|
Size: 37433
Comment:
|
Size: 37689
Comment:
|
| Deletions are marked like this. | Additions are marked like this. |
| Line 33: | Line 33: |
| A patient’s mouth is digitally scanned and stored on a computer. The file is manipulated with [[https://en.wikipedia.org/wiki/Computer-aided_design|CAD]] (Computer aided design) software to precisely measure and design the new needed tooth or brace. When ready, the file is sent to the 3D printer which creates the tooth/brace in minutes ''(figures 2 and 3)'', allowing the patient to complete the intervention in a single visit. Digital files are stored onsite or hosted on the cloud. A patient's dental history is only a click away, and the thousands of plaster molds stored in offices and labs have disappeared. | A patient’s mouth is digitally scanned and stored on a computer. The file is manipulated with [[https://en.wikipedia.org/wiki/Computer-aided_design|CAD]] (Computer aided design) software to precisely measure and design the necessary tooth or brace. When ready, the file is sent to the 3D printer which creates the tooth/brace in minutes ''(figures 2 and 3)'' allowing the patient to complete the intervention in a single visit. Digital files are stored onsite or hosted on the cloud. A patient's dental history is only a click away, and the thousands of plaster molds stored in offices and labs have disappeared. |
| Line 45: | Line 45: |
| Rapid evolution of 3DP is pushing dentistry past creating crowns and dentures: Future prints’ material will be made of ammonium salts mixed into dental resin. Ammonium salts fight bacteria which cause infections and tooth decay. This antimicrobial plastic has been developed to eventually be used to manufacture a variety of 3D-printed bacteria-zapping dental appliances, right in a dentist’s office. Tests have been successful against harmful bacteria, and the American dental association (ADA) doubts that the resin will kill every single one of the many species of bacteria present in the mouth. Most “good bacteria” necessary for oral health, shall not be harmed. Broader tests needs to be done on the ammonium salt treated teeth in order to determine their durability when exposed to saliva, toothpaste, and other factors. Once these "enhanced" dental products successfully hold up to the rigors of clinical trials, they will become the latest innovation for the industry. ~-[[#refs|[Yue et al., 2015]|]]-~ | Rapid evolution of 3DP is pushing dentistry past creating crowns and dentures; the future material of dental prints will be made of ammonium salts mixed into dental resin. Ammonium salts fight bacteria which cause infections and tooth decay. This antimicrobial plastic has been developed to eventually be used to manufacture a variety of 3D-printed, bacteria-zapping dental appliances; right in the dentist’s office. Tests have been successful against harmful bacteria; however, the American dental association (ADA) doubts that the resin will kill every single one of the many species of bacteria present in the mouth. Most “good bacteria”, necessary for oral health, shall not be harmed. Broader tests needs to be done on the ammonium salt treated teeth in order to determine their durability when exposed to saliva, toothpaste, and other factors. Once these "enhanced" dental products successfully hold up to the rigors of clinical trials, they will become the latest innovation for the industry. ~-[[#refs|[Yue et al., 2015]|]]-~ |
| Line 55: | Line 55: |
| One of the most common uses of 3DP in the medical and veterinary fields is the making of custom fitted prosthetics. [[https://en.wikipedia.org/wiki/CT_scan|CT scans]] are used to make a [[https://en.wikipedia.org/wiki/Tomography|tomography]] of the patient’s anatomy, allowing the printed prosthetic to be customised with great precision, in a variety of materials. | One of the most common uses of 3DP in the medical and veterinary fields is the making of custom fitted prosthetics. [[https://en.wikipedia.org/wiki/CT_scan|CT scans]] are used to make a [[https://en.wikipedia.org/wiki/Tomography|tomography]] of the patient’s anatomy, allowing the printed prosthetic to be customised with great precision and in a variety of materials. |
| Line 68: | Line 68: |
| 3DP is used to create cheaper and better fitting prosthetics for amputees. [[https://www.youtube.com/watch?v=uh6fzLOYp1M|“Bespoke Innovations”]] ''(San Francisco)'' uses a scan of the patient’s intact limb to design a tailored symmetric prosthetic leg, thereby, improving walking abilities thanks to a perfect balance between the two legs.<<BR>>Prosthetic limbs are also printed for animals who underwent amputation, or suffering from deformities. [[https://youtu.be/uRmoowIN8aY|“Derby the dog”]] ''(Figure 4)'' was born with deformed front limbs, functional only down to the elbow. His motion was limited and made running impossible. Derby’s owner first tried a dog wheelchair, which kept him from certain terrains and limited his interaction with other dogs. Consequently, prosthetic legs had to be made for Derby. “3D systems” used scans of Derby’s legs, to create two unique prosthetic legs personalised to his handicap and motion: a flexible loop design, printed by a multi-substance 3D printer. His new flexible legs have been allowing Derby to run without difficulty from the very moment he wore them. | 3DP is used to create cheaper and better fitting prosthetics for amputees. [[https://www.youtube.com/watch?v=uh6fzLOYp1M|“Bespoke Innovations”]] ''(San Francisco)'' uses a scan of the patient’s intact limb to design a tailored symmetric prosthetic leg; thereby improving walking abilities thanks to a perfect balance between the two limbs.