|
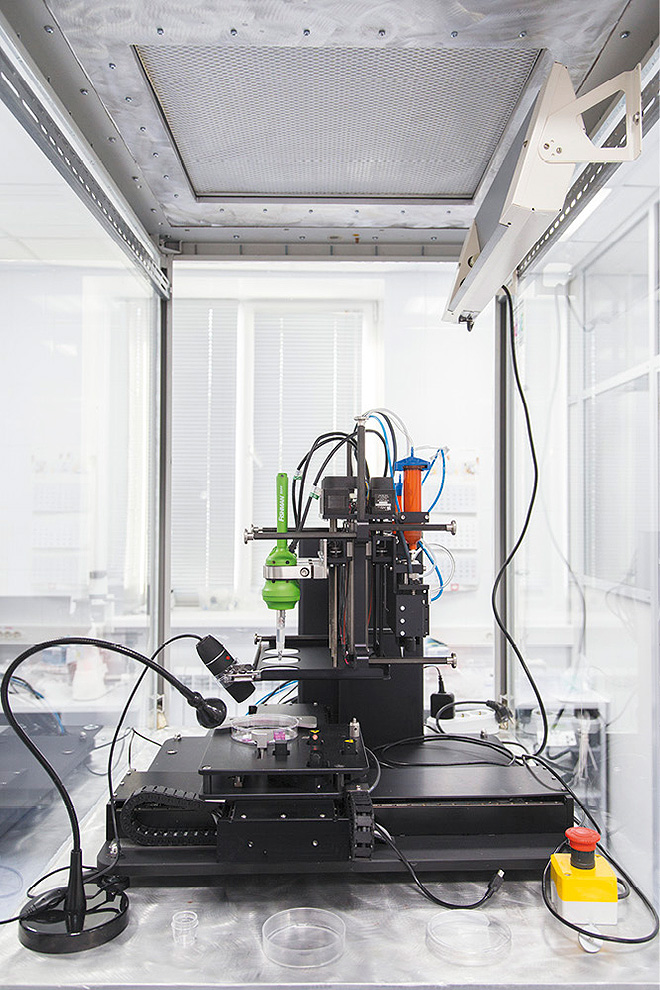
Figure 1: 3D bioprinter developed by |
Medical uses of 3D printing
3D printing is the process in which three-dimensional (3D) objects are literally "printed out", layer by layer, until an object is formed. Using this process, 3D printing is able to achieve extreme levels of accuracy and complexity. While makers often like to talk about 3D printing (3DP) manufacturing breakthrough, no one can deny that 3D printers (Figure 1) are actually being used to develop revolutionary medical applications at an amazing pace. 3DP has been applied in medicine since 2000s, when it was first used to make dental implants and custom prosthetics. [Cui et al., 2012] Since then, applications have evolved considerably due to constant evolution and newly developed material, which fit the need of patients and reduce rejection risks. Other medical fields such as surgical organ implants, replacement and reconstruction, have now also embraced the use of 3DP. It is also an ethical alternative for medical research and the testing of drugs and toxicology.
General 3DP uses many material such as ABS plastic, PLA, polyamide (nylon), glass filled polyamide, stereolithography materials (epoxy resins), silver, titanium, steel, wax, photopolymers and polycarbonate. When it comes to the medical field, the chosen material depends on its applications. Cell cultures and stem cells have been used to grow “personalised material” such as blood vessels, vascular networks, tissues, and organs. The Combination of Sciences and digital technologies is pushing the limits of 3DP to our imagination.
