The Inverse Relationship between the Incidence of Infectious diseases and the Immune diseases
By Maria Mulvihill, Serena Iceton, Kathryn Lovegrove
Contents
- The Inverse Relationship between the Incidence of Infectious diseases and the Immune diseases
Introduction
In 1989 David P Strachan published a paper that described and formulated the Hygiene Hypothesis to explain the findings from a number of studies that the regular exposure to allergens early in life may help improve the natural immune system against developing allergies (and other immune diseases) in later life (Strachan DP, 1989). The hypothesis also explains the alternative inverse relationship that an antiseptic clean environment (i.e., excessive cleanliness in Western nations) may be implicated in the rise of immune disease. This essay focuses on the background to this theory, the underlying immune principles and its relevance to public health and education. Although the Hygiene Hypothesis remains compelling, opposing arguments that question its basis are considered at the end.
Definitions of Immune Disease
![]() The following is knowledge we accumulated during our Physiology Course.
The following is knowledge we accumulated during our Physiology Course.
It is evident that if a pathogen infects the body, an immune response will occur and in some cases, it causes the immune system to attack self-cells which it considers to be foreign bodies.
Infectious and Immune diseases occur in all animals and are both a result of pathogenic organisms directly or indirectly entering the body. Examples of pathogens include bacteria, viruses, fungi and parasites. With a strong immune system, the body is capable of defending itself by producing antibodies against of the infection or disease. However, as a result of an autoimmune condition, the immune system produce antibodies that begin to attack self-cells, such as organs and tissue. This is called an immune disease.
The Immune Response / Mechanisms of Action
In order to discuss this hypothesis further, the basic function of the Immune System will be discussed.
There are two major types of an Immune system: Innate (non - specific) and Acquired (specific).
Innate Immune System
The Innate Immune system is a non-specific form of Immunity used to kill invading foreign bodies. The cells of the Innate Immune system including Macrophages, Granulocytes and Natural Killer Cells do not need to have recognised the invading substance before. It is activated and provides an effect immediately. It does not have a memory function and therefore does not provide lifelong immunity towards infectious diseases.
Acquired/Specific Immune System
The Acquired/Specific Immune System is used to remove non self-particles through the production of Antibodies. There are two types of Acquired Immunity: Cellular involving T Lymphocytes and Humeral Involving B Lymphocytes. Both types are present during an Immune Response. The acquired system has a memory function and will be able to produce antibodies against the pathogen should it ever invade the body again. This is based on the fact that Memory T and Memory B cells are present from previous immune responses, and will recognise Antigens that have previously entered the body, and then stimulate Antibody production against them. They both remain in the body long after the antigen has left the body. It could be said that Memory B cells are more effective, because they cause direct production of the Antibody against the Antigen. However, T cells do not produce Antibodies, and so the Helper T cells release Cytokines (messenger molecules) which stimulate B cells to produce Antibodies against the Antigen.
MHC and its role in self-recognition
In order for an effective Immune Response the body must be able to distinguish between self and Non Self Cells. There is only one type of material against of which the immune system does not produce antibody. This is the Major Histocompatibility Complex I and II (MHC I and MHC II). MHC- I complexes are found on the surface of all nucleated cells. MHC - II complexes are found on the surface of Antigen Presenting Cells (APC) e.g. Macrophages/ Dendritic Cells. Antigen Presentation is a process where cells such as Antigen Presenting Cells, ingest invading particles by phagocytosis and then present their Antigen to the T lymphocyte. Then Antibodies can be produced against the Antigen, so should it enter the body again a very quick immune response will occur, involving direct production of that specific antibody again.
Production of B-Lymphocytes
In both Humeral and Cellular Immunity there is an Antigen Independent Stage and an Antigen Dependent Stage. During the Antigen Independent Stage of Humeral Immunity, Pre B Lymphocyte matures in the bone marrow and become Virgin B Lymphocytes. The Virgin B Lymphocyte enters the circulation, where the Antigen Dependent Stage starts. The B lymphocyte binds to the Antigen which is bound to the APC. If it has the appropriate IgG like molecule on its surface which is specific for that Antigen, the B lymphocyte will be activated. During binding of the B lymphocyte and the Antigen, Cytokines are released which cause activation of the B lymphocyte provided that the Ig is specific to the Antigen. Activation may be Th- independent or Th-dependent (Th=T helper cell). Once the B lymphocyte is activated, it goes to the secondary lymphatic organ where it proliferates to a Plasma cell. The plasma cell makes the Antibodies (Immunoglobulin). Some change into Memory B cells, which allow for long term immunity.