<<BR>>Prosthetics are also printed for animals who underwent amputation or are suffering from deformities. [[https://youtu.be/uRmoowIN8aY|“Derby the dog”]] ''(Figure 4)'' was born with deformed front limbs; functional only down to the elbow. His condition limited his motion and made running impossible. Derby’s owner first tried a dog wheelchair, which kept him from certain terrains and limited his interaction with other dogs. Consequently, prosthetic legs had to be made for Derby. “3D systems” used scans of Derby’s legs to create two unique prosthetics: personalised to his handicap and range of motion. The custom legs are a flexible loop design printed by a multi-substance 3D printer. They have allowed Derby to run without difficulty from the very moment he wore them. |
| Line 80: | Line 80: |
| A logger-head sea turtle was brought to the “Research, Rescue, and Rehabilitation Centre” (Pamukkale University in Turkey) after he collided with a boat propeller and the right side of his head was badly injured. CT scans of the turtle were sent to [[http://www.btech.com.tr|“BTech Innovations”]] who created a costumed [[https://www.youtube.com/watch?v=5HtnDLRQCc4|titanium beak and jaw]] ''(Figure 5)''. Titanium is lightweight, strong, and rust-resistant, which makes it the ideal material. Without it the turtle could not have survived on its own. The prosthetics were successfully implanted and no signs of rejection were observed.<<BR>> Several other prosthetic stories show how 3DP saves birds who would otherwise have no chance to survive. Beak injuries are often involved. In February 2016, [[http://www.abc.net.au/news/2016-02-25/titanium-beak-gives-macaw-chance-to-crunch-food/7198934|Gigi the Macaw]], was the first bird to receive a titanium beak after he was rescued from illegal exotic bird trade. Gigi recovered quickly from the intervention and adapted to its new beak thanks to which he can eat solid food on its own. |
A logger-head sea turtle was brought to the “Research, Rescue, and Rehabilitation Centre” (Pamukkale University in Turkey) after he collided with a boat propeller and the right side of his head was badly injured. CT scans of the turtle were sent to [[http://www.btech.com.tr|“BTech Innovations”]] who created a custom [[https://www.youtube.com/watch?v=5HtnDLRQCc4|titanium beak and jaw]] ''(Figure 5)''. Titanium is lightweight, strong, and rust-resistant which makes it the ideal material. Without it the turtle could not have survived on its own. The prosthetics were successfully implanted and no signs of rejection were observed.<<BR>> Several other prosthetic stories have shown how 3DP saves injured birds (most with damage to their beak) who otherwise would have had no chance of surviving. In February 2016, [[http://www.abc.net.au/news/2016-02-25/titanium-beak-gives-macaw-chance-to-crunch-food/7198934|Gigi the Macaw]] (the first to receive such treatment) received a titanium beak after he was rescued from the illegal exotic bird trade. Gigi recovered quickly from the intervention and adapted to her new beak, thanks to which she can eat solid food on her own. |
| Line 91: | Line 91: |
| In some instances, 3D printed objects are not aimed at being used on the patient, but help health technicians to better evaluate the injury or malformation. Coupled with CT scans, the patient’s anatomy is closely mapped through a CAD software, and reproduced by a 3D printer. This allows surgeons to appropriately plan the intervention, thereby greatly lowering the risk of complications. This use of 3DP is hoped to make reconstruction easier, quicker and cheaper. ~-[[#refs|[Bardet et al., 2015]|]]-~ | In some instances, 3D printed objects are not aimed at being used on the patient; but rather at helping health technicians to better evaluate the injury or malformation. Coupled with CT scans, the patient’s anatomy is closely mapped through CAD software and reproduced by a 3D printer. This allows surgeons to appropriately plan the intervention, thereby greatly lowering the risk of complications. This use of 3DP is expected to make reconstruction easier, quicker, and cheaper. ~-[[#refs|[Bardet et al., 2015]|]]-~ |
| Line 103: | Line 103: |
| From 3D views of the computed MRI scan, An acrylic model of the injured area is reproduced by a 3D printer. the reproduced bones allows the proper diagnostic on the possible fracture of inherited malformation and allow the surgeon to choose the right equipment prior to surgery. Metal plates, for instance, are adapted (bent) the the 3D model so it perfectly fits the patient’s bone shape and size. ''(Figure 6)'' screw zones are also carefully picked without visibility restrictions of the surgical area. Once the material is perfectly adapted the surgical approach is made easier, the intervention is quicker and more precise, contributing to a successful bone repair. In some malformation such as radius curvus, the combined use of angled rotation centers, MRI and acrylic 3D model acrylic give an accurate assessment of bone deformities that could not otherwise be obtained. With these new methods, a precise pre-surgical strategy can be planned to deal with very large bone defects that can be fixed in a single intervention. ~-[[#refs|[Bardet et al., 2015]|]]-~ | Using 3D views of the computed MRI scan, an acrylic model of the injured area is reproduced by a 3D printer. The reproduced bones allow for a more exact diagnosis of a possible fracture or inherited malformation and allow