Contents
1. Orthodonty
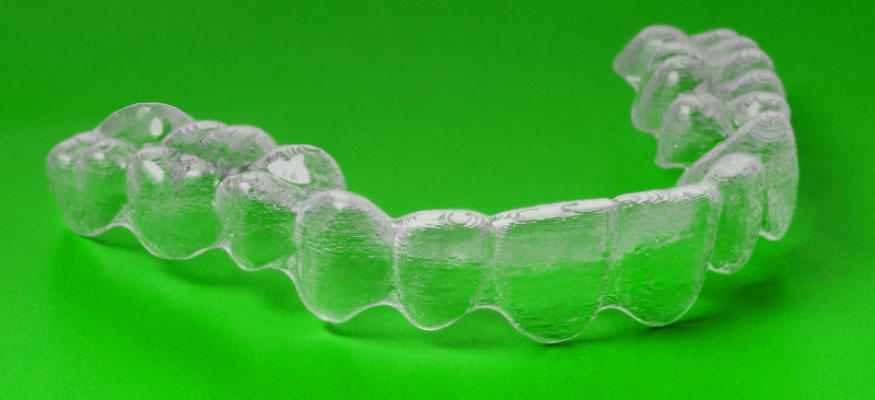
Dentistry was the first medical field to enthusiastically embrace 3DP. Before 3D technologies reached this market, dental implants and dentures were made by a milling machine that cut them out of a solid block of polymer: not always entirely accurate, and certainly not very fast. The advent of 3DP has been a revolution for dentistry. It brought in the best possible accuracy, unmatched by traditional methods. Dentists are now able to print new teeth or braces on-site and on-demand (figures 2 and 3) instead of sending them to labs. This has greatly reduced treatment time for patients.
|
Figure 2: 3D printed brace. |
1.1. Tooth and Brace printing
A patient’s mouth is digitally scanned and stored on a computer. The file is manipulated with CAD (Computer aided design) software to precisely measure and design the necessary tooth or brace. When ready, the file is sent to the 3D printer which creates the tooth/brace in minutes (figures 2 and 3) allowing the patient to complete the intervention in a single visit. Digital files are stored onsite or hosted on the cloud. A patient's dental history is only a click away, and the thousands of plaster molds stored in offices and labs have disappeared.
|
Figure 3: model of a fixed partial denture (bridge) |
1.2. What’s next?
Rapid evolution of 3DP is pushing dentistry past creating crowns and dentures; the future material of dental prints will be made of ammonium salts mixed into dental resin. Ammonium salts fight bacteria that cause infections and tooth decay. This antimicrobial plastic has been developed to eventually manufacture a variety of 3D-printed, bacteria-zapping dental appliances, right in the dentist’s office. Tests have been successful against harmful bacteria, however, the American dental association (ADA) doubts that the resin will kill every single one of the many species of bacteria present in the mouth. Most “good bacteria”, necessary for oral health, shall not be harmed. Broader tests needs to be done on the ammonium salt treated teeth in order to determine their durability when exposed to saliva, toothpaste, and other factors. Once these "enhanced" dental products successfully hold up to the rigors of clinical trials, they will become the latest innovation for the industry. [Yue et al., 2015]
2. Prosthetics
One of the most common uses of 3DP in the medical and veterinary fields is the making of custom fitted prosthetics. CT scans are used to make a tomography of the patient’s anatomy, allowing the printed prosthetic to be customised with great precision and in a variety of materials.
|
Figure 4: Derby the dog, running on 3D printed |
2.1. Prosthetic limbs
3DP is used to create cheaper and better fitting prosthetics for amputees. “Bespoke Innovations” (San Francisco) uses a scan of the patient’s intact limb to design a tailored symmetric prosthetic leg; thereby improving walking abilities thanks to a perfect balance between the two limbs. Then, they use the scan to create "fairings" to dress the prosthetics, and help patient to better accept their new limb.
Prosthetics are also printed for animals who underwent amputation or are suffering from deformities. “Derby the dog” (Figure 4) was born with deformed front limbs; functional only down to the elbow. His condition limited his motion and made running impossible. Derby’s owner first tried a dog wheelchair, which kept him from certain terrains and limited his interaction with other dogs. Consequently, prosthetic legs had to be made for Derby. “3D systems” used scans of Derby’s legs to create two unique prosthetics: personalised to his handicap and range of motion. The custom legs are a flexible loop-design printed by a multi-substance 3D printer. They have allowed Derby to run without difficulty from the very moment he wore them.
|
Figure 5: 'Terminator' turtle gets a 3D printed |
2.2. 3DP saves endangered wildlife
A logger-head sea turtle was brought to the “Research, Rescue, and Rehabilitation Centre” (Pamukkale University in Turkey) after he collided with a boat propeller, and the right side of his head was badly injured. CT scans of the turtle were sent to “BTech Innovations” who created a custom titanium beak and jaw (Figure 5). Titanium is lightweight, strong, and rust-resistant which makes it the ideal material. Without it the turtle could not have survived on its own. The prosthetics were successfully implanted and no signs of rejection were observed.
