Pathogenesis of the Main Neurodegenerative Diseases: Alzheimer’s and Parkinson’s Diseases
Project by:
Pirounaki, Styliani
Vadamootoo, Shanya
Aoun, Lea
Supervisor:
Dr. Bárány Zoltán
Physiology Department,
University of Veterinary Medicine, Budapest
Spring Term, 2017
Contents
-
Pathogenesis of the Main Neurodegenerative Diseases: Alzheimer’s and Parkinson’s Diseases
- Introduction to Alzheimer’s disease
- Types and stages of Alzheimer’s disease
- Causes of Alzheimer’s disease
- Diagnosis and treatment
- Correlation to Animals
- Introduction to Parkinson’s disease
- Stages of Parkinson’s disease:
- Causes of Parkinson’s disease
- Diagnosis and treatment
- Correlation to Animals
- Recent discovery
- References
Introduction to Alzheimer’s disease
Alzheimer's disease (AD) is the most common type of dementia, it is caused by parts of the brain shrinking (atrophy), which affects the structure and function of particular brain areas. AD and dementia are often used interchangeably as many people believe that one means the other. According to the national institute on aging (NIA), Dementia is a brain disorder that affects communication and performance of daily activities(impaired thinking and memory) and AD is a form of dementia that specifically affects parts of the brain that control thought, memory and language. AD is not a reversible disease. It is degenerative and incurable at this time. Some forms of dementia, such as a drug interaction or a vitamin deficiency, are actually reversible or temporary.
Atypical AD: Atypical AD is the type of AD where a different area in the brain is affected. Although this type of AD results because of the same underlying cause (plaques and tangles), its first symptom is not memory loss. The atypical forms of AD are as follows:
Posterior cortical atrophy (PCA) occurs when there is damage to the parietal lobes (Ross S, 1996).These are areas that process visual information and deal with spatial awareness. This means the early symptoms of PCA are often problems identifying objects or reading, even if the eyes are healthy.
Logogenic aphasia involves damage to the areas in the left side of the brain(frontal lobes) that is responsible for speech. The person’s conversation becomes labored with long pauses.
- Frontal variant AD involves damage to the Frontal lobes. The symptoms are problems with planning and decision-making. The person may also behave in socially inappropriate ways or seem not to care about the feelings of others (Krishnan, 2014).
Types and stages of Alzheimer’s disease
Types:
- Early onset AD:
- Early-onset AD occurs in people age 30 to 60 and represents less than 5 percent of all people with Alzheimer's. Most cases are caused by an inherited mutation in one of three genes. For others, the disease develops without any genetic or other known cause.
- Early-onset AD is caused by a single-gene mutation on chromosomes 21, 14, or 1. Due to these mutations, abnormal proteins are formed. Mutations on chromosome 21 cause the formation of abnormal amyloid precursor protein (APP). A mutation on chromosome 14 leads to the production of abnormal presenilin 1(PS1) (a core protein that forms amyloid beta from APP), and a mutation on chromosome 1 leads to abnormal presenilin 2(PS2); which processes proteins that transmit chemical signals from the cell membrane to the nucleus.
Mutations in the genes for APP, PS1 and PS2 were observed in AD families and all these mutations induced an increase of Ab production (Puzzo & al, 2015); on the other hand, a mutation in the APP gene that results in a reduction in the formation of amyloidogenic peptides was found to protect against cognitive decline in the elderly (Jonsson et al., 2012)
- Early-onset AD occurs in people age 30 to 60 and represents less than 5 percent of all people with Alzheimer's. Most cases are caused by an inherited mutation in one of three genes. For others, the disease develops without any genetic or other known cause.
- Late-onset AD:
- Most people with AD have this form of the disease, in which symptoms become apparent in the mid-60s and later. A specific gene has not yet been found to cause late-onset AD. However, one genetic risk factor—having one form of the apolipoprotein E (APOE) gene on chromosome 19—increases the risk of late on-set AD(Corder E. H. et al, 1993). APOE comes in several different forms, or alleles:
- APOE e2 — the least common — appears to reduce the risk of Alzheimer's.
- APOE e4 — a little more common — appears to increase the risk of Alzheimer's.