Production of T-Lymphocytes
Cellular Immunity also involves an Antigen Independent and Dependent Stage. During the Antigen Independent Stage the Pre T Lymphocyte changes into a Virgin T Lymphocyte. On the surface of each virgin-T-lymphocyte there will be an Ig-like molecule (TCR) appearing against a certain possible antigen structure. This is referred to as a Ti Cell (T Initiator cell). Once this T-Initiator cell enters the blood, the Antigen dependent stage starts. When the T - Initiator cell has the appropriate Ig against the Antigen, and the CD4 Cell Surface Antigen, it will recognise an Antigen on an Antigen Presenting Cell with the MHC - II complex. The linkage between the AP cell and the Ti-cell will result in the primary stimulation. Ti Cells with the CD4 cell surface antigen and the appropriate Ig like structure will bind to an Antigen that is on and AP cell with the MHC II complex. This will cause the proliferation of T Helper cells via Blastic Transformation.
(Ti cell + Ig like structure + CD4 cell surface Antigen) + (AP cell + MHC - II ) = T Helper cell.
Ti cells with the CD8 Cell Surface Antigen and appropriate Ig like structure, will recognise Antigens on APC cells with the MHC - I complexes, and form T Cytotoxic cells.
(Ti cell + Ig like structure + CD8 cell surface Antigen) + (AP cell + MHC - I ) = T cytotoxic cell.
T cells will only activate and cause immune responses if they have bound to a cell containing an APC containing a MHC complex on its cell surface. During the Blastic transformation some other kinds of T-cells develop as well: Ts = suppressor (it compensates the aggressive Tc-cell (cytotoxic) activity), and Tm-cells (memory cells).
Cytotoxic T cells with the CD8 cell surface antigen will recognise cells and kill virally infected or tumour/ mutant cells. T Helper cells with the CD4 Cell Surface Antigen will develop into Th1 and Th 2 cells. Th1 cells stimulate B cells to produce Antibodies. Th 2 cells will cause Macrophages to be activated and cause cellular bacteria to be destroyed.
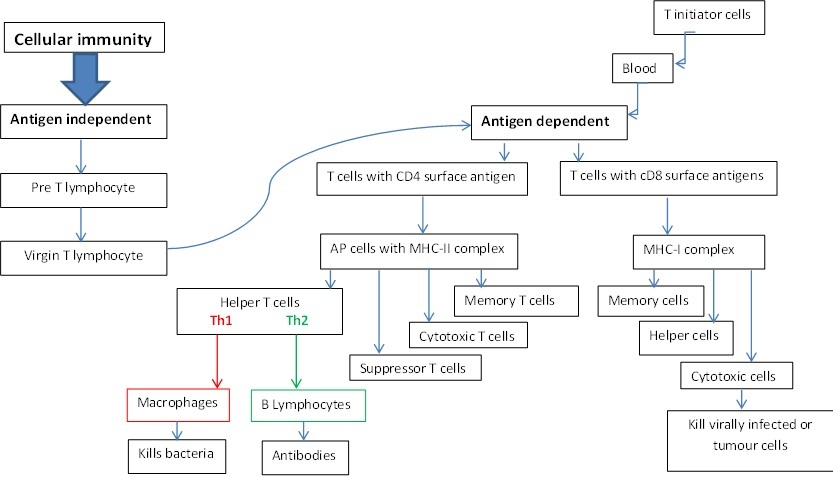
Figure 1: A flowchart illustrating Cellular Immunity
A link between the Innate and the Adaptive Immune System
It was found that fruit flies have a Toll Receptor which is responsible for recognising microorganisms and activating the Innate Immune system. The same type of receptor can be found in mammalian species which is called the Toll – like receptor. Therefore the innate system cannot be called totally “non-specific”. TLR’s can be found on the surface of Dendritic cells (DC), and on the surface of T and B cells. DCs are the coordinator of the immune system building a bridge between the adaptive and innate immune system. They engulf the microorganism, process it and express its MHC receptor. This is how the DC presents the microorganism to the B or T cell. Processes involving antibody production then start as part a Specific/Adaptive Immune response.
