Estrogen may induce breast cancer
Student essay written by: Andrea Myklebust, Annika Gjessing and Mari Jahr
Contents
Preface
We chose this topic because for us it is very interesting and an up to date topic. In this essay we wanted to get a better knowledge about estrogen, what preparations that contain higher level and what risks it may have on a human body. We have used textbooks and mostly medical articles posted on pubmed.com to get more information.
Introduction
Breast cancer is the most common type of cancer among women in the Western world, and breast cancer incidences have increased by 2-3 % annually during the past 50 years, (Bigaard et al, 2012). Several factors are playing a role in how women around the world get breast cancer, both lifestyle and genetics inherited play a crucial role. Several studies have been done proving that prolonged intake of the hormone estrogen over several years may increase the possibility to develop breast cancer. Estrogen intake in form of birth control pills and HRT (hormone replacement therapy) linked to menopause is the most common used preparations.
Physiology background
Estrogens are hormones which occur naturally and synthetically and are principally associated with ovarian cycle, pregnancy and parturition together with progesterone and gonadotropins. The most important hormones are those belonging to the group of steroids and are produced by the granulosa cells of follicles in the ovary, placenta and adrenal cortex in women. Estrogens comprises of estradiol-17β (Figure 1), estrone and estriol where estradiol-17β is the most predominant in both pregnant and non-pregnant.
Fig. 1. 17-beta-estradiol
Estrogen regulates the proliferation of normal and neoplastic breast epithelium. It triggers its effect on women genital development and the organism as a whole and is also to be found in bone structure. Some of its tasks relevant to this topic are to stimulate follicular development, development of secondary sexual characteristics like breasts by stimulating duct growth, secretory activity of uterine ducts and more.
Progesterone works close with the estrogens and it is a part of estrogens synthesis. It is a steroid sex hormone produced by corpus luteum of the ovary, placenta and adrenal cortex. Main task is to ensure secretory changes in the uterus in the other half of the menstrual cycle. In this way the uterus is ready to receive a fertilized egg. Progesterone also acts relaxing on the musculature of the uterus that will prevent repelling of the fertilized egg. It also promotes endometrial gland growth.
Both progesterone and estrogens are steroid hormones which are synthesized from the cholesterol in the blood. The pathway starts with the: cholesterol → pregnenolone → progesterone → testosterone → estrogens. (Reece, 2009).
The estrous cycle starts after puberty and is the period between two subsequent ovulations. It consists of four phases: proestrus, estrus, metestrus and diestrus. The length of estrus cycle in humans is 28 days and in mammals usually 21 days, but it differs from species to species. The estrous cycle is interrupted by pregnancy. Estrogen level is highest near the end of the follicular phase right before ovulation (menstrual cycle).
Estrogens have two receptors named ERα and ERβ and they are very alike in the amino acid level in both the DNA binding domain and the ligand binding domain. They are represented in many tissues, in some organs they are equally and in others one of them predominates. At the same time they may be represented in the same tissue, but in different cell types. The ERα is mainly represented in the uterus, ovary (theca cells), bone, breast, liver, white adipose tissue and more. While the ERβ is mainly represented in colon, ovary (granulosa cells), bone marrow, salivary gland and vascular endothelium. (Dahlman-Wright et al, 2006).
General about breast cancer
Breast cancer is a cancer type that develops from breast cells. Majority of breast cancer occurs in females and it is the most common invasive cancer in females World Wide. The breast consists of billions of microscopic cells. Under developing of breast cancer these cells multiply uncontrollably. Cell proliferation through receptor-mediated processes was long thought to be the only mechanism, but it is now known that the intermediates produced after several metabolizing reactions may produce oxygen radicals. These radicals can damage the cells proteins, DNA, etc. and the damaged DNA can turn into mutation, and later lead to cancer. (Conova, 2003).
Again, you have two subtypes which are determined by their location. The most common type is the one that begins in the lactiferous duct, also known as the milk duct. The second type begins in the lobules and is much less common.