- Having at least one APOE e4 gene increases the risk of developing Alzheimer's disease. If you have two APOE e4 genes (one on each chromosome), the risk is even higher. But not everyone who has one or even two APOE e4 genes develops Alzheimer's disease. The disease also occurs in many people who don't even have an APOE e4 gene, suggesting that the APOE e4 gene affects risk but is not a cause.
- Most people with AD have this form of the disease, in which symptoms become apparent in the mid-60s and later. A specific gene has not yet been found to cause late-onset AD. However, one genetic risk factor—having one form of the apolipoprotein E (APOE) gene on chromosome 19—increases the risk of late on-set AD(Corder E. H. et al, 1993). APOE comes in several different forms, or alleles:
Stages: The different stages of AD are summarized in table 1.
Stages |
Signs |
Stage 1 |
No impairment- the person does not experience memory problems. No evidence of disease. |
Stage 2 |
Very mild decline- Person feels as if he/she is having memory lapses-forgetting familiar words or location of everyday objects, but no symptoms of dementia can be detected. |
Stage 3 |
Mild decline- Difficulties may be noticed. Doctors may be able to detect problems in memory or concentration. Some difficulties: |
Stage 4 |
Moderate decline- Clear-cut symptom can be detected in several areas such as forgetfulness of a recent event or one’s own personal history |
Stage 5 |
Moderately severe decline- gaps in memory and thinking are noticeable and an individual begins to need help with day-to-day activities. Examples: Being unable to recall own address, where they are, what day it is, choosing proper clothing… |
Stage 6 |
Severe decline- Memory continues to worsen, personality changes may take place and extensive help is needed for day-to-day activities. Examples: |
Stage 7 |
Very severe decline- loss of ability to respond to the environment, to carry on a conversation and eventually to control movements (Reflexes become abnormal and muscles grow rigid). They lose ability to smile and cannot sit on their own. |
Table 1: Stages of AD (Table created by Lea Aoun, Shanya Vadamootoo and Styliani Pirounaki)
Causes of Alzheimer’s disease
Some factors are known to increase the risk of developing A.D. (Belluck P, 2016). These include:
- Age
- Age is the single most significant factor in the development of AD; the risk greatly increases after the age of 65. Early-onset AD can affect people much younger than that, but the percentage is very low (1 in 20 people affected)
- Family history of the condition
- Inherited genes can contribute to the risk of developing A.D, although the actual increase is small.
- Down’s Syndrome
- This is because the genetic fault that causes Down's syndrome (mutation in the chromosome 21) can also cause amyloid plaques to build up in the brain and that may lead to A.D.
- Gender
- Women are twice as likely to get A.D. The reasons are not clear but it may be linked to the lack of the hormone estrogen after menopause.
- Lifestyle factors. These include:
- Smoking
- Obesity
- Diabetes
- High blood pressure
- High cholesterol
- Previous severe head injuries
- Conditions associated with cardiovascular disease
The risk can be reduced by:
- Stopping smoking
- Eating a healthy, balanced diet
- Leading an active life, both physically and mentally
- Regular health checks
Although the causes of AD aren't yet fully understood, its effect on the brain is clear. AD damages and kills brain cells such as neurons(mostly in the hippocampus), which are the main target cell, astrocytes, which are important support cells that become overactive in the affected brain, and the microglial cells, which are neuroglial cells that function as the main form of active immune response in the CNS. In the Alzheimer's brain: (as seen in figure 1)
- The cortex shrivels up, damaging areas involved in thinking, planning and remembering.
- Shrinkage is especially severe in the hippocampus, an area of the cortex that plays a key role in formation of new memories.
- Ventricles (fluid-filled spaces within the brain) grow larger.