Several other prosthetic stories have shown how 3DP saves injured birds who otherwise would have had no chance of surviving. Most have damage to their beak. In February 2016, Gigi the Macaw received a titanium beak after she was rescued from the illegal exotic bird trade. She is the first to have received such treatment. Gigi recovered quickly from the intervention and adapted to her new beak, thanks to which she can eat solid food on her own.
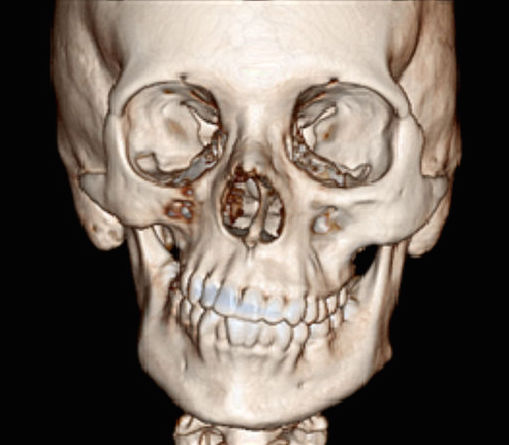
3. Help for better planning, time and cost effective surgery
In some instances, 3D printed objects are not aimed at being used on the patient; but rather at helping health technicians to better evaluate the injury or malformation. Coupled with CT scans, the patient’s anatomy is closely mapped through CAD software and reproduced by a 3D printer. This allows surgeons to appropriately plan the intervention, thereby greatly lowering the risk of complications. This use of 3DP is expected to make reconstruction easier, quicker, and cheaper. [Bardet et al., 2015]
|
Figure 6: metal plate placed and adjusted on the |
3.1. Bone Fracture repair or congenital bone deformation
Using the computed MRI scan, an acrylic model of the injured area is reproduced by a 3D printer. The reproduced bones allow for a more exact diagnosis of a possible fracture or inherited malformation, and allow the surgeon to choose the right equipment prior to surgery. Metal plates, for instance, are adapted (bent) to the 3D model so it fits perfectly with the patient’s bone shape and size, as well as being catered to their specific needs (for example, bone fracture). (Figure 6) Screw zones can also be carefully picked on the 3D model without the regular visibility restrictions of the surgical area. With careful planning, using the precise 3D-printed bone model, the surgical approach is made easier and the intervention is quicker and more precise. In some malformations, such as radius curvus, the combined use of angled rotation centers, MRI, and acrylic 3D models gives an accurate assessment of bone deformities which otherwise could not have been obtained. With these innovative methods, a precise pre-surgical strategy can be created for large bone defects, allowing them to be fixed in a single intervention. [Bardet et al., 2015]
3.2. Cartilage/ bone replacement
In these kinds of interventions the injured or missing organ needs to be replaced by similar tissue taken from another part of the body. Needless to say that the material supply is limited and precious. For example, in ear replacement surgery, cartilage is harvested from the rib cage and immediately carved into the replacement ear. The allowance for time and tolerance of errors in this sort of sensitive procedure is very low. Before the appearance of 3DP, surgeons would practice carving the needed shape on materials such as soap, fruits, pig cartilage, etc. Training material rarely had the size, consistency, or characteristics necessary for a true preparation. A better solution came with a low cost, 3D print cartilage model close to the look and feel of human cartilage. This enables surgeons to practice the procedure with a superior training material and better efficiency.
4. Organ implants
Tissue or organ failure, diseases, accidents, and birth defects are critical medical problems. Current treatments rely mostly on organ transplants from living or deceased organ donors who need to be a perfect “match”. [Cui et al., 2012] While the global population is aging and previously unseen diseases appear, 3DP brings an alternative to (the lack of) organ donations or appropriate medication. It is a revolutionary step in the world of medicine. 3DP now allows the use of biocompatible materials, cells, and other biological components to print complex structures, such as tissues and organs, destined for organ transplantation. Scientists have so far been able to create several kinds of tissues including multi-layered skin, bone, vascular tissue, tracheal splints, heart tissue, and cartilaginous structures. [Murphy and Atala, 2014] One innovative solution involves using a cell sample from the patient to grow a replacement organ, minimizing the risks of tissue rejection and a lifelong need of immunosuppressants. [Schubert et al., 2014] Even though 3DP is taking over the "industry" with unique, custom-made, better-fitted 3D printed implants, successful procedures are still followed by months or even years of painful recovery and rehabilitation.
