationship between pancreatic cancer cells and the pancreatic stromal/stellate cells generating hypoxia in pancreatic cancer tissue, and initiating a cascade of events. These events will lead to the stromal/stellate cells forming a dense extracellular matrix (ECM) that reduces capillary function, and the pancreatic cancer cells to secrete antiangiogenic factors that will limit new vessel formation (Erkan et al, 2015). The combination of these two events leads to lack of blood flow- which results in formation of hypoxic areas within the tumor tissue of the pancreas (Erkan et al, 2015). Hypoxia-inducible-factor-1 (HIF-1) initiates first as a response to hypoxia, which further heighten the stromal/stellate cell to create a vicious cycle which leads to severely hypoxic areas throughout the tumor tissue (Erkan et al, 2015). HIF-1 also mediate adaptive responses of pancreatic cancer cells, which allows the cells to survive by improved aerobe glycolysis, inhibition of apoptosis and constant proliferation whilst increasing the aggressiveness of the disease through maintenance of cancer stem cells (CSC), invasion/metastasis and treatment resistance (Erkan et al, 2015).

Figure 4 Hypoxia in Pancreatic Cancer (Erkan et al, 2015)
Pancreatic cancer has a very poor prognosis because it is very invasive and has a rapid progression (Stocken et al, 2008). Pancreatic cancer is one of the deadliest types of malignant carcinoma and is typically diagnosed at a late stage, with a 3% 5-year survival rate in the US (Li et al, 2018). For the best chance at long term survival surgery is the best option, but chemotherapy and radiation therapy is also used (Li et al, 2018).
Prostate cancer
Hypoxia in prostate cancer tumours occurs early during the tumour development, and are related to the more aggressive phenotypes of prostate cancer (Mckenna et al, 2018). The Hypoxia and hypoxia-related biomarkers are associated with the progression of the disease, and also failure of treatment (Mckenna et al, 2018).
As shown in Figure 5, under hypoxic conditions several signalling pathways are activated in the tumour cells. Some of the activated factors include HIF, PI3K/Akt/mTOR, NOX (NADPH oxidase), Wnt/ β-catenin and Hedgehog (Mckenna et al, 2018). These pathways are communicating and ensuring the tumour cells survival in the harsh hypoxic conditions, inducing formation of blood vessels -angiogenesis, rapid reproduction of the cells, stemness, spread and further growth (Mckenna et al, 2018). The cancerous cells will also do a basic transformation – ependymal to mesenchymal transition. This transition is leading to cancer cells with a more invasive or metastatic phenotype (Mckenna et al, 2018).
Therapy options are surgery, radiation therapy, hormone therapy, chemotherapy or a combination. Under hypoxic conditions there is harder to reach the tumour cells in an adequate way, since the 02 pathways are limited. A way around this could be chemotherapy that targets hypoxic cells (Mckenna et al, 2018).
Surgery is a good option, but the metastasis have to be under control to remove enough of the tumour cells. In radiotherapy, the primary factors leads to radio resistance, and the radio sensitivity declines with lower 02 levels (Harrison et al, 2004)
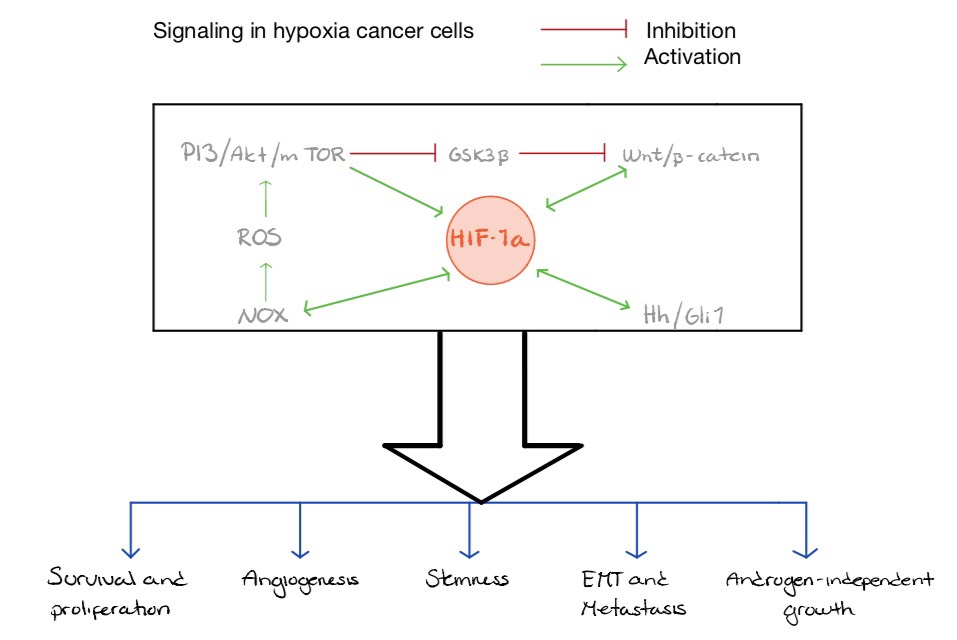
Figure 5 Hypoxia in Prostate cancer (Deep et Panigrahi, 2015)
Cervical cancer
20-35% of all cervical cancer patients are expected to die from their disease (Höckel et al, 1996). Hypoxic tumour types are known to increase this percentage, caused by the more aggressive phenotypes developed due to hypoxic induced development of the tumour cells, which will affect the spread and life expectancy of the disease (Höckel et al, 1996). The strengthened resistance of hypoxic tumour cells will lead to a decrease in responsiveness to radiotherapy and chemotherapy, which are typically used in cervical cancer treatment (Höckel et al, 1996).