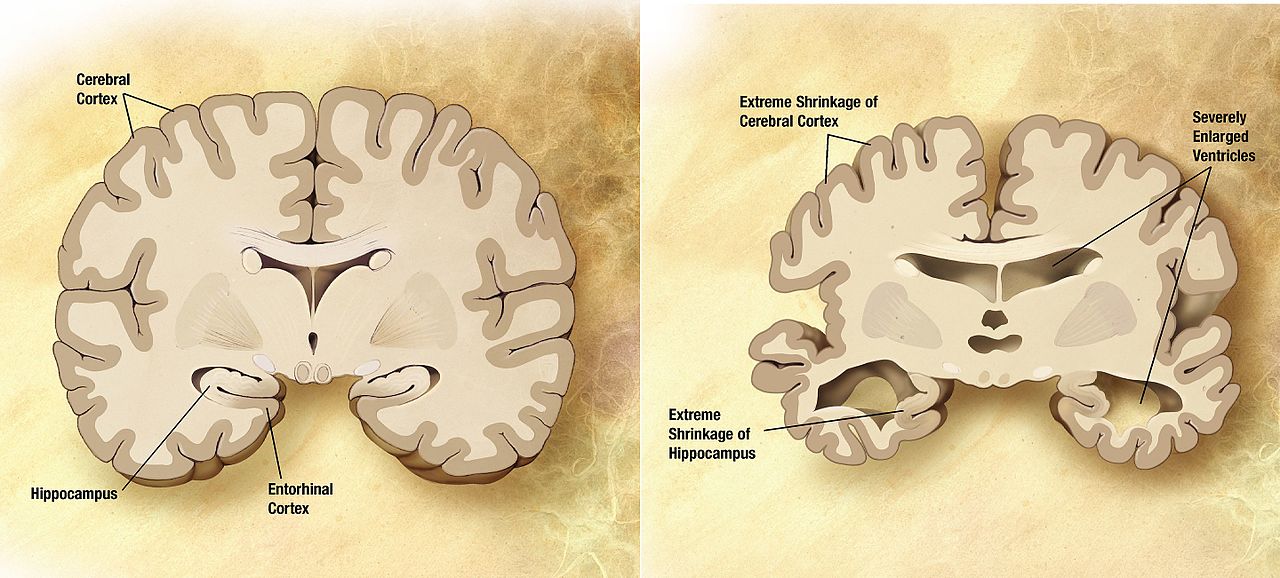 Figure 1: Shrinkage of the brain due to Alzheimer's Disease. Permission to use the image was granted. https://commons.wikimedia.org/w/index.php?curid=4471173%22%3ELink%3C/a (20/04/2017)
Figure 1: Shrinkage of the brain due to Alzheimer's Disease. Permission to use the image was granted. https://commons.wikimedia.org/w/index.php?curid=4471173%22%3ELink%3C/a (20/04/2017)
Plaques form when protein pieces called beta-amyloid clump together. Beta-amyloid is chemically "sticky" and gradually builds up into plaques. The small clumps may block cell-to-cell signaling at synapses. They may also activate immune system cells that trigger inflammation and devour disabled cells. Recent research has found that amyloid begins accumulating 20 years or more before symptoms of dementia occur, and advancements in scans that can detect amyloid are making it possible to identify people in earlier stages, including some who have no symptoms of dementia yet.
Newly found evidence suggests that AD pathogenesis is not restricted to the neuronal compartment but also interacts with immunological mechanisms in the brain. Pattern recognition receptors on microglial cells and astrocytes are bound by aggregated proteins. This binding triggers an innate immune response that causes the release of inflammatory mediators, which contribute to AD pathogenesis and can affect its severity (Heneka M.T. et al, 2015). Clinically, AD patients do not show the cardinal signs: dolor, tumor, calor, and rubor (i.e., pain, swelling, heat, redness). Even though neutrophils, which play a role in the classical acute inflammatory response, are absent, AD brains show active microglia (brain macrophages) which indicates the activation of mononuclear phagocytes. At the molecular level, amyloid plagues in the brain contain various proteins associated with an inflammatory response. However most of these proteins, in different concentrations, play different roles, thus, their precise role in the amyloid formation is still unknown (Eikelenboom P. et al, 2002).
There are several histopathological alterations that could be detected during A.D:
- Alzheimer's tissue has many fewer nerve cells and synapses than a healthy brain.
- Plaques, abnormal clusters of protein fragments, build up between nerve cells.
- Dead and dying nerve cells contain “tangles”, which are made up of abnormally twisted strands of another protein called tau.