4.1. Soft tissue implants
In the first stages of soft tissue 3DP trials, the tissue was collapsing in on itself before the printing was even complete. Through many innovations and trials, this issue has eventually been solved by using a slurry of gelatin to support the tissue or organ as it is being printed. Once the printing is complete the gelatin is melted away in room-temperature water and the finished tissue is able to support itself.
4.1.1. New material
A vastly used 3DP technique is the "Two-photon polymerization". It creates small, detailed objects from several types of photoreactive liquid precursors. These precursors contain light-reactive chemicals that turn the liquid into a solid polymer. Unfortunately, most of these chemicals are toxic and might cause complications when used in a medical implant. An alternative to these toxic chemicals has been found in riboflavin (vitamin B2): both nontoxic and biocompatible. It is mixed with a precursor material to make it photoreactive and is then used to create medical implants from non-toxic polymers. [Nguyen et al., 2013] This discovery brought into light many more biocompatible materials which can be used in the 3D printing of implants.
|
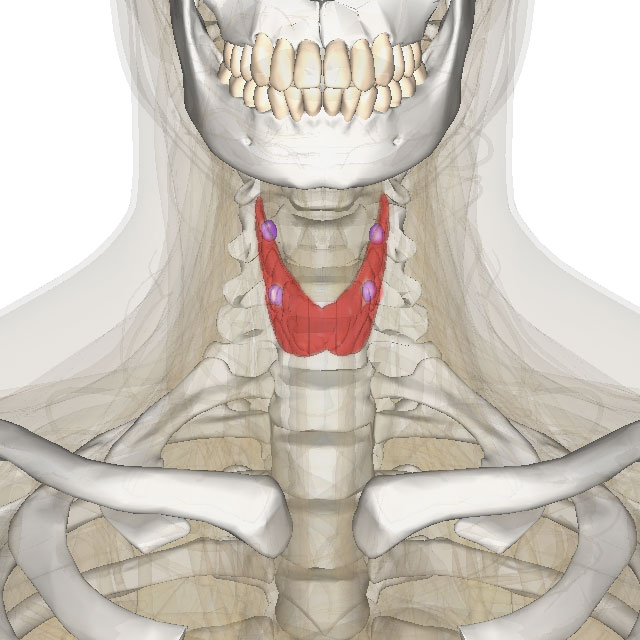
Figure 7: thyroid/parathyroid in color |
4.1.2. Printing Organs
In March 2011, Anthony Atala, M.D. (Director of the Wake Forest Institute for Regenerative Medicine) demonstrated the 3DP of a kidney from a solution of living cells; it was however lacking the necessary tubules and blood vessels to make it functional. Researchers had first tried printing the kidney layer by layer, leaving holes for the vessels and tubules. Unfortunately, this led to a lack in the structural stability needed to withstand blood pressure. The main issue with creating functional organs is that living cells need to be within 150-200 microns of a capillary to survive. Ongoing research is working on solving the problem and creating the incredibly small spaces needed for the blood supply within the 3D printed organ, along with the structural stability necessary to withstand normal blood pressure.
3D printing techniques have also been used to build a new human ear. The auricle, printed from a collagen based material, was injected with a gel made of living cells, which grew into cartilage and replaced the collagen mold within 3 months. Up until now, replacement ears have been built from a more styrofoam-like material or, as seen earlier, from cartilage harvested from the patient's own ribs. This bioengineering advancement pushes the field of 3DP and tissue engineering towards the ability to print entirely printed organs. [Reiffel et al., 2013]
In march 2015, a thyroid gland was successfully reproduced and transplanted into a mouse. This specific organ (Figure 7) was chosen due to its relative simplicity, with the hope that, later on, other organ transplants would be possible once the technology allows it. The mouse’s own stem cells (from fat tissue) were used as primary material in order to prevent rejection. The Thyroid gland's mature cells are grown using a three-directional robot, which drips fabric layers of the living stem cells through an automated syringe. Before printing, the cells were transformed into ‘spheroids’ (layered cells) and then placed in hydrogel to enable the printing process. After printing, the organ was placed in a bioreactor to dissolve the gel and the finished thyroid organ was left to mature on its own before the surgical implant.
