Anti-inflammatory effects of theophylline
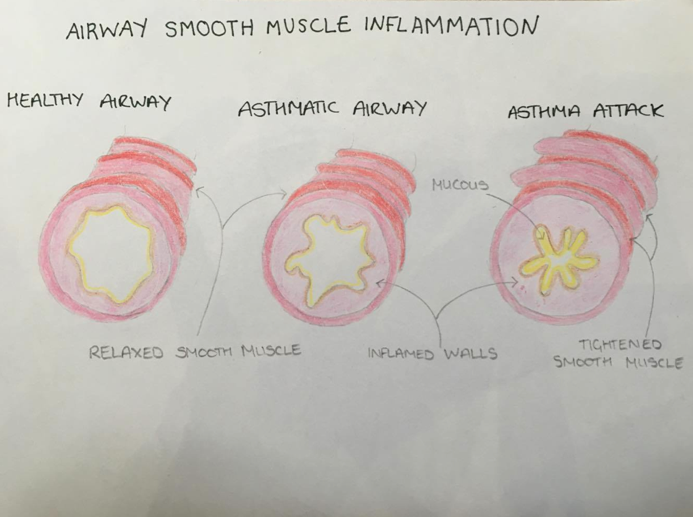
Theophylline, also known as 1,3-dimethylxanthine, is a methylxanthine drug used in therapy for respiratory diseases such as chronic obstructive pulmonary disease and asthma under a variety of brand names. Asthma is “a chronic (long term) lung disease that inflames and narrows the airways. Asthma causes recurring periods of wheezing, chest tightness and shortness of breath, and coughing.” (http://www.nhlbi.nih.gov/health/health-topics/topics/asthma) Formula: C7H8N4O2
Contents
- Anti-inflammatory effects of theophylline
Anti-inflammatory
Anti-inflammatory simply is the property of a certain substance, for example a drug, that is able to reduce inflammation and/or swelling. As asthma is a lung disease that inflames and narrows airways through the act of swelling this is where theophylline as an anti-inflammatory drug takes effect.
|
Use as a Bronchodilator
Theophylline is known for it’s ability to work as a bronchodilator meaning that it is a drug that is able to widen the bronchi which will in results decrease the resistance in the airflow to the lungs. Even though it is shown that theophylline has bronchodilator activity “it is becoming increasingly apparent that this drug also possesses anti-inflammatory and immunomodulatory activity.” (Spina et al, 1998) Henry Hyde Salter in 1860 drew the conclusion that caffeine was a bronchodilator. Therefore as theophylline has a similar chemical structure to caffeine it was used as a treatment for asthma in 1922.
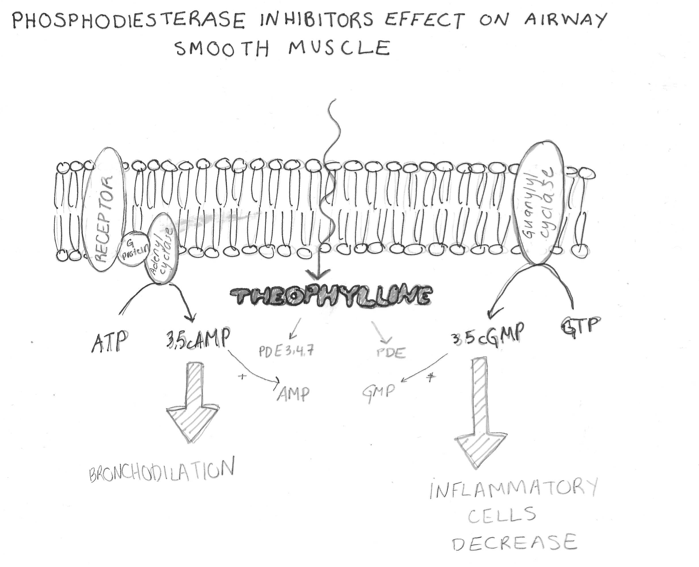
One way that the theophylline works is by inhibiting the breakdown of the second messengers by xanthine which is a major part of the structure of theophylline. These second messengers are cyclic AMP and cyclic GMP. AMP stands for adenosine monophosphate and GMP for guanosine monophosphate. When the breakdown of AMP and GMP occur this will lead to the airway smooth muscle relaxation and therefore has a positive effect on the curing of asthma. Another mechanism that has been brought forward is that theophylline is able to raise intracellular cAMP and CGMP levels through the inhibition of PDE (phosphodiesterase). By doing so it relaxes the smooth muscle in the airway passages and also inhibits inflammatory cell activation. Even though theophylline is not a very strong inhibitor of phosphodiesterase it works because it has also been shown that the PDE levels in animals with atropic disease, one of these being asthma and therefore there will be a stronger response from the theophylline because of the increased levels of PDE. (Banner et al, 1996)
|
Theophylline is currently used as a bronchodilator in asthma therapy. Theophylline is able to directly relax human airway smooth muscle in vitro and, like β2-agonists, acts as a functional antagonist, preventing and reversing the effects of all bronchoconstrictor agonists. The bronchodilator effect of theophylline in human airways is reduced by charybdotoxin, which selectively inhibits large-conductance Ca2+-activated K+ channels (maxi-K channels), suggesting that theophylline opens these maxi-K channels via an increase in cAMP. Theophylline is a relatively weak bronchodilator with a median effective concentration of 1.5 × 10−4 M in vitro, which equates to a plasma concentration of 67 mg/L, assuming 60% protein binding.