the surgeon to choose the right equipment prior to surgery. Metal plates, for instance, are adapted (bent) to the 3D model so it fits perfectly with the patient’s bone shape and size, as well as being catered to their specific needs (for example, bone fracture). ''(Figure 6)'' Screw zones can also be carefully picked from viewing the 3D model without regular visibility restrictions of the surgical area. With careful planning, using the precise 3D-printed bone model, the surgical approach is made easier and the intervention is quicker and more precise. These factors contribute to a successful bone repair. In some malformations, such as radius curvus, the combined use of angled rotation centers, MRI, and acrylic 3D models gives an accurate assessment of bone deformities which otherwise could not have been obtained. With these new, innovative methods a precise pre-surgical strategy can be created for large bone defects, allowing them to be fixed in a single intervention. ~-[[#refs|[Bardet et al., 2015]|]]-~ |
|
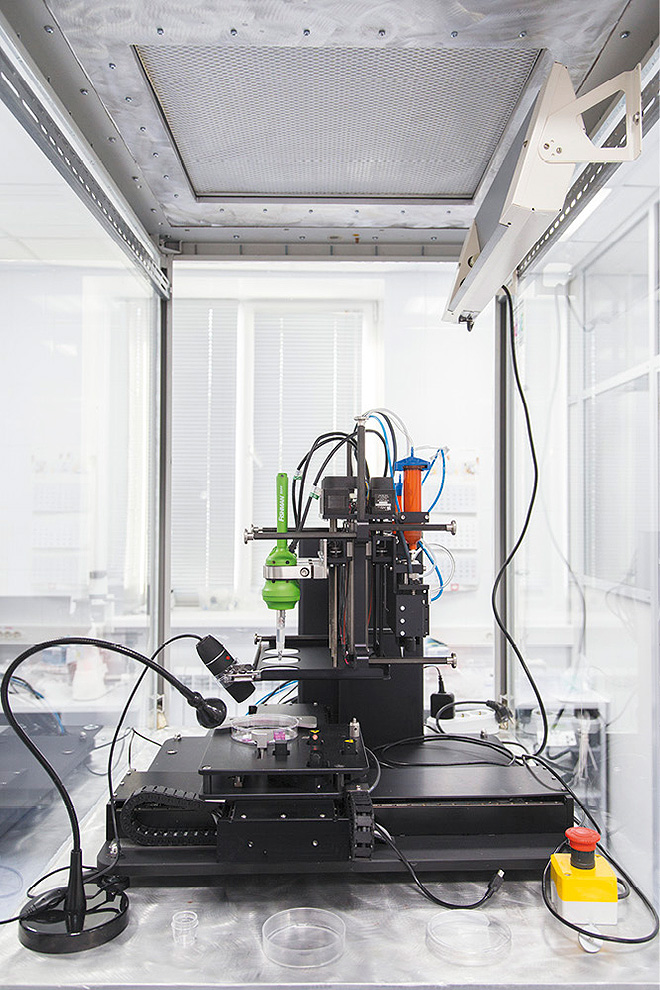
Figure 1: 3D bioprinter developed by |
Medical uses of 3D printing
3D printing is the process in which three-dimensional (3D) objects are literally "printed out", layer by layer, until an object is formed. Using this process, 3D printing is able to achieve extreme levels of accuracy and complexity. While makers often like to talk about 3D printing (3DP) manufacturing revolution, no one can deny that 3D printers (Figure 1) are actually being used to develop revolutionary medical applications at an amazing pace. 3DP has been applied in medicine since 2000s, when it was first used to make dental implants and custom prosthetics. [Cui et al., 2012] Since then, applications have evolved considerably due to constantly newly developed material fitting the need of patients and reducing rejection risks. Other medical fields such as surgical organ implants, replacement and reconstruction, have now also embraced the use of 3DP.
General 3DP uses many material such as ABS plastic, PLA, polyamide (nylon), glass filled polyamide, stereolithography materials (epoxy resins), silver, titanium, steel, wax, photopolymers and polycarbonate. When it comes to the medical field, the chosen material depends on its applications. Cell cultures and stem cells have been used to grow “personalised material” such as blood vessels, vascular networks, tissues, and organs. The use of 3D printing is also an ethical alternative for medical research and the testing of drugs and toxicology.
Contents
1. Orthodonty
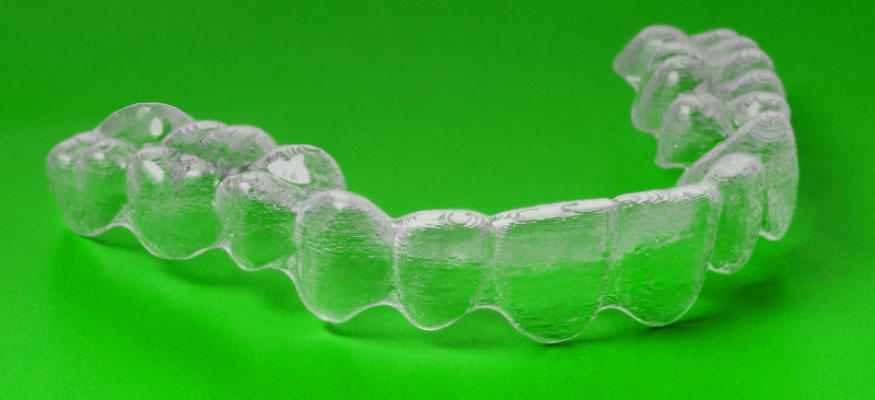
Dentistry was the first medical field to enthusiastically embrace 3DP and the digital technology. Before 3D technologies reached this market, dental implants and dentures were made by a milling machine that cut them out of a solid block of polymer: not always entirely accurate, and certainly not very fast. The advent of 3DP has been a revolution for dentistry. It brought in the best possible accuracy, unmatched by traditional methods. Dentists are now able to print new teeth or braces on-site and on-demand (figures 2 and 3) instead of sending them to labs. This has greatly reduced treatment time for patients.
|
Figure 2: 3D printed brace. |
1.1. Tooth and Brace printing
A patient’s mouth is digitally scanned and stored on a computer. The file is manipulated with CAD (Computer aided design) software to precisely measure and design the necessary tooth or brace. When ready, the file is sent to the 3D printer which creates the tooth/brace in minutes (figures 2 and 3) allowing the patient to complete the intervention in a single visit. Digital files are stored onsite or hosted on the cloud. A patient's dental history is only a click away, and the thousands of plaster molds stored in offices and labs have disappeared.
|
Figure 3: model of a fixed partial denture (bridge) |
1.2. What’s next?
Rapid evolution of 3DP is pushing dentistry past creating crowns and dentures; the future material of dental prints will be made of ammonium salts mixed into dental resin. Ammonium salts fight bacteria which cause infections and tooth decay. This antimicrobial plastic has been developed to eventually be used to manufacture a variety of 3D-printed, bacteria-zapping dental appliances; right in the dentist’s office. Tests have been successful against harmful bacteria; however, the American dental association (ADA) doubts that the resin will kill every single one of the many species of bacteria present in the mouth. Most “good bacteria”, necessary for oral health, shall not be harmed. Broader tests needs to be done on the ammonium salt treated teeth in order to determine their durability when exposed to saliva, toothpaste, and other factors. Once these "enhanced" dental products successfully hold up to the rigors of clinical trials, they will become the latest innovation for the industry. [Yue et al., 2015]
2. Prosthetics
One of the most common uses of 3DP in the medical and veterinary fields is the making of custom fitted prosthetics. CT scans are used to make a tomography of the patient’s anatomy, allowing the printed prosthetic to be customised with great precision and in a variety of materials.
|
Figure 4: Derby the dog, running on 3D printed |
2.1. Prosthetic limbs
3DP is used to create cheaper and better fitting prosthetics for amputees. “Bespoke Innovations” (San Francisco) uses a scan of the patient’s intact limb to design a tailored symmetric prosthetic leg; thereby improving walking abilities thanks to a perfect balance between the two limbs.