|
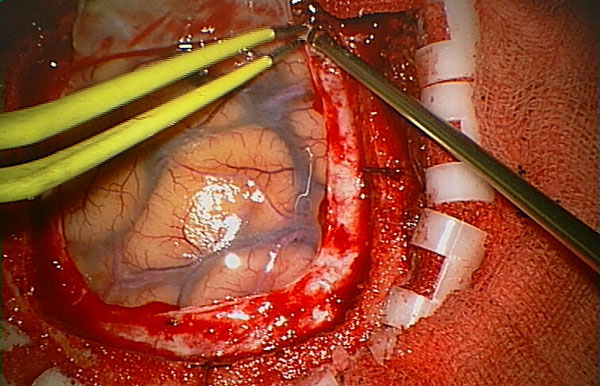
Figure 8: Surgery on the brain. |
4.1.3. Dura Mater
The brain is protected by a layer called dura mater, which can be divided into superficial and meningeal layers. In surgery, these layers are cut open in order to access the brain at the site of operation (Figure 8). Upon completion of the surgery, The dura mater must be closed up by a suture and onlay procedure. “Maipu Regenerative Medical Technology” has developed a method of 3D printing using a substance they call “Redura”. Printed directly onto the surgical site, “Redura” provides a suitable environment for the cells and tissues to regenerate. Within 2 months the meningeal tissue grows back and the “Redura” begins to dissolve into two natural, non-toxic components: water and carbon dioxide. “Redura” is used in hospitals globally and has been successfully applied in over 10 000 patients without any reported adverse effects.
4.2. Bones and cartilage implants
|
Figure 9: Porous bone. |
A broken bone can regenerate but it cannot regrow after being crushed or destroyed by cancer. It also cannot be easily replaced by another material and its exact characteristics have, so far, been impossible to reproduce synthetically because of several unique properties: strong, rigid, light, and porous (Figure 9) all at once. [Roohani-Esfahani et al., 2016] This is why they are the second most transplanted tissue in the world (after blood). So far, surgeons have been using segments of the patient’s own skeleton (autografts). Bones from cadavers can also be used (allografts) as well as various ceramics or metallic alloys. The use of autografts limits availability, while other options can result in rejection by the organism. 3DP technologies have become extremely useful in the constantly growing field of osteology and arthrology. They allow significant advances in synthetic bone implants. Many different materials have been developed to mimic bone characteristics and the use of patient-specific imaging data makes it possible to print bone implants specific to each individual. The latest research and discoveries have already contributed to replacing the use of metal altogether. Implants will eventually be made entirely from biocompatible materials that can be broken down by the body.
4.2.1. Cartilage repair
Cartilage is a poorly irrigated tissue. Once damaged, it never regenerates, and defects may lead to osteoarthritis (in adults). This repair incapacity could be solved by tissue engineering. The challenge lies in that the optimum scaffold must be able to reproduce the natural extracellular matrix, fulfill cartilage functions in the early stage of the implant process, and induce the natural regeneration of the tissue.