Höckel et al (1996) describes how hypoxia is known to enhance the genetic diversity of the cancer cells. Evolution will therefore develop aggressive phenotypes typical for hypoxic tumour cells, such as the increase of growth of the primary tumour, increased spread to the connective tissue of the uterus and increased frequency of lymph-vascular spread.
HIF-1 alpha used in early prognosis of cervical cancer HIF-1 alpha stabilizes the tumour suppressor protein p53, which causes cell death (Birner et al, 2000). In cervical cancer, p53 is usually inactivated by the viral oncoprotein E6 leading to further stimulation of the HIF-1 alpha expression, which will affect the tissues response to treatment as the cancer suppressing proteins does not show significant activity (Birner et al, 2000). ‘
Breast cancer
Brown and Bicknell (2001) suggests that oxygen radicals give an important indication of the prognosis, and therefore explains how antioxidants are important in therapy, as they can antagonize the effect of ROS. If antioxidants are proven effective in the treatment of breast carcinoma, it would be very interesting since they are a low toxicity substance (Brown and Bicknell, 2001).
The insufficient blood supply of breast carcinoma cells will cause low glucose levels (Brown and Bicknell, 2001). Pyruvate supplies will decrease when glucose levels are low, so the cell will no longer to be able to decompose the oxygen radicals, which enhance the accumulation and damage further (Brown and Bicknell, 2001).
Brown and Bicknell (2001) also describes possibilities of how oxygen stress can aid tumour spread, as it causes easier detachment of the cell from the basal membrane, and increased permeability in the microenvironment of the tumour, and can thus spread through the blood or lymph easier. This vascular spread is also promoted further in breast carcinoma by increasing HIF-1 alpha levels which promotes VEGF production and further spread to surrounding lymph nodes, and by increased blood supply through vasodilation activation (Brown and Bicknell, 2001).
Brain cancer
Brain tumors can be categorized by their primary site location, which can be supratentorial or infratentorial tumors (Jain et al, 2007). The tumors are named after the cell type involved, eg: Astrocytoma, which is a tumor formed by mutated astrocytes. Glioblastoma is a type of astrocytoma that is the most common and aggressive malignant primary type of adult brain tumor, and it is found in the cerebral hemisphere (Jain et al, 2007).
Jain et al (2007) showed that pervasive hypoxia is one thing that characterizes glioblastomas, and that it is uniformly fatal, despite radiotherapy, chemotherapy and surgery. Researchers have found out that anti-VEGF therapies can be effective in the treatment of glioblastoma because it can, for a little while, bring the tumor vessels back to normal (Jain et al, 2007). This means that the usage of anti-VEGF in glioblastoma can optimize the combination of chemotherapeutics and radiation as treatment (Jain et al, 2007).
Hyperbaric oxygen (HBO) treatment has shown to reinforce normoxia in hypoxic regions in brain tumors (Graham et al 2018). Graham et al (1996) explained in their article that one study showed glioblastoma treated with HBO and radiotherapy improved survival, but at the same time another study showed that it can form complications such as necrosis and seizures, so this is a exiting field but it still need more research.
Conclusion
Those tumour cells who survive hypoxic stress will have an increased multiplication rate, causing increased oxygen deficiency in the body. The reproduction of these cells will further enhance the cells ability to cope with the low-oxygen environment, which will make the tumour cells a more dominant type, becoming more difficult to treat with their improved ability of survival and more aggressive spreading. The transcription factor HIF-1 will also make the treatment more difficult, as a strong HIF-1 alpha expression will lower the survival rate and decrease the disease-free time (Birner et al, 2000).
Some ways to counteract these responses in the body can be oxygen treatment, or targeted chemotherapy to reach the tumour cells in an efficient way. It is shown that different types of cancer need different kinds of therapy. The same therapy method does not give the same result in every case.
Therapies like chemotherapy and radiotherapy are dependent on apoptosis, and as the oxidative stress cause resistance to apoptosis, hypoxia can lead to treatment failure.
Understanding the role of oxygen and hypoxia in the treatment of different cancer types is crucial to create an optimal treatment plan, as they are both factors known to alter the way different treatments would work under normal conditions.