Use in Treatment for Patients with Chronic Obstructive Pulmonary Disease
Chronic Obstructive Pulmonary Disease is a type of obstructive lung disease which disrupts the normal airflow to the lungs and therefore results in poor airflow. In order to investigate inflammation in chronic obstructive pulmonary disease we look at induced sputum. Sputum is the phlegm and saliva that is coughed up from the lower airways which include the trachea and the bronchi. Neutrophil proportion, interleukin and myeloperoxidase are all factors that are shown in the induced sputum of chronic obstructive pulmonary disease patients. Low doses of theophylline reduce the total number and proportion of neutrophils in induced sputum, the concentration of interleukin (IL)-8, and myeloperoxidase and neutrophil chemotactic responses, which suggests that it may have an anti-inflammatory effect. The antiinflammatory effects of theophylline are seen at concentrations less than 10 mg/L, which is below the dose at which significant clinically useful bronchodilatation is evident.
|
Effect on Transcription
Theophylline has its primary effect on transcription through the proinflammatory transcription factor nuclear factor (NF)-kB. This is a protein complex that has a role in the transcription of DNA. When this is done incorrectly, or the regulation of it is not controlled it can result in inflammation. Theophylline prevents the translocation of the proinflammatory transcription factor nuclear factor (NF)-κB into the nucleus, which will therefore result in minimizing the chances of inflammation like in asthma and chronic obstructive pulmonary disease.
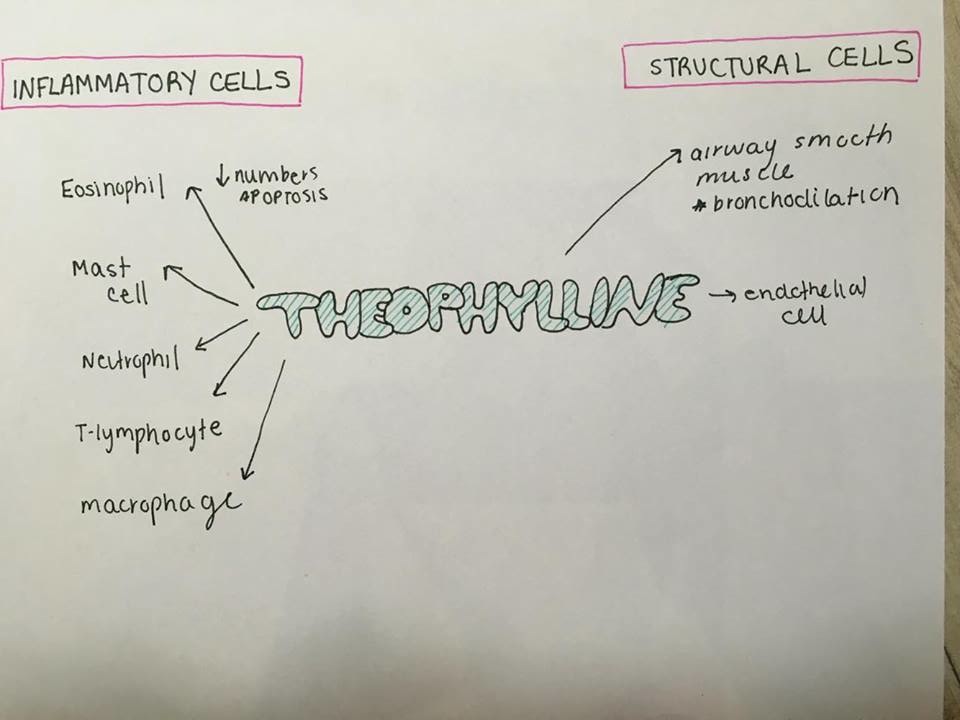
Effects on Apoptosis
Apoptosis is a process of programmed cell death that occurs in multicellular organisms. Apoptosis in neutrophils in vitro is promoted by Theophylline. Eosinophils are reduced in the anti-apoptotic protein Bcl-2 via Theophylline-induced apoptosis. PDE inhibition does not mediate this effect, but it may be caused by the antagonism of adenosine A2A receptors. Apoptosis in T lymphocytes results in the reduction of their cell life, this is also induced by Theophylline. So the apoptosis of T lymphocytes appears to be mediated via PDE inhibition.