Prosthetics are also printed for animals who underwent amputation or are suffering from deformities. “Derby the dog” (Figure 4) was born with deformed front limbs; functional only down to the elbow. His condition limited his motion and made running impossible. Derby’s owner first tried a dog wheelchair, which kept him from certain terrains and limited his interaction with other dogs. Consequently, prosthetic legs had to be made for Derby. “3D systems” used scans of Derby’s legs to create two unique prosthetics: personalised to his handicap and range of motion. The custom legs are a flexible loop design printed by a multi-substance 3D printer. They have allowed Derby to run without difficulty from the very moment he wore them.
|
Figure 5: 'Terminator' turtle gets a 3D printed |
2.2. 3DP saves endangered wildlife
A logger-head sea turtle was brought to the “Research, Rescue, and Rehabilitation Centre” (Pamukkale University in Turkey) after he collided with a boat propeller and the right side of his head was badly injured. CT scans of the turtle were sent to “BTech Innovations” who created a custom titanium beak and jaw (Figure 5). Titanium is lightweight, strong, and rust-resistant which makes it the ideal material. Without it the turtle could not have survived on its own. The prosthetics were successfully implanted and no signs of rejection were observed.
Several other prosthetic stories have shown how 3DP saves injured birds (most with damage to their beak) who otherwise would have had no chance of surviving. In February 2016, Gigi the Macaw (the first to receive such treatment) received a titanium beak after he was rescued from the illegal exotic bird trade. Gigi recovered quickly from the intervention and adapted to her new beak, thanks to which she can eat solid food on her own.
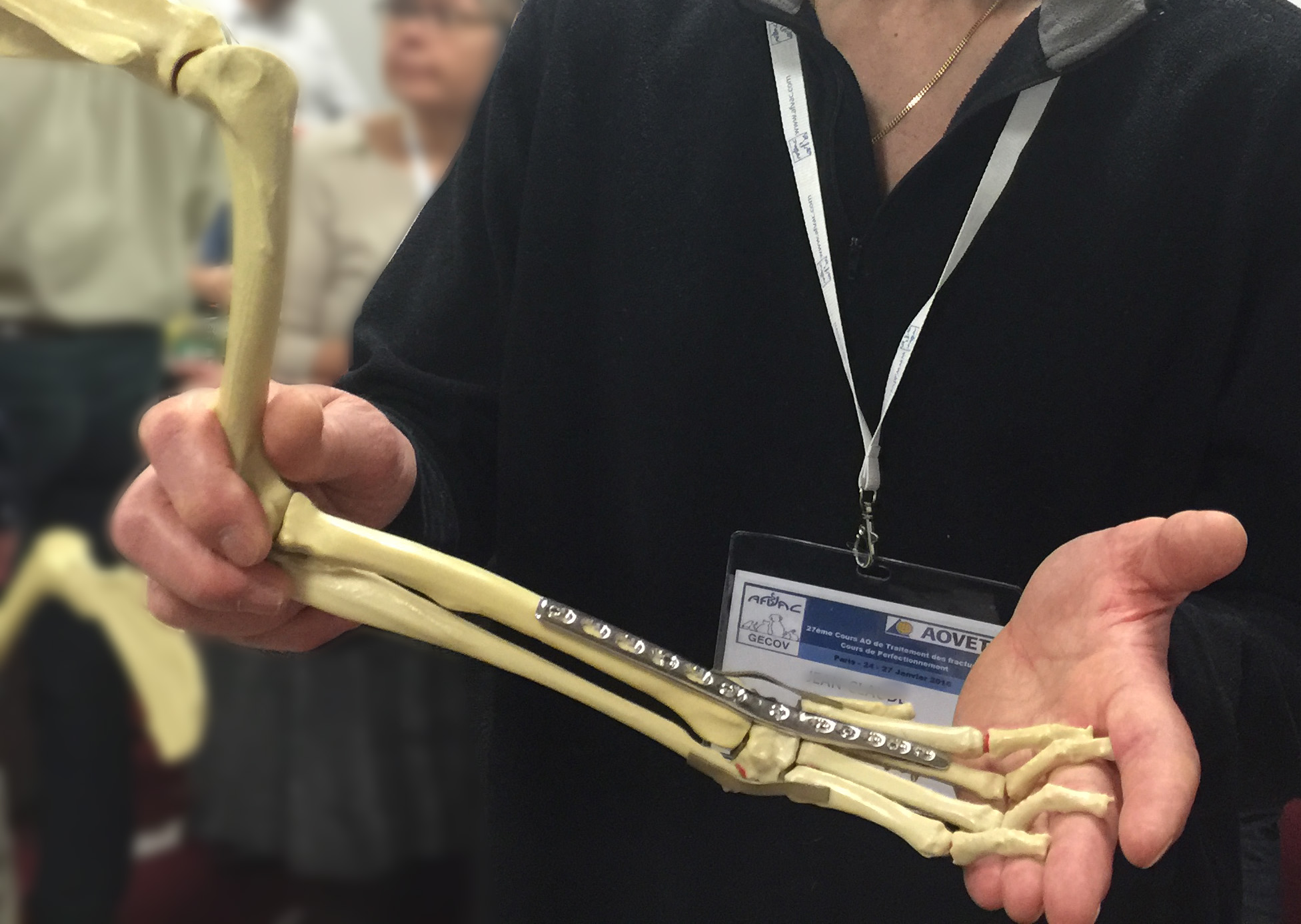
3. Help for better planning, time and cost effective surgery
In some instances, 3D printed objects are not aimed at being used on the patient; but rather at helping health technicians to better evaluate the injury or malformation. Coupled with CT scans, the patient’s anatomy is closely mapped through CAD software and reproduced by a 3D printer. This allows surgeons to appropriately plan the intervention, thereby greatly lowering the risk of complications. This use of 3DP is expected to make reconstruction easier, quicker, and cheaper. [Bardet et al., 2015]
|
Figure 6: metal plate placed and adjusted on the |
3.1. Bone Fracture repair or congenital bone deformation
Using 3D views of the computed MRI scan, an acrylic model of the injured area is reproduced by a 3D printer. The reproduced bones allow for a more exact diagnosis of a possible fracture or inherited malformation and allow the surgeon to choose the right equipment prior to surgery. Metal plates, for instance, are adapted (bent) to the 3D model so it fits perfectly with the patient’s bone shape and size, as well as being catered to their specific needs (for example, bone fracture). (Figure 6) Screw zones can also be carefully picked from viewing the 3D model without regular visibility restrictions of the surgical area. With careful planning, using the precise 3D-printed bone model, the surgical approach is made easier and the intervention is quicker and more precise. These factors contribute to a successful bone repair. In some malformations, such as radius curvus, the combined use of angled rotation centers, MRI, and acrylic 3D models gives an accurate assessment of bone deformities which otherwise could not have been obtained. With these new, innovative methods a precise pre-surgical strategy can be created for large bone defects, allowing them to be fixed in a single intervention. [Bardet et al., 2015]
3.2. Cartilage/ bone replacement