References
Birner, P.; Schindl, M.; Obermair, A.; Plank, C.; Breitenecker, G.; Oberhuber, G. (2000): Overexpression of Hypoxia-inducible Factor 1a Is a Marker for an Unfavorable Prognosis in Early-Stage Invasive Cervical Cancer. Cancer Res 60: 4693-4696
Bredell, M. G.; Ernst, J.; El-Kochairi, I.; Dahlem, Y.; Ikenberg, K.; Schuman, D. M. (2016): Current relevance of hypoxia in head and neck cancer. Oncotarget 7: (31) 50781-50804
Brown, N. S.; Bicknell, R. (2001): Hypoxia and oxidative stress in breast cancer Oxidative stress: its effects on the growth, metastatic potential and response to therapy of breast cancer. Breast Cancer Res 3: 323–327
Desouky, O.; Ding, N.; Zhou, G. (2015): Targeted and non-targeted effects of ionizing radiation. Journal of Radiation Research and Applied Sciences 8: 247-254
Erkan, M.; Kurtoglu, M.; Kleef, J. (2015): The role of hypoxia in pancreatic cancer: a potential therapeutic target, Expert Review of Gastroenterology & Hepatology 10: (3) 301-316
Graham, K.; Unger, E. (2018): Overcoming tumor hypoxia as a barrier to radiotherapy, chemotherapy and immunotherapy in cancer treatment. International journal of nanomedicine vol 13: 136049-6058.
Harrison, L.; Blackwell, K. (2004): Hypoxia and anemia: Factors in decreased sensitivity to radiation therapy and chemotherapy. The oncologist 9: 31–40
Höckel, M.; Schienger, K.; Aral, B.; Milze M.; Schäffer, U.; Vaupel, P. (1996): Association between Tumor Hypoxia and Malignant Progression in Advanced Cancer of the Uterine Cervix. Cancer Res 56: 4509-4515.
Ilic, M.; Ilic, I. (2016): Epidemiology of pancreatic cancer. World J Gastroenterol 22: (44) 9694-9705.
Jain, R. K.; Tomaso, E. D.; Duda, D. G.; Loeffler, J. S.; Sorensen, A. G.; Batchelor, T. T. (2007): Angiogenesis in brain tumors. Nature Reviews Neuroscience 8: 610-622
Li, W.; Liu, H.; Qian, Q.; Cheng, L.; Yan, B.; Han, L.; Xu, Q.; Ma, Q.; Ma, J.(2018): Hyperglycemia aggravates microenvironment hypoxia and promotes the metastatic ability of pancreatic cancer. Comput Struct Biotechnol Journal 16: 479–487.
McKenna, D. J.; Errington, R; Pors, K (2018): Current challenges and opportunities in treating hypoxic prostate tumours. JCMT journal 4: 1-13
Moen, I; Stuhr, L. (2012): Hyperbaric oxygen therapy and cancer – a review. Targeted oncology 7: (4) 233–242
Raa, A.; Stansberg, C.; Steen, V. M.; Bjerkvig, R.; Reed, R. K.; Stuhr, L. EB. (2007): Hyperoxia retards growth and induces apoptosis and loss of glands and blood vessels in DMBA-induced rat mammary tumors. BMC Cancer 7: 23
Rockwell, S.; Dobrucki, I. T.; Kim, E. Y.; Marrison, S. T.; Vu, V. T. (2009): Hypoxia and radiation therapy: Past history, ongoing research, and future promise. Current molecular medicine 9: (4) 442-458
Stocken, D. D.; Hassan, A. B.; Altman, D. G.; Billingham, L. J.; Bramhall, S. R .; Johnson, P. J.; Freemantle, N. (2008): Modelling prognostic factors in advanced pancreatic cancer. British Journal of Cancer 99: 883-893
Vaupel, P.; Höckel, M.; Mayer, A.(2007): Detection and Characterization of Tumor Hypoxia Using pO2 Histography. Antioxidant Redox Signal 9: (8) 1221-1235
Figures
Figure 1. Self-drawn figure, adapted from: Mckenna D.; J.; Errington, R; Pors, K. (2018): Current challenges and opportunities in treating hypoxic prostate tumours. JCMT journal 4: 1-13
Figure 2. Self-drawn figure, adapted from: Harrison, L; Blackwell, K. (2004): Hypoxia and Anemia: Factors in Decreased Sensitivity to Radiation Therapy and Chemotherapy. The Oncologist 9: (5) 31-40
Figure 3. Self-drawn figure, adapted from: Vaupel, P.; Höckel, M.; Mayer, A. (2007): Detection and Characterization of Tumor Hypoxia Using pO2 Histography. Antioxidant Redox Signal 9: (8) 1221-1235
Figure 4. Self-drawn figure, adapted from: Erkan, M.; Kurtoglu, M.; Kleef, J. (2015): The role of hypoxia in pancreatic cancer: a potential therapeutic target?, Expert Review of Gastroenterology & Hepatology 10: (3) 301-316
Figure 5. Self-drawn figure, adapted from: Deep, G; Panigrahi, G. K. (2015): Hypoxia-induced signaling promotes prostate cancer progression: exomes role as messenger of hypoxic response in tumor microenvironment. Crit Rev Oncog. 20(5-6):419-434