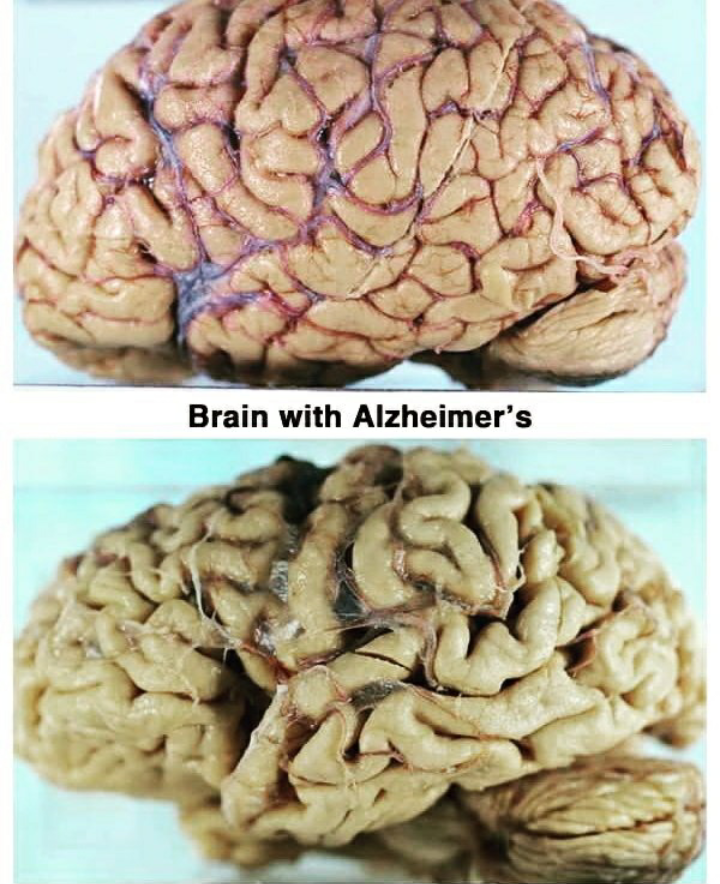
Figure 2: Healthy brain vs. Alzheimer's brain Permission to use this image was granted https://www.instagram.com/p/BSrimHSjTO5/?taken-by=wannastudy_medicine&hl=en (14/04/2017)
Diagnosis and treatment
There is no reliable diagnostic tool for AD. While physicians can almost always determine if a person has dementia, it may be difficult to determine the exact cause. Diagnosing Alzheimer's requires careful medical evaluation, including:
- A thorough medical history
- Mental status and mood testing
- A physical and neurological exam
- Tests (such as blood tests and brain imaging) to rule out other causes of dementia-like symptoms
Treatments: Several treatments of AD are compiled in table 2.
Types of Treatment |
|
Antipsychotic drugs |
Originally developed to treat schizophrenia, antipsychotic drugs are being tested in treating psychosis, agitation and aggression in AD Studies have established that, as in schizophrenia, there is a therapeutic window of D2/3 receptor occupancy for optimal treatment of psychosis in AD (Reeves et al., 2017). |
Anti-amyloid treatment |
In asymptomatic Alzheimer disease- to test whether an anti-amyloid investigational drug, “Solanezumab” can slow memory and cognitive decline |
Exercise |
In adults with mild memory problems(EXERT)- to evaluate the effect of physical exercise on cognition, functional status, brain atrophy, blood flow in adult with mild memory impairment |
Aricept, Exelon, Namzaric, Namenda, Razadyne |
These drugs either slow the breakdown of the neurotransmitter acetylcholine or block the overproduction of glutamate in the brain, but none have been shown to work very well for very long |
SNIFF |
Study of nasal insulin to fight forgetfulness (SNIFF) - to find out whether a type of insulin when administered as a nasal spray improves memory in adults with mild memory impairment. |
Table 2:Various treatments for AD (Table created by Lea Aoun, Shanya Vadamootoo and Styliani Pirounaki)
Correlation to Animals
According to Dr. Lorie Huston, animals suffer from a similar disease known as cognitive dysfunction. There is no known breed disposition but it is found mainly in older pets, it is characterized by disorientation of the animal (walk in circle, stare into corners) as well as changes in sleeping cycle, loss of previous training and control of bladder. Affected animals may also lose interest in interacting with people. The disease can be due to damage of brain cells, mainly neurons in the substantia nigra, or formation of a plague due to B-amyloid protein. The plague plays a role in the destruction of the cells and shrinkage of the brain. “In addition, many of the substances that transmit messages within the brain appear to be altered, which could also lead to abnormal behavior.” Alzheimer’s disease and cognitive dysfunction are quite similar. They cause similar behavioral changes and physical changes in the brain. There is no cure for this Cognitive dysfunction but there are ways to control it. For example, to stimulate their brain activity (teaching them new tricks) to slow down the spread of the disease. Other techniques to keep the brain healthy are the supplementation of the antioxidants, fatty acids and L-carnitine in their diet. Selegiline can also be prescribed in dogs, cats and horses.