In these kinds of interventions, the injured or missing organs need to be replaced by similar tissue taken from another body part. Needless to say that the material supply is limited and precious. In the example of ear replacement surgery, cartilage is harvested from the rib cage, from which the new ear is immediately carved. The time and error allowance is therefore very low. Before the appearance of 3DP, surgeons have been practicing carving of the needed shape on materials such as soap, fruits, pig cartilage, etc. Training material rarely had the size consistency or characteristics for a true preparation. A better solutiom came with a low cost 3D print cartilage model close to the look and feel of human cartilage, which enables surgeons to practice on the procedure with a superior training efficiency.
4. Organ implants
Tissue or organ failure, diseases, accidents, and birth defects are critical medical problems. Current treatments rely mostly on organ transplants from living or deceased organ donors, who need to be a “match”. [Cui et al., 2012] While the global population is aging and unseen diseases appear, 3DP brings an alternative to (the lack of) organ donations or appropriate medication. It is a revolutionary step in the world of medicine. 3DP now allows the use of biocompatible materials, cells, and other biological components to print complex structures such as tissues and organs, destined for organ transplantation. Scientists have so far been able to create several kinds of tissues including multi-layered skin, bone, vascular tissue, tracheal splints, heart tissue, and cartilaginous structures. [Murphy and Atala, 2014] An innovative solution involves using a cell sample from the patient, to grow a replacement organ which can minimise risks of tissue rejection, and lifelong need of immunosuppressants. [Schubert et al., 2014] 3DP is already hard at work in the implant industry, taking over the business with custom-made and unique 3D printed implants. However, there are no magic solutions: though they provide a much better fit, 3DP implants are still followed by months or even years of painful hobbling around and rehabilitation.
4.1. Soft tissue implants
In the first stages of soft tissue 3DP trials, the tissue was collapsing on itself while being printed. This has eventually been solved by using a slurry of gelatin to support the tissue or organ as it is being printed. Once the printing is complete the gelatin is melted away in room-temperature water, and the finished tissue is able to support itself.
4.1.1. New material
A vastly used 3DP technique is the "Two-photon polymerization". It creates small detailed objects from several types of photoreactive liquid precursors, which contain light-reactive chemicals that turn the liquid into a solid polymer. Unfortunately, most of these chemicals are toxic, and might cause complications when used in a medical implant. An alternative has been however found in riboflavin (vitamin B2): both nontoxic and biocompatible, it is mixed with a precursor material to make it photoreactive, and create medical implants from non-toxic polymers. [Nguyen et al, 2013] This discovery brought up many more biocompatible implant materials, which can be used for 3D implants printing.
|
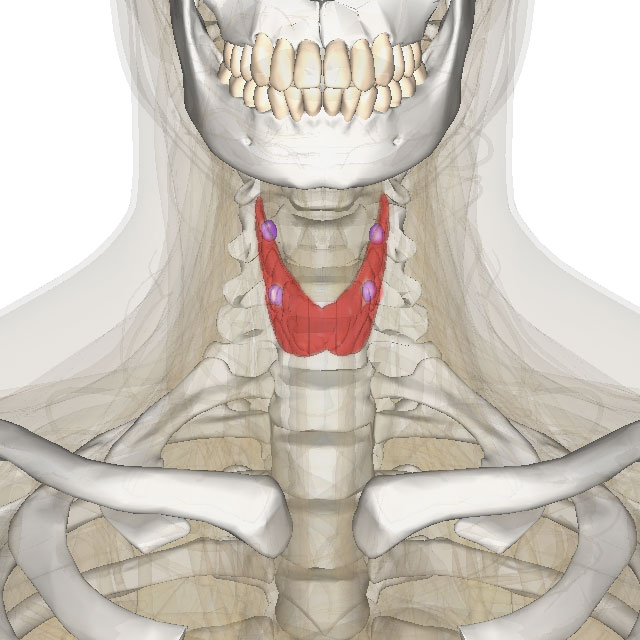
Figure 7: thyroid/parathyroid in color |
4.1.2. Printing Organs
In March 2011, Anthony Atala, M.D. (Director of the Wake Forest Institute for Regenerative Medicine) demonstrated the 3DP of a kidney from a solution of living cells, though it was lacking the necessary tubules and blood vessels to make it functional. Researchers had tried printing the kidney, leaving holes for the vessels and tubules, but this led to a lack in the structural stability needed to withstand blood pressure. This has been the main issue with creating functional organs: living cells need to be within 150-200 microns of a capillary to survive. Ongoing research is working on solving the problem, and create the incredibly small spaces needed for the blood supply within the 3D printed organ, along with the structural stability necessary to withstand normal blood pressure.