Gender differences in Infectious and Autoimmune diseases
Infectious Diseases
Through studies it has been shown that there are differences in the vulnerability to infectious diseases in the sexes. This has been defined by a search of the world’s literature and a study of the Johns Hopkins Hospital case records covering the period from 1930 to 1963. It has been seen that there is a male dominance in all the data, especially at infancy. This is also the period in which infections by Gram-Negative (Gram (stain type) negative enteric rods are rod-shaped bacteria that usually are found as single individual cells.) enteric bacilli outnumber those by Gram-positive organisms and this difference affects males more than females. This has been countered by the invention of antibiotics and treatment that has formed an increased sex ratio (Thomas C. Washburn et Al., 1964).
The cause of the sex differences in susceptibility can be seen by the different genes in male and female. Males have two different chromosomes – XY, while females have homologous chromosomes – XX. It would stand to reason then, that males would have a greater resistance to infectious diseases as they could produce a more random combination of genes, making it more difficult for the bacteria to infect them.
"In an experiment the immune response to a protein antigen (BSA, bovine serum albumin) was compared in male and female mice. It was found that female mice have developed a stronger and longer lasting immune response and that female mice were more responsive to small doses of antigen." (G. Terres et Al., 2012)
The major difference between the mice would be the concentration of oestrogen. Several cells of the immune system including dendritic cells (DCs), natural killer cells, macrophages, and lymphocytes express oestrogen receptors, suggesting that this hormone modulates their function. Unfortunately, this difference is also thought to play an important role in the higher susceptibility of women to autoimmune diseases such as lupus, rheumatoid arthritis, and multiple sclerosis(Verthelyi, 2006).
Autoimmune Diseases
An example of an autoimmune disease is Multiple Sclerosis (MS). It is an inflammatory disease in which the fatty myelin sheaths around the axons of the brain and spinal cord are damaged, leading to demyelination and scarring. Disease onset usually occurs in young adults, and it is more common in women. Multiple Sclerosis was differentiated and 'framed' as a separate identifiable entity by von Frerichs, Vulpian, and Charcot others in the mid-nineteenth century (T. Jock Murray, 2009).
Multiple Sclerosis affects the ability of nerve cells in the brain and spinal cord to communicate with each other effectively. Nerve cells communicate by sending electrical signals called action potentials down long fibres called axons, which are contained within an insulating substance called myelin. In MS, the body’s own immune system attacks and causes damage to the myelin. When myelin is lost, the axons can no longer effectively conduct signals. The name multiple sclerosis refers to scars (sclerosis – better known as plaques or lesions) particularly in the white matter of the brain and spinal cord, which is mainly composed of myelin.
Among people who develop MS before the age of 20, women outnumber men by three to one (3:1 ratio). Looking at people of all ages, at least twice as many women as men are living with MS. Early studies in animals show that testosterone may be protective, and researchers think that this could explain why men develop MS less often and typically later in life than women. However, when men develop MS, it is usually more severe and progressive. They are more likely to develop Primary Progressive Multiple Sclerosis (PPMS). Compared with relapse - onset multiple sclerosis, people with PPMS are older at onset and a higher proportion are men (David. H. Miller, 2007) . In this form of MS, there is a smaller chance of recovery so men with PPMS deteriorate at a faster rate, having more mobility, bowel, and bladder problems than would be seen in a women with MS.
What is the Hygiene Hypothesis?