Introduction to Parkinson’s disease
Parkinson's disease (PD) is the second most common neurodegenerative disorder after AD. It a chronic and progressive movement disorder, meaning that symptoms continue and worsen over time. The main motor symptoms are collectively called “Parkinsonism” or “Parkinsonian Syndrome”. It is expected to impose an increasing social and economic burden on societies as populations age. Its prevalence is generally estimated at 0.3% of the entire population and about 1% in people over 60 years of age. PD is clearly an age related disease; it is rare before the age of 50 years and the prevalence increases with age (up to 4% in the highest age groups) (Lonneke, 2006).Neuroprotective effects of estrogen have been suggested as a possible explanation for a higher risk of PD in men than in women but their role is still controversial.
Stages of Parkinson’s disease:
Parkinson's is not considered a fatal disease. The disease progresses differently for each individual:
- Movement symptoms vary from person to person, and so does the rate at which they progress.
- Some people with PD live with mild symptoms for many years, whereas others develop movement difficulties more quickly.
- No motor symptoms also are very individualized, and they affect most people with PD at all stages of disease.
The stages of PD(shown in table 3) correspond both to the severity of movement symptoms and to how much the disease affects a person’s daily activities. The most commonly used rating scales are focused on the motor symptoms, but new scales include information on non-motor symptoms (such as problems with sense of smell).
The first, known as Hoehn and Yahr, will rate the symptoms on a scale of 1 to 5. On this scale, depending on a person’s difficulties, 1 and 2 represent early-stage, 2 and 3 mid-stage, and 4 and 5 advanced-stage PD.
- Another scale commonly used to assess the progression of PD is the United Parkinson’s Disease Rating Scale (UPDRS). It is more comprehensive than the Hoehn and Yahr scale, which focuses on movement symptoms. In addition to these, the UPDRS takes into account cognitive difficulties, ability to carry out daily activities, and treatment complications.
Stages |
Signs |
Mild Parkinson’s |
•Movement symptoms may be inconvenient, but do not affect daily activities |
Moderate Parkinson’s |
•Movement symptoms occur on both sides of the body |
Advanced Parkinson’s |
•Great difficulty walking |
Table 3:Stages of PD (Table created by Lea Aoun, Shanya Vadamootoo and Styliani Pirounaki
Primary Motor Symptoms: (seen in figure 3)
- Resting Tremor: In the early stages of the disease, about 70 percent of people experience a slight tremor in the hand or foot on one side of the body, or less commonly in the jaw or face.
- Bradykinesia: Bradykinesia means “slow movement.” It also describes a general reduction of spontaneous movement, which can give the appearance of abnormal stillness and a decrease in facial expressivity. Bradykinesia causes difficulty with repetitive movements, such as finger tapping.
- Rigidity: Rigidity causes stiffness and inflexibility of the limbs, neck and trunk. Muscles normally stretch when they move, and then relax when they are at rest. PD causes muscles to be in a constantly flexed position, sometimes contributing to a decreased range of motion.
- Postural Instability: It is one of the most important signs of PD. A person with postural instability loses balance and is unable to stand upright.