3D printing techniques has also been used to build a new external human ear. The auricle, printed from a collagen based material, was injected with gel made of living cells, which grew cartilage and replaced the collagen mold in 3 months. So far, replacement ears had been built from a more styrofoam-like material or as seen earlier, from harvested cartilage on the own's patient sternum. This bioengineering advancement pushes the field 3DP and tissue engineering towards entirely printed organs. [Reiffel et al., 2013]
In march 2015, a thyroid gland was successfully reproduced and transplanted on a mouse. This specific organ (Figure 7) was chosen due to its relative simplicity, with hope that later on, other organ transplants would be possible as technology allows it. The mouse’s own stem cells (from fat tissue) were used as primary material in order to prevent rejection, and the gland mature cells were grown thanks to a 3 directions robot, which dripped fabric layers of living cells through an automated syringe. Before printing, the cells were transformed into ‘spheroids’ (layered cells), then placed in hydrogel, to enable the printing process. After printing, the organ was placed in a bioreactor which dissolved the gel to leave the thyroid organ was left to mature on its own before the surgical implant.
|
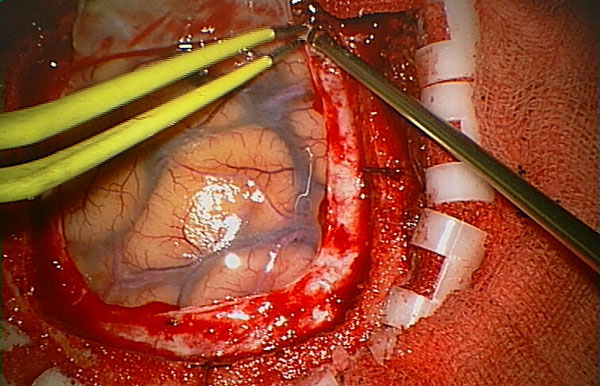
Figure 8: Surgery on the brain. |
4.1.3. Dura Mater
The brain is protected by dura mater. it is divided into a superficial and meningeal layer, which need to be cut open in case of brain surgery (Figure 8). Upon completion of the surgery, The Dura mater must be closed up by a suture and onlay procedure. “Maipu Regenerative Medical Technology” developed 3D printing of a substance they called “Redura”. Printed onto the surgical site “Redura” provides a suitable environment for the cells and tissues to regenerate. Within 2 months, the meningeal tissue grows back and the “Redura” begins to dissolve into 2 non-harmful natural components: water and carbon dioxide. The “Redura” is used in hospitals globally and has been successfully used in over 10 000 patients without any adverse effects.
4.2. Bones and cartilage implants
|
Figure 9: Porous bone. |
A broken bone can regenerate, but cannot regrow after being crushed or destroyed by cancer. It also cannot be easily replaced by another material, and its exact characteristics have been so far impossible to reproduce synthetically, because of several unique properties: It is highly porous from the inside (Figure 9), and firm on the outside, bones are strong, rigid, light and porous all at once. [Roohani-Esfahani et al., 2016] This is why they are the second most transplanted tissue in the world (after blood). So far, surgeons have been using segments of the patient’s own skeleton (autografts), but bones from cadavers can also be used (allograft), as well as various ceramics or metallic alloys. The use of autografts limits availability, while other options can result in rejection by the organism. 3DP technologies have become extremely useful in the constantly growing field of osteology and arthrology. They allow significant advances in synthetic bone implants. Many different materials have been developed to mimic bone characteristics, and use of patient-specific imaging data makes it possible to print 3D bone implants specific to each individual. Latest researches and discoveries already contribute to replacing the use of metal altogether. Implants will eventually be made entirely from biocompatible materials that can be broken down by the body.
4.2.1. Cartilage repair
Cartilage is a poorly irrigated tissue. once damaged, it never regenerates, and defects may lead to osteoarthritis (in adults). This repair incapacity could be solved by tissue Engineering. Among the challenges: the production of an optimum scaffold is able to: - Reproduce the natural extracellular matrix - Carry cartilage functions in the early stage of the implant process, while also inducing the regeneration of tissue.
Hydrogels are attractive 3DP biomaterials for the repair of articular cartilage. They can potentially help with regeneration, as they share several common features with the organism extracellular matrix, and allow cell encapsulation in a highly hydrated and mechanically supportive 3D environment. Hydrogels also allow efficient and homogeneous cell seeding, pipetted directly onto the scaffold structure. Hydrogels can provide chemical and physical biologically-relevant signals while being printed in various shapes and biomechanical characteristics. They still need to be optimized to ensure proper cell survival conditions, while respecting physico-chemical requirements for the biofabrication process. A challenge well on its way thanks to the development of novel hydrogel-based bioinks, in parallel with multi-material biofabrication approaches, in order to construct intricate stable 3D structures which provide the cells with a biologically suitable environment, matching the harsh in-vivo mechanical conditions. [Malda, 2015]
|
Figure 10: 3D reconstruction of the CT scan |
4.2.2. Bone implants
High-precision 3D printers can steadily manufactures solid bone, one layer at a time. Artificial bones were initially developed to replicate complex bones such as the pelvis or spine. They were printed from titanium, and used on patients with bone tumor or after surgical resection. The main advantage being that 3DP recreates the exact skeletal structure of any patient, which enables to develop a 3D scaffold with the correct shape and size needed for implant. The skeleton area in need of reconstruction is CT scanned '(Figure 10)' in order to create a 3D image, which is used to calculate the shape of the personalised bone piece needed. It is then precisely printed out using one of several developed techniques and accompanying material. The race for discoveries has been pushing numerous universities, researchers and manufacturers to concentrate their efforts on the development of the yet latest breakthrough which make bone implants, safer, quicker and cheaper. It has become a very competitive market and grows at a very fast pace for veterinary and human use alike.