The Hygiene Hypothesis suggests that current increase in the amount of people suffering from Immune diseases is caused due to a lack of exposure to pathogenic substances. Although the exact cause of this is still debatable, the Hygiene Hypothesis suggests that if the body does not receive enough stimuli to develop the T Suppressor Cells (which regulate and control the Immune Response), a Th1/ Th2 cell imbalance will be caused. T-helper cells are generally subdivided into types 1 and 2 (TH1 and TH2 respectively). This division reflects a functional difference between these two cell types; TH1 cells are part of the cellular and TH2 cells, the humeral system. Th1 cells cause the action of Cytotoxic T cells and Macrophages, while Th2 cells cause the production of Antibodies. A healthy immune system is both balanced and dynamic: it should be balanced between Th1 and Th2 activity, switching back and forth between the two as needed. This allows for a quick eradication of a threat and then a return to balance before responding to the next threat. During a Th1/Th2 cell imbalance, when an antigen invades the body, a Th - 2 cell mediated response will be more likely to be initiated, rather than a Th - 1 mediated response. Th1 cells promote cell-mediated immunity while Th2 cells induce humeral immunity. The danger of this is when the Th - 2 mediated response is dominated, the immune system will be in a state of Hyperactivity, and so will begin to produce antibodies against harmless antigens (Allergy), or even worse against its own cells (Autoimmune disease). (Sergio Romagnani, 2004)
Both humans and other mammalian diseases are influenced by genetic and environment factors. In the case of some immune diseases, such as allergic hypersensitivity and rhinitis, studies have indicated an inverse relationship between their prevalence in later life and early exposure to allergens in the environment. David Strachan observed that allergic diseases such as Hay Fever were far more prevalent in families with one child than with many children(D. P Strachan, 2000). This is because larger families experience greater exposure to many more different types of pathogens. David Strachan developed and published the ‘Hygiene Hypothesis’ in 1989 to then explain this relationship. It states that "a lack of early childhood exposure to infectious agents, symbiotic microorganisms (e.g., gut flora or probiotics), and parasites increases susceptibility to allergic diseases by suppressing natural development of the immune system". (Bianca Schaub et Al., 2006) (Andrew H. Liu et Al., 2003)
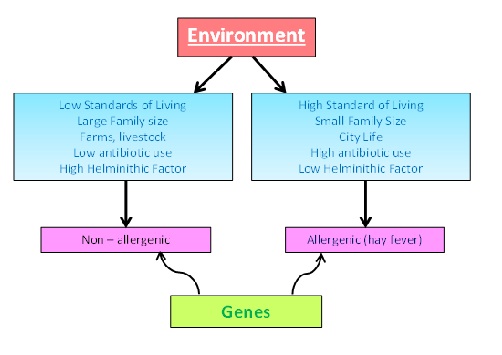
Figure 2: Factors contributing to non-allergic and allergic susceptibility
Background to the theory / Supporting Evidence
This hypothesis has been observed and supported by a number of studies.
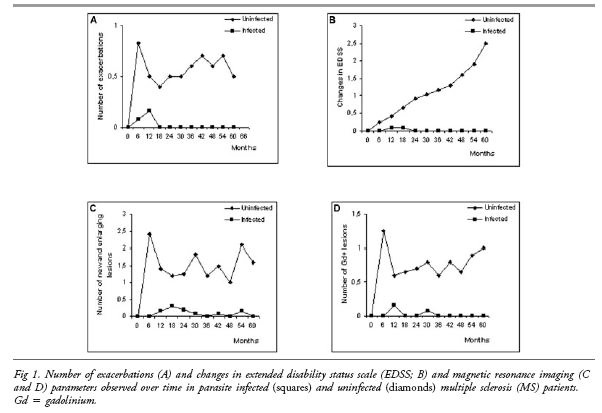
Helminithic Therapy
One study that contributes to the theory of hygiene hypothesis is provided by the experiment that was carried out with Pig worms (trichuris suic) and Multiple Sclerosis. Trichuris suic cause an immune response without causing infection to the human body. In an experiment carried out by Correale and Farez (2007), 36 test subjects were studied for 4.7 years; 12 MS patients infected with worms, 12 uninfected MS patients and 12 Healthy individuals. They were regularly monitored over the test period. It was concluded that the intestinal worms slowed the advancement of symptoms in the test subjects with MS. The 12 uninfected MS patients had, however, rapidly progressive symptoms. The 12 healthy individuals remained uninfected with worms and had not changed. In the advancement of health and the continued emphasis of hygiene, parasitic infection has decreased. Therefore, the positive effects of worm infections has been lost. Other cases of the positive effects of worm infection can be seen Ulcerus Collitus, which caused a 43% improvement in patients. 72% improvement in Chrone’s disease was also seen. The intestinal worms evolved to survive in the human body without being attacked by the immune system by reducing the inflammatory response mediated by regulatory T-cells. The inflammatory response is decreased even more by the host, who has learned to adapt. (Stephen Stearns, 2008)
Figure 3: Graph showing the difference between infected and non - infected MS patients, with trichuris Suic.