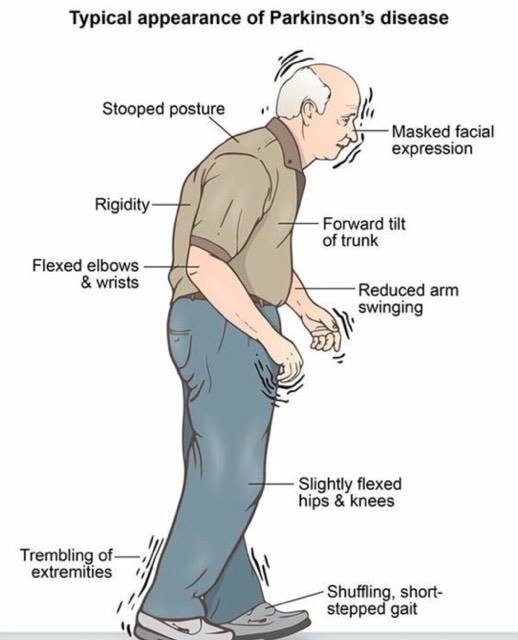
Figure 3: Signs of Parkinson's Permission to use this image was granted https://www.instagram.com/p/BSxDBIdgRpa/?taken-by=ma.ri.ze.te&hl=en (20/04/2017)
Secondary Motor Symptoms
- Freezing: Freezing of gait is an important sign of PD that is not explained by rigidity or bradykinesia.
- Micrographia: A person’s handwriting decreases in size. This occurs as a result of bradykinesia.
- Mask-like Expression: A person’s face appears less expressive than usual, occurs because of the decrease in facial movements.
- Unwanted Accelerations: Some people experience faster speech and movement instead of slower ones.
Non motor Symptoms: Most people with PD experience non-motor symptoms, those that do not involve movement, coordination, physical tasks or mobility. While a person’s family and friends may not be able to see them, these “invisible” symptoms can actually be more troublesome for some people than the motor impairments of PD.
Causes of Parkinson’s disease
PD involves the malfunction and death of vital nerve cells in the brain, called neurons. PD primarily affects neurons in an area of the brain called the substantia nigra. Some of these dying neurons produced dopamine, a chemical that sends messages to the part of the brain that controls movement and coordination. As PD progresses, the amount of dopamine produced in the brain decreases, leaving a person unable to control movement normally. This can be seen in figure 4. Scientists are also exploring the idea that loss of cells in other areas of the brain and body contribute to PD. For example, researchers have discovered that the hallmark sign of PD — clumps of a protein alpha-synuclein, (or Lewy Bodies) — are found not only in the mid-brain but also in the brain stem and the olfactory bulb which correlate to sense of smell and sleep regulation. This could explain the non-motor symptoms experienced by some people (Stecher, 2017)
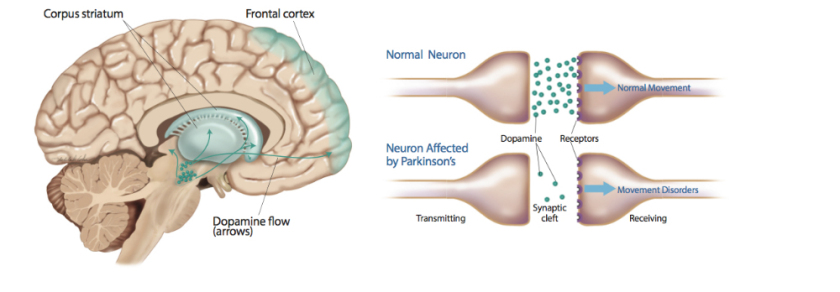
Figure 4: Effect of Parkinson's on the Dopamine release in the brain Permission to use this image was granted: https://futurism.com/were-about-to-enter-a-new-era-in-parkinsons-disease-treatments/ (27/03/2017)
To date, despite decades of intensive study, the causes of PD remain unknown. Many experts think that the disease is caused by a combination of genetic and environmental factors, which may vary from person to person. In some people, genetic factors may play a role; in others, illness, an environmental toxin or other event may contribute to PD. Scientists have identified aging as an important risk factor;
- Genetic Factors:
- The vast majority of PD cases are not directly inherited. About 15 to 25 percent of people with Parkinson’s report having a relative with the disease. Researchers have discovered several gene mutations that can cause the disease directly, but these affect only a small number of families. Some of these mutations involve genes that play a role in dopamine cell functions.
- Environmental Factors
- Some scientists have suggested that PD may result from exposure to an environmental toxin or injury. Epidemiological research has identified several factors that may be linked to Parkinson’s, including rural living, well water, manganese and pesticides.
It is noted that a simple exposure to an environmental toxin is never enough to cause PD, there is no conclusive evidence that any environmental factor, alone, can be considered a cause of the disease.