Invasive breast cancer type is when the cancer cells break out from duct or inside the lobules and act on nearby tissue. The cancer cells may reach the lymph node and finally spread to other organs like liver, bones, lungs, and to other parts of the body by the blood stream and lymphatic system.
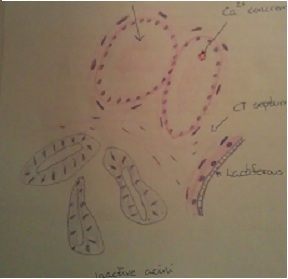
Fig. 2. Normal breast epithelium, mammary gland (Jahr, 2012)
The non-invasive breast cancer does not break out of their origin place, but are still inside the lobules/milk ducts. They may develop into invasive breast cancer.
Symptoms of breast cancer can be felt by the patient by having a lump in the breast, an area of thickened tissue, redness in skin around the breast, pain in armpits or beast that does not seem to be related to the woman’s menstrual cycle. (Nordqvist, 2012).
Why some develop breast cancer and others do not is not easy to say, but some risk factors can impact in a woman probability of developing breast cancer. The risk of developing breast cancer increases with age, most likely when the age 50 has past and after menopause. Genetics may also play an important role. Canadian National Breast screening study (2005) followed 27.318 women who had or have had a family member with breast cancer. They found 1.707 cases. Some genes can be inherited (like BRCA1 and BRCA2 genes). If a woman has had breast cancer, the risk of getting it again is higher compared to woman who has no history of the disease. Use of estrogen preparation also increase the risk of develop breast cancer. (Silvera et al, 2005).
Menopause, HRT and breast cancer
Menopause is the permanent end of menstruation and fertility and starts about 12 month after your last menstruation. It is a natural biological process, not a disease, and usually appears when women reach 45-55 years. Symptoms like hot-flash, urinary stress incontinence and vaginal dryness, suddenly changes in the everyday mood, osteoporosis etc. are common features. To diminish these symptoms many women use preparations like HRT (hormone replacement therapy). (Zieve, 2011).
HRT is the use of synthetic or natural female hormones to make up for the decline or lack of natural hormones produced in a woman’s body. Most of HRT contains both natural estrogen (estradiol, estron and estriol) and progestin. There are also pure estrogen HRT preparations (Progynova) which are without progestogen addition. Women who have had their uterus removed use these. Those who have intact uterus cannot use pure estrogen HRT because of the risk of cancer corporis uteri development. HRT can be taken as orals or transdermal (cream or patch).
Today, the most common argument to start HRT treatment is the menopausal symptoms. Hot-flash and the suddenly changes of everyday mood are symptoms which do not need long lasting treatments, while vaginal dryness and urinary stress incontinence are progressive and need several treatments. The natural estrogen in HRT has a protector effect on atherosclerosis. It lowers LDL and triglycerides. It raises HDL levels and has endothelial vasodilatation properties plus an anti-inflammatory component. The estrogen in HRT lowers vaginal pH, makes the epithelium thicker and increases the bloodstream. This rebuilding will improve dryness, bleeding, inflammation and tendency until increased vaginal discharge.
A main reason for why women avoid HRT is the increasing factor to develop breast cancer. Estrogens regulate the proliferation of normal and abnormal new growth of tissue in breast epithelium, but still some questions about how estrogens induce changes in the structure of the mammary epithelium are not yet known. A research done by the UCL School of Pharmacy, London, United Kingdom (2012), describes a connection between treatment with 17β-estradiol and induced breast cancer, and estrogen receptor with recovered normal breast epithelium. It is an investigation of mammary gland formation and disruption.
An in vitro 3D model of development of breast glandular structure was used to investigate the interaction. Together with the breast glandular structure, breast epithelial MCF-12A cells were used comprising estrogen receptor ERα, ERβ and G-protein coupled estrogen receptor 1 (GPER) component. The experiment showed normal development of breast epithelium with MCF-12A cells under normal conditions. The cells formed organized acini with deposition of basement membrane and hollow lumen. During treatment with 17β-estradiol, bisphenol A and propylparaben the epithelium showed obvious changes. The acini was deformed and got filling of the acinar lumen, a disruption of the breast epithelium. (Marchese and Silva, 2012). This discovery helps us understand how estrogens and their receptors act on development of epithelium, but still totally clearance of how they change the structure are not yet known.