4.2.2.1. Allograft material
Bones have been successfully printed from a material composed of very fine bone powder and biological glue. The allograft bone powder is made from other animals of the same species, theoretically increasing the chances of biological compatibility (in comparison to metal implants). The 3DP process consist of minuscule layers of bone powder followed by bio-glue (around 0.1 mm of bone-glue-bone-glue layers). this process requires thousands of layers to form a very detailed structure, and this method is limited as to print sizes. Bones cannot exceed 15 cm because this form of printing is not as strong as original bones causing long bones to lose sturdiness. Moreover, biocompatibility problem still remains and rejections still exist.
4.2.2.2. Synthetic material
It has been a challenge to make a synthetic material that is very porous (allowing blood and cells to go through it), but also mechanically strong, to match the real bony structure. Nevertheless, a few processes have been developed to create synthetic bones that are even stronger than the real thing. Synthetic bone is printed using a 3D printer capable of using two synthetic polymers in an optimized geometric pattern. The hierarchical structures giving strength to the natural composite are self-assembled through electrochemical reactions. The Geometric pattern used for 3D print are based on those seen in natural material such as bone or nacre, but also include new designs non-existing in nature, which make the material much more resistant: the composite fracture behavior is similar to bone, though 22 times more fracture-resistant than its strongest constituent material. [Dimas et al., 2013]
Another printable material has been developed to be hundred times stronger than current synthetic materials. By studying properties of the skeleton, such as collagen and calcium, a new ceramic material has been made to copy all the structural and functional aspects of bones. Its strength and porosity are very similar to natural bone: strong enough to withstand the pressure of use, but porous enough to allow blood and cells to pass through it. In addition, it is capable of encouraging the regeneration of new bone cells in the correct position. The ceramic is bioactive and contains seed cells resembling natural bone which can eventually be replaced by natural bone in the body. It is also well accepted by the body (no rejection), Which makes it a particularly interesting material which is far superior to other synthetic materials. [Roohani-Esfahani et al., 2016]
4.2.2.3. Autograft made differently
After the treated area has been scanned and calculated, a 3D scaffold is printed using only the mineral part of animal bones: the bones are stripped from all their cellular material. Then, stem cells are extracted from a fat sample taken from the patient. They are injected into the printed shape and placed under human body conditions using bioreactor (temperature, pH, etc.), which by that, they grow bones. In 3 weeks time, the new bone is completed, the animal bone scaffolding is removed, which means the implant is completely made of the patient’s own cells, to avoid risks of ejection. So far, (2016) this procedure has only been applied on animals, and will soon be used on humans. The procedure could be used on patients with congenital facial defects, bone trauma and other complications, with surgical complications greatly reduced.
4.2.2.4. Anti-rejection material: the 3D printing revolution
When an implant needs replacement, or needs removal several years after its implantation due to rejection, it is another trauma caused to the patient. Fortunately, a developed material made from a calcium polyphosphate powder similar to bone, is bio-absorbable and ultimately replaces fresh tissue. The new bones and custom joints are printed using a powder-deposition printing technique, then heated to become completely solid and implantable. Though more and more biocompatible 3D materials are developed, calcium polyphosphate is actually so compatible, that new bone will grow directly into the implant. Over time, the implant is completely replaced with new bone, not only diminishing the need for additional surgery, but optimizing recovery as well. The project has been in development since 2008, and animal testing is starting in 2016. Several challenges still need to be overcome, then, the principle can be applied to just about every necessary implant -from knees, hips, shoulders and ankles. [An et al., 2016]
4.2.2.5. Stronger implant
Improving the strength of 3D printed bone implants, could help patients who have suffered significant bone loss, to recover much faster. A novel 3D printing process involves manipulating and freezing the growth crystals within a 3D printed material. crystals grown in sub-zero temperatures might provide a viable solution to improve the strength of 3D printed bones while retaining the structures’ porosity. A micro-computed tomography image of the sample bone scaffold 3D printing combined with freezing can reduce significantly the fabrication time and cost of such medical devices. The secret behind the toughness of many biological materials is the way their components are arranged from the molecular level , all the way up to the macro level. Using this design strategy could help engineer bone scaffolds, whose porosity does not compromise their strength.
5. References
- Bardet J. F., Bordelo J. P. A. (2015): Passavin P. Radius Curvus. Synthese Vétérinaire. 359: 22-24.
- Bartlett S. (2013): Printing organs on demand. Lancet Respir Med 1(9): 684.
Cui X.; Boland T.; D’Lima D. D.; Lotz M. K. (2012): Thermal inkjet printing in tissue engineering and regenerative medicine. Recent Pat Drug Deliv Formul 6(2): 149–155.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3565591/- Klein G. T.; Lu Y.; Wang M. Y. (2013): 3D printing and neurosurgery—ready for prime time? World Neurosurg 80(3-4): 233–235.
- Dimas L. S.; Bratzel G. H.; Eylon I.; Buehler M. J. (2013): Tough Composites Inspired by Mineralized Natural Materials: Computation, 3D printing, and Testing. Advanced functioning material. 23(36):4629-4638
An L.; Guang-huai X.; Miao S.; Hui-feng S.; Chi-yuan M.; Qing G.; Zhong-ru G.; Shi-gui Y.; Yan-ming L.; & Yong H. (2016): 3D Printing Surgical Implants at the clinic: An Experimental Study on Anterior Cruciate Ligament Reconstruction. Sci. Rep. 6, 21704.
http://www.nature.com/articles/srep21704- Malda J. (2015): The application of 3D hydrogel printing technology for cartilage regeneration. European Cells and Materials. 30(1): 3.