Diagnosis and treatment
The doctor asks questions about symptoms and health and performs a neurological exam that tests the nerves. The doctor will also ask questions about mood. In some cases, doctors prescribe medication. Lab and blood tests are performed to rule out other diseases.
At this time, there is no cure for PD. However, there are several types of medicines that can control the symptoms and make the disease easier to live with.
- Levodopa (also called L-dopa) is the best drug for controlling symptoms of PD. But it can cause problems if used for a long time or at high doses(Stecher, 2017).
- Another treatment is brain-stimulation in which wires are placed in specific parts of the brain that control motor functions. Electric impulses are used.
- New therapies:
- Neuromodulation techniques- The most prevalent is called transcranial magnetic stimulation in which magnets are attached to the outside of patient’s heads that send a focused electric current deep into the target areas of the brain. It is also used for depression(Stecher, 2017).
- Immunotherapies- The relatively recent identification of alpha-synuclein as playing a key role in disease formation has lead researchers to believe that we may be able to harness the body’s immune system to stop the protein from clumping while also mitigating the body’s natural inflammatory responses that damage neurons(Stecher, 2017).
- Stem Cell Therapies- This is due, in part, to the 2007 discovery of a new type of stem cell called IPS cells which allow researchers to grow fully functioning stem cells from patient’s own skin cells(Stecher, 2017).
- Gene Modification Therapies - The most popular one today is called CRISPR, a technique that allows researchers to cut and paste genetic code, changing the genome of living organisms(Stecher, 2017).
- Direct Programming – Direct programming is believed to be the ultimate solution to neurodegeneration. It results in changing cell types in the organism. For example, in people with PD, healthy cells such as glial cells or astrocytes, can be altered into dopamine-producing cells(Stecher, 2017).
Correlation to Animals
All mammals have to produce dopamine and so they are able to become dopamine-deficient and develop Parkinson’s disease. Cats can exhibit "parkinsonian" symptoms, including small-to-pronounced tremors, front or back leg weakness, an altered or sluggish gait, rhythmic tics or twitches of the extremities, ears, eyes, tongue or face, frequenting falling or a lack of coordination. Parkinsonian symptoms in cats can have many causes. Possible causes may include several types of degenerative neurological disorders, encephalitis (swelling of the brain), injury, a reaction to prescription drugs, food or vitamin toxicity or sensitivity, spinal, brain or nerve tumors. A series of tests could be a diagnostic tool for the cat's parkinsonian symptoms. These tests may include: a complete blood count (CBC), urinalysis, a myelogram (dye-study of the spinal column), a CT scan or MRI, a spinal tap or cerebrospinal fluid check (CSF), X-rays, or an electromyography (EMG) to check for muscular problems. Treatment may include drugs, palliative care at home, avoidance of toxins, or a change in diet.
Recent discovery
Deborah Brauser (2017) showed in a recent research that Metformin (a medicine used to treat type 2 Diabetes Mellitus) was found to increase the chance of getting Alzheimer’s dementia or Parkinson’s diseases by almost twice as much if used long-term. "We'd heard about a possible protective effect from metformin. However, we found the reverse", said Dr. Kuan.
References
Brauser, D. (2017). Metformin Use Linked to Increased Dementia, Parkinson's Risk in Patients With Diabetes. Medscape.