Hydrogels are attractive 3DP biomaterials for the repair of articular cartilage. They have the potential to help with regeneration as they share several common features with the organism's extracellular matrix and allow cell encapsulation in a highly hydrated and mechanically supportive 3D environment. Hydrogels also allow efficient and homogeneous cell seeding, pipetted directly onto the scaffold structure. Hydrogels can provide chemical and physical biologically-relevant signals while being printed in various shapes and with various biomechanical characteristics. However, they still need to be optimized to ensure proper cell survival conditions, while respecting physico-chemical requirements for the biofabrication process. This challenge is well on its way to being solved, thanks to the development of novel hydrogel-based bioinks. This method is used in parallel with multi-material biofabrication approaches in order to construct intricate, stable 3D structures. This provides the cells with a biologically suitable environment, whilst matching the harsh in-vivo mechanical conditions. [Malda, 2015]
|
Figure 10: 3D reconstruction of the CT scan |
4.2.2. Bone implants
High-precision 3D printers can steadily manufacture solid bone, one layer at a time. Artificial bones were initially developed to replicate complex bones such as the pelvis or spine. They were printed from titanium and used on patients with bone tumors or after surgical resection. The main advantage is that 3DP recreates the exact skeletal structure of any patient, enabling the development of a 3D scaffold with the perfect shape and size for implantation. The skeleton area in need of reconstruction is CT scanned and a 3D image is created (Figure 10). The image is then used to calculate the shape of the personalized bone piece and the implant is then printed out using one of several developed techniques and accompanying material. The race for discoveries has been pushing numerous universities, researchers, and manufacturers to concentrate their efforts on the development of the latest breakthrough to make bone implants safer, quicker, and cheaper. It has become a very competitive market and grows at a very fast pace for veterinary and human use alike.
4.2.2.1. Allograft material
Bones have been successfully printed from a material composed of very fine bone powder and biological glue. The allograft bone powder is made from other animals of the same species, theoretically increasing the chances of biological compatibility (in comparison to metal implants). The 3DP process consists of the layering of minuscule layers of bone powder followed by bio-glue (around 0.1 mm of bone-glue-bone-glue layers). This process requires thousands of layers to form a very detailed structure and is limited as to print sizes. Bones cannot exceed 15 cm because this form of printing is not as strong as original bones, causing long bones to lose sturdiness. Moreover, the biocompatibility problem still remains and rejections still exist.
4.2.2.2. Synthetic material
It has been a challenge to make a synthetic bone material that has the porosity (allowing blood and cells to go through it) as well as the mechanic strength to match the bony structure. Nevertheless, a few processes have been developed to create synthetic bones that are even stronger than the real thing. Synthetic bone is printed using a 3D printer capable of using two synthetic polymers in an optimized geometric pattern. The hierarchical structures, giving strength to the natural composite, are self-assembled through electrochemical reactions. The Geometric pattern used for 3D print are based on those seen in natural material such as bone or nacre, but also include new designs not existing in nature. The composite fracture behavior is similar to bone, but with 22 times more fracture-resistance than its strongest constituent material. This makes it a much more resilient material than natural bone. [Dimas et al., 2013]
Another printable material has been developed to be hundred times stronger than current synthetic materials. By studying properties of the skeleton, such as collagen and calcium, a new ceramic material has been made to copy all the structural and functional aspects of bones. Its strength and porosity are very similar to natural bone: strong enough to withstand the pressure of use, but porous enough to allow blood and cells to pass through it. In addition, it is capable of encouraging the regeneration of new bone cells in the correct position. The ceramic is bioactive and contains seed cells, resembling natural bone, which are eventually replaced by natural bone in the body due to the healing process. It is also well accepted by the body (no rejection), making it a particularly interesting material, far superior to other synthetic counterparts. [Roohani-Esfahani et al., 2016]
4.2.2.3. Autograft made differently
After the treated area has been scanned and calculated, a 3D scaffold is printed using only the mineral parts of animal bones, meaning that the bones are stripped from all their cellular material. Stem cells are then extracted from a fat sample taken from the patient. The cells are injected into the printed shape and placed under human body conditions using a bioreactor (temperature, pH, etc.). Using this method they can essentially grow bones. In 3 weeks time the new bone is completed and the animal bone scaffolding is removed, leaving an implant which is completely made of the patient’s own cells. This helps to avoid the risks of rejection. So far (2016) this procedure has only been applied on animals, but will soon be used on humans. The procedure could be used for bone reconstruction, where it is especially important to reduce the risk of complications.