Effects on Immune cells
Both the activation and accumulation of eosinophils are of equal importance at inflammatory sites. It’s been found that chronic treatment with PDE4 inhibitors reduced the levels of eosinophil peroxidase (maker of eosinophil activation)in the bronchoalveolar lavage fluid after an allergen challenge. (Spina et al 1998) Theophylline also has a role in inhibiting T-cell proliferation following antigenic and mitogenic stimulation. (Banner et al, 1996 ) Inflammations reduced as the activated T-lymphocytes are the only cell type that directly recognize and respond to processed antigens. They then regulate the production of IgE’s by B cells and act in the recruitment of other inflammatory cells to the site, such as eosinophils.
Theophylline also effects the eosinophils that reach the inflammatory site. It reduces the release of some toxic and pro inflammatory mediators from the eosinophils. E.G. Reactive oxygen species (ROS) and basic proteins.
Similar results have also been shown with neutrophils, inhibiting the release of ROS which damage the airways and intensify inflammation.
Theraputic levels of theophylline can also inhibit the tumoricidal activity of natural killer cells. (Banner et al, 1996)
Effects on HDAC
The activation of HDAC,is caused by Theophylline. Hence the expression of inflammatory genes are surpressed by Theophylline. Histone de-acetylase (HDAC) is directly activated, resulting in the de-acetylation of core histones which have been acetylated by the Histone Acetyltransferase (HAT) activity of co-activators such as CBP (cAMP-responsive element-binding [CREB] protein). Therapeutic concentrations of Theophylline provide this effect, but it is lost at higher concentrations (10−4 M). Resulting in non-selective HDAC inhibitor Trichostatin A blocking it. Ergo, concentrations of 10−6–10−5 M are used to prevent this occurrence. The activity of HDAC activity significantly in the bronchial biopsies of patients with asthma after they’ve been treated with these low doses of theophylline (the mean plasma concentration is about 5 mg/L). Thus proving that low therapeutic concentrations of Theophylline are sufficient to activate HDAC in vivo.
The Difference between Theophylline and Corticosteroids
The effect of Theophylline and Corticosteroids are very different. Due to the effect of Theophylline which is observed in the NF-κB–immunoprecipitated inflammatory gene complexes from nuclear extracts, it is believed that there is a relatively direct activation of HDAC. However, due to a lot of other nuclear proteins which are co-precipitated in inflammatory gene complexes, it is not proven whether HDACs are the direct target of Theophylline. The effects of corticosteroids are due to recruitment of HDAC2 to the active transcription site. However this is without the direct effect on HDAC activation. Thus contrasting with Theophyllines effects. The overall effects of Theophylline are relatively small. Only three quarters of Theophylline increases the activity. However, it has been shown that by using a Chromatin Immunoprecipitation Assay that this can significantly reduce histone-4 acetylation at the granulocyte-macrophage colony-stimulating factor promoter when targeted by dexamethasone When histones are in resting state they are acetylated. Small differences in the number of acetylated histones result in relatively large biophysical changes. Ergo, only miniscule alterations in the quantity of acetylated lysines on histone tails can rapidly switch a gene from an inactive to an active state and vice versa. Theophylline activates different subtypes of HDAC, having an equal activation in both HDAC1 and HDAC2. Whereas there appears to be a relatively selective effect on Class I HDACs, with less effect on Class II HDACs.
Side effects
The most common side effects of theophylline are headaches, nausea and gastrointestinal issues. These may be caused by the inhibition of specific PDE’s. E.g. Inhibition of PDE4 in the vomiting center. Other side effects can be caused by adenosine receptor antagonism. Mainly of the A1 receptors. This inhibition can be avoided by using selective PDE inhibitors. Side effects caused by adenosine antagonism and PDE inhibitors are most common when theophylline is used in higher concentrations. At plasma concentrations of 10-20 mg/L side effects in patients were relatively common and treatment had to be discontinued, however at the lower concentration of 5-10 mg/L side effects were largely avoided.