Corder, B.H.;Sanders, A. M.; Strittmatter, W.J; Schmekel, D.E.; Gaskell, P.C.; Small, G.W.; Roses, A.D.; Haines, J.L.;Pericak-Vance, M.A.(1993) Gene dose of Apolipoprotein E type 4 Allele and the Risk of Alzheimer's Disease in Late-onset Families. Science 261:921-923
Eikelenboom, P.; Bate, C.; Van Gool, W.A.; Hoozemans, J.J.M.; Rozemuller, J.M.; Veerhuis, R.; Williams, A. (2002): Neuroinflammation in Alzheimer’s Disease and Prion Disease. GLIA 40: 232–239
Heneka, M.T.; Carson, M.J.; Khoury, J.E.; Landreth, G.E.; Brosseron, F.; Feinstein, D.L.; Jacobs, A.H.; Wyss-Coray, T; Vitorica, J; Ransohoff, R.M.; Herrup, K; Frautschy, S.A.; Finsen, B; Brown, G.C.; Verkhratsky, A; Yamanaka, K; Koistinaho, J; Latz, E; Halle, A; Petzold, G.C.; Town, T; Morgan, D; Shinohara, M.L.; Perry, V.H.; Holmes, C; Bazan, N.G.; Brooks, D.J.; Hunot, S; Joseph, B; Deigendesch, N; Garaschuk, O; Boddeke, E; Dinarello, C.A.; Breitner, J.C.; Cole, G.M.; Golenbock, D.T.; Kummer, M.P. (2015): Neuroinflammation in Alzheimer's disease. The Lancet Neurology, 14(4): 388=405
Johnsson, T.; Atwal, J.K.; Steinberg, S.; Snaedal, J.; Jonsson, P.V.; Bjornsson, S.; Stefansson, H.; Sulem, P.; Gudbjartsson, D.; Maloney, J.; Hoyte, K.; Gustafson, A.; Liu, Y.; Lu, Y., Bhangale, T.; Graham, R.R.; Huttenlocher, J.; Bjornsdottir, G.; Andreassen, O.A.; Johnsson, E.G.; Palotie, A.; Behrens, T.W.; Magnusson, O.T.; Kong, A; Thorsteinsdottir, U.; Watts, R.J.; Stefansson, K. (2012) A mutation in APP protects against Alzheimer’s disease and age-related cognitive decline. Nature 488:96–99.
Lonneke, M.L.; De Lau, M. (2006). Epidemiology of Parkinson's Disease. The Lancet, 525-535.
Puzzo, D.; Gulisano, W.; Aranico, O.; Palmeri, A. (2015) The keystone of alzheimer pathogenesis might be sought in ab physiology. Neuroscience Forefront Review, 26-36.
Reeves, S.; McLachan, E.; Bertrand, J.; Antonio, F.D.; Brownings, S.; Nair, A.; Greaves, S.; Smith, A.; Taylor, D.; Dunn, J.; Marsden, P.; Kessler, R.; Howard, R.(2017) Therapeutic window of dopamine D2/3 receptor occupancy to treat psychosis in Alzheimer's disease. Brain, 1117-1127.
Ross, S.; G.N.G. (1996). Progressive biparietal atrophy: An atypical presentation of Alzheimer's disease. Journal of Neurology Neurosurgery & Psychiatry, 61(4):388-95.
Stecher, B. (2017). We're About to Enter a New Era in Parkinson's disease Treatment, Futurism. http://www.nhs.uk/Conditions/Alzheimersdisease/Pages/Diagnosis.aspx
https://www.alzheimers.org.uk/download/downloads/id/3379/what_is_alzheimers_disease.pdf
https://www.nytimes.com/2016/05/02/science/what-is-alzheimers-disease.html?_r=0 https://www.ncbi.nlm.nih.gov/pubmed/28334978
http://www.alz.org/alzheimers_disease_stages_of_alzheimers.asp
http://www.alzheimers.net/difference-between-alzheimers-and-dementia/
http://www.mayoclinic.org/diseases-conditions/alzheimers-disease/symptoms-causes/dxc-20167103
https://www.nia.nih.gov/alzheimers/publication/alzheimers-disease-genetics-fact-sheet
http://www.petmd.com/blogs/thedailyvet/lorieahuston/2014/september/do-dogs-and-cats-suffer-alzheimers-32003#
http://www.alzheimers.net/2014-08-14/can-animals-get-alzheimers/
http://www.webmd.com/parkinsons-disease/tc/parkinsons-disease-topic-overview
http://www.pdf.org/en/diagnosis
https://futurism.com/were-about-to-enter-a-new-era-in-parkinsons-disease-treatments/
http://pets.thenest.com/can-cats-parkinsons-disease-10589.html
Image references:
https://commons.wikimedia.org/w/index.php?curid=4471173%22%3ELink%3C/a
https://www.instagram.com/p/BSrimHSjTO5/?taken-by=wannastudy_medicine&hl=en
https://www.instagram.com/p/BSxDBIdgRpa/?taken-by=ma.ri.ze.te&hl=en
https://futurism.com/were-about-to-enter-a-new-era-in-parkinsons-disease-treatments/