4.2.2.4. Anti-rejection material: the 3D printing revolution
When an implant needs replacement or removal several years after its implantation due to rejection, it is another trauma caused to the patient. Fortunately, a developed material, made from a calcium polyphosphate powder similar to bone, is bio-absorbable and ultimately replaces fresh tissue. The new bones and custom joints are printed using a powder-deposition printing technique, then heated to become completely solid and implantable. Though more and more biocompatible 3D materials are developed, calcium polyphosphate is actually so compatible that new bone will grow directly into the implant. Over time the implant is completely replaced with new bone, not only diminishing the need for additional surgery, but optimizing recovery as well. The project has been in development since 2008 and animal testing is starting in 2016. Several challenges still need to be overcome before human applications, but once trials are complete, the principle can be applied to just about every necessary implant - including knees, hips, shoulders and ankles. [An et al., 2016]
4.2.2.5. Stronger implant
Improving the strength of 3D printed bone implants could help patients who have suffered significant bone loss to recover much faster. A novel 3D printing process involves manipulating and freezing the growth crystals within a 3D printed material. Crystals grown in sub-zero temperatures might provide a viable solution to improve the strength of 3D printed bones while retaining the structure's porosity. A micro-computed tomography image of the sample bone scaffold is used on 3D printing combined with freezing. This can significantly reduce the fabrication time and cost of such medical devices. The secret behind the toughness of many biological materials is the way their components are arranged from the molecular level all the way up to the macro level. Using this design strategy could help engineer bone scaffolds whose porosity does not compromise their strength.
5. References
- Bardet J. F.; Bordelo J. P. A. (2015): Passavin P. Radius Curvus. Synthese Vétérinaire. 359: 22-24.
- Bartlett S. (2013): Printing organs on demand. Lancet Respir Med 1(9): 684.
Cui X.; Boland T.; D’Lima D. D.; Lotz M. K. (2012): Thermal inkjet printing in tissue engineering and regenerative medicine. Recent Pat Drug Deliv Formul 6(2): 149–155.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3565591/- Klein G. T.; Lu Y.; Wang M. Y. (2013): 3D printing and neurosurgery—ready for prime time? World Neurosurg 80(3-4): 233–235.
- Dimas L. S.; Bratzel G. H.; Eylon I.; Buehler M. J. (2013): Tough Composites Inspired by Mineralized Natural Materials: Computation, 3D printing, and Testing. Advanced functioning material. 23(36):4629-4638
An L.; Guang-huai X.; Miao S.; Hui-feng S.; Chi-yuan M.; Qing G.; Zhong-ru G.; Shi-gui Y.; Yan-ming L.; & Yong H. (2016): 3D Printing Surgical Implants at the clinic: An Experimental Study on Anterior Cruciate Ligament Reconstruction. Scientific Reports. 6, 21704.
http://www.nature.com/articles/srep21704- Malda J. (2015): The application of 3D hydrogel printing technology for cartilage regeneration. European Cells and Materials. 30(1): 3.
Murphy S. V.; Atala A. (2014): 3D bioprinting of tissues and organs. Nature Biotechnology. 32: 773–785
http://www.nature.com/nbt/journal/v32/n8/full/nbt.2958.htmlNguyen A. K.; Gittard S. D.; Koroleva A.; Schlie S.; Gaidukeviciute A.; Chichkov B. N.; Narayan R. J. (2013): Two-photon polymerization of polyethylene glycol diacrylate scaffolds with riboflavin and triethanolamine used as a water-soluble photoinitiator. Future medicine. 8(6): 725-738.
http://www.futuremedicine.com/doi/abs/10.2217/rme.13.60?journalCode=rme&Schubert C.; Van Langeveld M. C.; Donoso L. A. (2014): Innovations in 3D printing: a 3D overview from optics to organs. British Journal of Ophthalmology. 98(2): 159–161.
http://bjo.bmj.com/content/98/2/159.full.pdf- Reiffel A. J.; Kafka C.; Hernandez K. A.; Popa S.; Perez J. L.; Zhou S., Pramanik S.; Brown B. N.; Ryu W. S.; Bonassar L. J.; Spector J. A. (2013): High-Fidelity Tissue Engineering of Patient-Specific Auricles for Reconstruction of Pediatric Microtia and Other Auricular Deformities. PLoS ONE 8(2): e56506. doi:10.1371/journal.pone.0056506
Roohani-Esfahani S. I.; Newman P.; Zreiqat H. (2016): Design and fabrication of 3D printed scaffolds with a mechanical strength comparable to Cortical bone to repair large bone defects. Scientific Reports. 6, 19468. DOI: 10.1038/srep19468
https://www.researchgate.net/publication/291387600Yue J.; Zhao P.; Gerasimov J. Y; Van De Lagemaat M.; Grotenhuis A.; Rustema-Abbing M.; Van Der Mei, H. C.; Busscher H. J.; Herrmann A.; Ren Y. (2015): 3D-Printable Antimicrobial Composite Resins. Advanced Functional Materials. 25(43): 6756–6767.