Effects of Theophylline compared to Other Phosphodiesterase Inhibitors
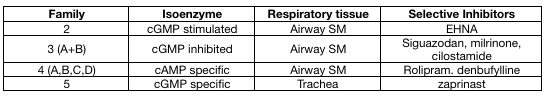
Theophylline is used in the treatment of asthma and other pulmonary diseases because of its bronchodilator, anti-inflammatory and immunomodulatory activity. Theophylline effects the airways because it is involved in the inhibition of phosphodiesterase (PDE) enzymes. Phosphodiestereases are a diverse group of enzymes that are classified into at least 7 groups, which can be inhibited by a number of different chemicals.
|
Rolipram is another phosphodiesterase inhibitor used to reduce the severity of asthma attacks. Tests on rabbits that were immunized at birth show that both theophylline and rolipram failed to alter acute bronchospasm following challenge with Alternaria tenuis in allergic rabbits. However both of the drugs attenuated eosinophilia in bronchoalveolar lavage fluid 24hr following allergen challenge. (Spina et al, 1998) This shows that these PDE inhibitors can reduce bronchoconstriction reducing the severity of asthma attacks. When challenged with the same fungus rolipram significantly inhibited bronchial hyper-responsiveness (easily triggered contraction on the bronchioles) further demonstrating this class of drugs ability to reduce severity of asthma attacks. Theophylline did not have such effects. Other studies showed in guinea pigs airway wall oedema and extravasation of plasma protein can be inhibited by administering theophylline via infusion or via the intratracheal route. (Spina et al, 1998) The oedema and plasma protein extra-vasation is induced by a variety of inflammatory cells. Theophylline reduces the inflammation levels hence the oedema and extravasation.
Future developments
Theophylline is currently the only anti-inflammatory drug available for patients with COPD as corticosteroids are ineffective in reducing inflammation and other PDE4 inhibitor usually have frequent side effects. Theophylline is an attractive drug the treatment of COPD because of its ability to reduce airway inflammation at low doses, reducing the occurrence of possible side effects. As the molecular mechanisms of Theophylline’s anti-inflammatory effects are now better understood, there is a strong rationale for combining low-dose theophylline and corticosteroids in an inhaled medication for treatment of airway diseases, especially COPD. It is possible that the combined use of Theophylline and corticosteroids will allow the therapeutic ratio of corticosteroids administered to patients to be increased. It’s predicted that although corticosteroids anti-inflammatory effects are mediated by HDAC, theophylline may enhance recruitment whilst avoiding steroid side effects. Because corticosteroids side effects are mainly mediated by gene induction, with HDAC mediating the anti-inflammatory effects. If corticosteroid sensitivity in COPD patients can be restored by using low dose Theophylline combined with inhaled or oral corticosteroid treatment may be effective in reducing inflammation and maybe even in reducing disease progression.
Another very useful property of theophylline is that it becomes more effective as oxidative stress increases. This property allows the treatment of all stages of COPD with the same dose of drug.
Theophylline’s effects on HDAC activation is one of the drugs most important mechanisms in the design of new drugs, especially since it is independent of the mechanisms of most side effects. This ability can be used to design theophylline-like molecules to be used as drugs to activate HDAC whilst avoiding adenosine receptor antagonism and PDE inhibition. These drugs would then allow larger dosages to be used because of the lack of side effects. Theophylline is only an activator of HDAC at low concentrations, at high concentrations it acts as a partial agonist. So it is also being used as a start molecule in the search for other agonist molecules with greater efficiency.High throughput screening is being used to look for molecules that mimic the effects of theophylline. This could lead to the development of new anti-inflammatory drugs to use with corticosteroids in the treatment of diseases such as COPD, severe asthma and even atherosclerosis.
References
Banner, Katharine H., and Clive P. Page. "Anti-inflammatory Effects of Theophylline and Selective Phosphodiesterase Inhibitors." Clinical and Experimental Allergy 26 (1996): 2-9. Web.
Barnes, P. J. (2005, January). Theophylline in Chronic Obstructive Pulmonary DiseaseNew Horizons. Retrieved April 23, 2016, from http://www.atsjournals.org/doi/full/10.1513/pats.200504-024SR#.Vw1kytTOqrV
Sampson, A. P., & Church, M. (1999). Anti-inflammatory drugs in asthma.
Spina, L. D., J. Landells, and C. P. Page. "The Role of Theophylline and Phosphodiesterase4 Isoenzyme Inhibitors as Anti-inflammatory Drugs." Clinical and Experimental Allergy (1998): 24-30. Web.
Spina, L. D., J. Landells, and C. P. Page. "The Role of Theophylline and Phosphodiesterase4 Isoenzyme Inhibitors as Anti-inflammatory Drugs." Clinical and Experimental Allergy (1998): 24-34. Web.
"What Is Asthma?" - NHLBI, NIH. Web. 25 Mar. 2016.