A study done in Copenhagen, Denmark, by the Institute of Cancer Epidermiology, Danish Cancer Society (2004), investigated the relation between HRT and breast cancer. 29 875 women between year 1993-1997 were studied and 23 618 of them were assumed to be postmenopausal and use of HRT was available. Through 4-5 years of study 423 cases of breast cancer was identified. The study showed an increase of breast cancer incidence rate ratio (IRR) by 2,22 % for users of HRT compared to never users. It also showed that the IRR for estrogen receptor-positive tumors was greater than the IRR for estrogen receptor-negative tumors. Finally the likelihood to develop positive breast cancer tumors increased with the continuous use of hormone replacement therapy. (Tjønneland et al, 2004).
Birth control pills and breast cancer
Another way of taking in larger amount of estrogen is through use of birth control pills. There are several types. The most common type of the pill is the combination P-Pills containing small amounts of estrogen (estradiol) and progesterone (progestin). These hormones work to prevent pregnancy by inhibit the body’s natural cyclical hormones. Pregnancy is prevented by a combination of factors. Hormonal contraceptives normally stop the body from ovulating, changing the cervical mucous and by this makes it difficult for the sperm to fertilize the egg and also make the lining of the womb inhospitable for implantation. For those who have an increased risk of thrombosis the combination pill is not recommended, but they may use gestagen P-pills (minipills) instead. This is also birth control. The difference is that they only contain progresteron. Women who are sensitive to estrogen, special risk of heart disease and stroke are recommended to use this kind of contraceptive. (Hirsch, 2009).
Beside breast cancer there are other negative side effects of using birth control pills. Some of the effects can be venous thromboembolism, weight gain and depression, but there are also some positive effects. People that are troubled with acne can use the pills to reduce the skin problems, and if you have heavy menstrual bleedings and a lot of stomach pain this will also diminish with use of birth control pills.
Intrauterine device (IUD) is another form of contraception. It is a “T” shaped device inserted into the uterus to prevent pregnancy. It is inserted by a health care provider. There are different types. Hormonal contains progesterone and the non hormonal contains copper. Spiral is not recommended for younger people who have never been pregnant. This is because the uterus is not elevated and the IUD may slip out. Younger people who have several sexual partners over a shorter time may get sexual transferred diseases. When you use IUD it is a higher risk for getting infection. IUD works mainly by affecting the motion of sperm so that the sperm cannot fertilize an egg. The copper spiral works “sperm killing” and the internal environment changes in a way that make the spermcells move slower. The main effect of copper UID is to prevent that the fertilized attaches to the cervical cavity. The hormone spiral also leads to a thinner mucous membrane, and prevent some of the ovulations. This type of contraception is used for long term. It can be in the uterus for up to 5 years. For many older women who have already given birth this is a very comfortable contraception. IUDs can be use while breastfeeding. And if you decide to try to get pregnant once more it is only to take out the spiral and the chance for getting pregnant fast is very large compared to if you have prolonged use of birth control pills. Only the hormone IUD is deemed to be as safe as the P-Pill to prevent pregnancy, while copper IUD is less secure. (Marshall et al, 2011)
A meta-analysis done by Informa Health Care (2012) showed a combined relative risk of 1.08% (95% confidence interval [CI]: 0.99–1.17) of breast cancer in women who used oral contraceptives compared to never users of oral contraceptives. 13 prospective cohort studies were included in the research, by searching databases from the period 1960 to 2012. The study included 11,722 cases and 859,894 participants. Furthermore, a dose – response analysis including 5 studies showed that every 10-years increment of oral contraceptive use was associated with a significant of 14% (95% CI: 1.23) rise in breast cancer risk. However, it is important to take into consideration that the latter finding is based on only a limited number of studies as little evidence of publication evidence was found. (Hang et al, 2012).