Murphy S. V.; Atala A. (2014): 3D bioprinting of tissues and organs. Nature Biotechnology. 32: 773–785
http://www.nature.com/nbt/journal/v32/n8/full/nbt.2958.htmlNguyen A. K.; Gittard S. D.; Koroleva A.; Schlie S.; Gaidukeviciute A.; Chichkov B. N.; Narayan R. J. (2013): Two-photon polymerization of polyethylene glycol diacrylate scaffolds with riboflavin and triethanolamine used as a water-soluble photoinitiator. Future medicine. 8(6): 725-738.
http://www.futuremedicine.com/doi/abs/10.2217/rme.13.60?journalCode=rme&Schubert C.; Van Langeveld M. C.; Donoso L. A. (2014): Innovations in 3D printing: a 3D overview from optics to organs. Br J Ophthalmol 98(2): 159–161.
http://bjo.bmj.com/content/98/2/159.full.pdf- Reiffel A. J.; Kafka C.; Hernandez K. A.; Popa S.; Perez J. L.; Zhou S., Pramanik S.; Brown B. N.; Ryu W. S.; Bonassar L. J.; Spector J. A. (2013): High-Fidelity Tissue Engineering of Patient-Specific Auricles for Reconstruction of Pediatric Microtia and Other Auricular Deformities. PLoS ONE 8(2): e56506. doi:10.1371/journal.pone.0056506
Roohani-Esfahani S. I.; Newman P.; Zreiqat H. (2016): Design and fabrication of 3D printed scaffolds with a mechanical strength comparable to Cortical bone to repair large bone defects. Sci. Rep. 6, 19468. DOI: 10.1038/srep19468
https://www.researchgate.net/publication/291387600Yue J.; Zhao P.; Gerasimov J. Y; Van De Lagemaat M.; Grotenhuis A.; Rustema-Abbing M.; Van Der Mei, H. C.; Busscher H. J.; Herrmann A.; Ren Y. (2015): 3D-Printable Antimicrobial Composite Resins. Advanced Functional Materials. 25(43): 6756–6767.
http://onlinelibrary.wiley.com/doi/10.1002/adfm.201502384/abstract;jsessionid=5FFB7E24256829D25461181357006B9E.f04t04
6. Websites
3D printing makes digital dentistry happen
http://www.stratasys.com/industries/dentalCore77. (2010): interview with Scott Summit, Co-Founder of Bespoke Innovations.
https://www.youtube.com/watch?v=uh6fzLOYp1MLatest News. (2015): 'Terminator' turtle gets a 3D printed titanium jaw.
https://www.youtube.com/watch?v=5HtnDLRQCc4ABC News Australia. (2016): 3D-printed titanium beak gives Brazilian macaw Gigi chance to crunch food for first time
http://www.abc.net.au/news/2016-02-25/titanium-beak-gives-macaw-chance-to-crunch-food/7198934Langston J. (2015): 3-D printing techniques help surgeons carve new ears.
http://www.washington.edu/news/2015/09/30/3-d-printing-techniques-help-surgeons-carve-new-ears/3D systems. "Derby the Dog, running on 3D prosthetics" (2015)
https://youtu.be/uRmoowIN8aYCNN. (2015): Grow human bone from fat.
http://edition.cnn.com/videos/tech/2015/10/30/orig-pioneers-epibone-human-bones-from-fat.cnn/video/playlists/pioneers-orig/3D bone printing project in China to enter animal testing stage (2015)
http://www.3ders.org/articles/20150715-3d-bone-printing-project-in-china-to-enter-animal-testing-stage.htmlGrunewald S. J. (2016): New Research into 3D Printed Bone Implants Could Change the Way We Heal Broken Bones.
https://3dprint.com/118059/3d-printed-bone-implants/Zavyalova V. (2015): Honey, I printed a thyroid gland
http://rbth.com/longreads/bioprint/index.htmlStephen Feller (2016): Scientists 3D-print bone structure to help tissue regenerate
http://www.upi.com/Health_News/2016/02/08/Scientists-3D-print-bone-structure-to-help-tissue-regenerate/3221454937055/Biomimetic-Synthetic-absorbable dural substitute (2015)
http://web.ros-medical.com/public/uploads/files/biologicos/Folleto_ReDura.pdfAtala A. Printing a human kidney (2011)
https://www.ted.com/talks/anthony_atala_printing_a_human_kidney
7. Figures
- Андрей Ильин [CC0 or CC0]. Wikimedia Commons
- Jestin, C. "3D printed Dental brace". 2016. Own work.
Coronation Dental Specialty Group. [CC BY-SA 3.0]. Wikimedia Commons.
3D systems. "Derby the Dog, running on 3D prosthetics". 2015. YouTube Video.
Latest News. "'Terminator' turtle gets a 3D printed titanium jaw". 2015. YouTuve Video.
- Jestin, J.C. "Aovet congress". 2016. Own work.
BodyParts3D is made by DBCLS (Polygondata is from BodyParts3D). "thyroid/parathyroid in color against skeleton and various organs". [CC BY-SA 2.1]. Wikimedia Commons.
- Anonymous. "Craniotomy_Arachnoid". 2006. Wikimedia commons.
patrick siemer from san francisco, usa. "bone" [CC BY 2.0]. Wikimedia Commons.
Desherinka. Personnal work. [CC BY-SA 3.0]. Wikimedia Commons.
8. Further reading (and Watching)
Duhaime-Ross A. (2016): This 3D bioprinter can make human-sized ear, muscle, and bone tissues
http://www.theverge.com/2016/2/15/10995730/3d-print-human-tissue-ear-muscles-boneCronin L. (2012): Print your own medicine.
https://www.ted.com/talks/lee_cronin_print_your_own_medicineSummit S. (2011): Beautiful artificial limbs.
https://www.ted.com/talks/scott_summit_beautiful_artificial_limbs