http://onlinelibrary.wiley.com/doi/10.1002/adfm.201502384/abstract;jsessionid=5FFB7E24256829D25461181357006B9E.f04t04
6. Websites
3D printing makes digital dentistry happen
http://www.stratasys.com/industries/dentalSummit S. (2011): Beautiful artificial limbs.
https://www.ted.com/talks/scott_summit_beautiful_artificial_limbsCustom prosthetics by bespoke innovation.
http://www.jebiga.com/custom-prosthetic-legs-bespoke-innovations/Latest News. (2015): 'Terminator' turtle gets a 3D printed titanium jaw.
https://www.youtube.com/watch?v=5HtnDLRQCc4ABC News Australia. (2016): 3D-printed titanium beak gives Brazilian macaw Gigi chance to crunch food for first time
http://www.abc.net.au/news/2016-02-25/titanium-beak-gives-macaw-chance-to-crunch-food/7198934Langston J. (2015): 3-D printing techniques help surgeons carve new ears.
http://www.washington.edu/news/2015/09/30/3-d-printing-techniques-help-surgeons-carve-new-ears/3D systems. "Derby the Dog, running on 3D prosthetics" (2015)
https://youtu.be/uRmoowIN8aYCNN. (2015): Grow human bone from fat.
http://edition.cnn.com/videos/tech/2015/10/30/orig-pioneers-epibone-human-bones-from-fat.cnn/video/playlists/pioneers-orig/3D bone printing project in China to enter animal testing stage (2015)
http://www.3ders.org/articles/20150715-3d-bone-printing-project-in-china-to-enter-animal-testing-stage.htmlGrunewald S. J. (2016): New Research into 3D Printed Bone Implants Could Change the Way We Heal Broken Bones.
https://3dprint.com/118059/3d-printed-bone-implants/Zavyalova V. (2015): Honey, I printed a thyroid gland
http://rbth.com/longreads/bioprint/index.htmlStephen Feller (2016): Scientists 3D-print bone structure to help tissue regenerate
http://www.upi.com/Health_News/2016/02/08/Scientists-3D-print-bone-structure-to-help-tissue-regenerate/3221454937055/Biomimetic-Synthetic-absorbable dural substitute (2015)
http://web.ros-medical.com/public/uploads/files/biologicos/Folleto_ReDura.pdfAtala A. Printing a human kidney (2011)
https://www.ted.com/talks/anthony_atala_printing_a_human_kidney
7. Figures
- Андрей Ильин [CC0 or CC0]. Wikimedia Commons
- Jestin, C. "3D printed Dental brace". 2016. Own work.
Coronation Dental Specialty Group. [CC BY-SA 3.0]. Wikimedia Commons.
3D systems. "Derby the Dog, running on 3D prosthetics". 2015. YouTube Video.
Latest News. "'Terminator' turtle gets a 3D printed titanium jaw". 2015. YouTuve Video.
- Jestin, J.C. "Aovet congress". 2016. Own work.
BodyParts3D is made by DBCLS (Polygondata is from BodyParts3D). "thyroid/parathyroid in color against skeleton and various organs". [CC BY-SA 2.1]. Wikimedia Commons.
- Anonymous. "Craniotomy_Arachnoid". 2006. Wikimedia commons.
patrick siemer from san francisco, usa. "bone" [CC BY 2.0]. Wikimedia Commons.
Desherinka. Personnal work. [CC BY-SA 3.0]. Wikimedia Commons.
8. Further reading (and Watching)
Duhaime-Ross A. (2016): This 3D bioprinter can make human-sized ear, muscle, and bone tissues
http://www.theverge.com/2016/2/15/10995730/3d-print-human-tissue-ear-muscles-boneCronin L. (2012): Print your own medicine.
https://www.ted.com/talks/lee_cronin_print_your_own_medicineSummit S. (2011): Beautiful artificial limbs.
https://www.ted.com/talks/scott_summit_beautiful_artificial_limbs