Conclusion
In July 2002 Stanford Prevention Research Center, USA (2002), published some new results of harms associated with use of HRT, (Hersh et al, 2002). Since this publication many patients have ended their therapy or reduced to lower doses. Again in 2009 some new results concluded that use of HRT increases the risk of breast cancer, stroke and venous thromboembolism, (Banks and Canfell, 2009). Beside these negative effects, treatment with HRT has clear positive effects on hot-flashes, osteoporosis and urogenital problems. Though, it recommends for short term only and that it is important with consultation with the doctor. The study above changed the view of doctors/gynecologists. Before this, patients were directly recommended to use HRT, these were considered harmless, but after this study doctors were much more restrictive. HRT sales figures fell and the industry removed many products off the market.
Some research suggests that starting with HRT more than 10 years after menopause is unfavorable. Women who initially have a higher risk of heart disease and breast cancer should refrain from it.
About the use of birth control pills it was difficult to find any precise numbers about prolonged use risks. We did find out there is an increasing risk of developing breast cancer after long-term use and that the risk will decrease for every year you do not use any oral contraceptives. Risk of thrombosis is also very high. After some research about other alternatives we found different oral contraceptives and IUD with different levels of estrogens and hormone spiral without estrogens to match women with different needs and background.
References
- Stahlberg C., Kroman N., Jensen M. B., Ewertz M., Bigaard J. (2012): Breast cancer incidence by estrogen receptor status in Denmark from 1996 to 2007. Breast Cancer Research and Treatment, 136:559-564
- Reece W. O. (2009): Functional anatomy and physiology of domestic animals. 4th edition. Edition first published by Wiley-Blackwell, 2009, in Ames, Iowa 50014-8300, USA.
- Korach K. S., Katzenellenbogen J. A., Jordan V. C., Fuqua S. A., Dahlman-Wright K., Cavailles V. et al. (2006): International Union of pharmacology. LXIV. Estrogen receptors. Pharmacological Reviews 58: (4) 773-781
- Conova S., (2003): Estrogen` s Role in Cancer. In Vivo: Volume 2, No 10
- Nordqvist C. (2012): What is Breast Cancer? What Causes Breast Cancer? Medical News Today
- Silvera S. A., Rohan T. E., Miller A. B. (2005): Oral contraceptive use and risk of breast cancer among women with a family history of breast cancer: a prospective cohort study. Cancer Causes and Control, 16:1059-1063
- Zieve D. (2011): Menopause.
- Silva, Marchese S. (2012): Disruption of 3D MCF-12A Breast Cell Cultures by Estrogens - An In Vitro Model for ER-Mediated Changes Indicative of Hormonal Carcinogenesis.
- Tjønneland A., Thomsen B. L., Overkad K., Olsen A., Mellemkjaer L., Ewertz M., Christensen J. (2004): Hormone replacement therapy in relation to breast carcinoma incidence rate ratios: a prospective Danish cohort study. Cancer 100: (11) 2328-2337
- Hirsch L. (2009): Birth control: birth control pill. Page 1-3.
- O`Brien B., Marshall S., Jones K. (2011): Intrauterine Device (IUD) For Birth Control.
- Yang W., Xun L., Jing F., Hang Z. (2012): Oral contraceptive use and risk of brest cancer: A meta-analysis of prospective cohort studies. The European Journal of Contraception and Reproductive Health Care 17: (6) 402-414
- Stefanick M. L., Stafford R. S., Hersh A. L. (2004): National use of postmenopausal hormone therapy: annual trends and response to recent evidence. The Journal of the American Medical Association 291: (1) 47-53
- Canfell K., Banks E. (2009): Invited Commentary: Hormone therapy risks and benefits – The Women`s Health Initiatice findings and the postmenopausal estrogen timing hypothesis. American Journal of Epidemiology 170: (1) 24-28
Figures (All figures and pictures are prepared (redrawn) by students)
"17-beta-Estradiol":
"Normal breast epithelium, Mammary gland"
- Drawn by: Jahr M. (2012), Histology practical book 2