Celiac Disease
Celiac disease is an Autoimmune Disease, caused by a reaction to the Gliadin (Gluten protein) found in Wheat, and other crops e.g. Rye and Barley. It causes digestive problems and the inability of the intestine to absorb nutrients. When people who have the disease ingest foods containing gluten, their immune system begins to attack itself by destroying villi of the small intestine. Celiac Disease is four times more prevalent today than half a century ago. Why the prevalence of Celiac Disease may have increased over time is not clear(Alberto Rubio Tapia MD et Al, 2011). This is too short a time period for substantial changes in human genetics and likely represents some major and pervasive environmental influence(Alberto Rubio Tapia MD et Al, 2011). Changes in the way cereals are grown and processed could be causing modifications to their structure and composition, but it is unclear how this affects the increase in the disease. A second environmental factor that may be contributing to the increase in celiac disease is what is known as the hygiene hypothesis. It describes how the body must be exposed to different bacteria, and pathogens in order for it to develop properly. In today’s society, increasing hygiene standards make the environment almost too clean particularly in the Western World. Free healthcare programmes and increased availability to all types of medicine in the Western World is decreasing the development of our immune systems. This is affecting children especially, as they become more susceptible to allergies and immune disorders. However, it could be said that in the Third World, especially in large cities with millions of inhabitants e.g. Kolkata, where there is a much lower standard of hygiene, there is also a reduced amount of people suffering from Celiac Disease and other Immune disorders. People are exposed to more pathogens, and this results in a better developed immune system.
Exposure on Farms
As we have already explained, a lack of exposure to infectious pathogens at a young age prevents natural improvement of the immune system. A weaker immune system is less beneficial and at a later stage of life, will be more susceptible to attack. A farm environment is an example of where natural exposure to pathogens can be obtained. There are high number of diseases which although do not affect an animal, can be infectious to humans. The prevalence of Escherichia coli 0157 displays striking variability across the Scottish cattle population (L. Matthews et Al, 2005). This type of E coli can then be transmitted to humans. Faeces, urine, feed, bedding, and mud contain bacteria; bacteria that are potentially damaging to humans. These aspects leave for an unhygienic environment.
Studies were carried out to understand whether the direct contact with animals, in this case farm animals, provided a greater degree of protection from the development of allergic diseases. An allergic disease is a result of the immune system being hyper sensitive and its excessive stimulation as a direct consequence of usually harmless bodies of the environment. It was concluded that exposure to a farming environment did benefit a person’s immunity and that interaction at a younger age continuously until adulthood bestowed increased defense (E. Von Mutius, 2010).
Pasteurisation
Pasteurisation of milk was discovered by Louis Pasteur in 1864. The methods of continuous heating and cooling of a liquid rids of any unwanted pathogens that may cause infectious diseases. Some examples include the harmful Ecoli O157 and mycobacterium Bovis (G.S. William, 1943). Although this treatment to the milk we drink has prevented disease, has it also resulted in a greater susceptibility to allergic diseases and immune diseases later on? Another study has shown that the ingestion of unprocessed animal products, such as milk has reduced proneness to asthma and allergies during childhood (E. Von Mutius, 2010).
Laboratory Rats VS Wild Rats
Laboratory specimens live in a germ and parasitic free environment. They receive extensive medical care that would rival human medical care in westernised societies. On the other hand, however, their wild counterparts are exposed to many diseases, microbes, infections and viruses. Examples of rodents that are found both in the laboratory and the wild are the House Mouse and the Common Rat (Rattus Norvegicus).
An experiment was carried out to investigate the relationship between the number of Immunoglobulin (Ig) in the serum of lab rats and of wild rats. The IgG is involved in autoimmune disease while IgE deals with foreign organisms infiltrating the host organism. The results show that wild rodents had higher levels of IgG and IgE compared with the lab rats. It would seem that wild rats would have a negative outcome from this increase in Ig's and be more susceptible to auto-immune disease. However, because they were exposed to more antigens, the wild rats had developed a greater number of antibodies as protection while laboratory rats unexposed to these conditions had not. This is a result of the auto reactive IgG's binding to the body’s own cells.
These results are consistent with the idea that animals without access to modern medicine have high levels of autoimmune-like and allergic-like immune responses that represent appropriate responses to unknown factors in their environment (A. P. Devalapalli, et Al, 2006).
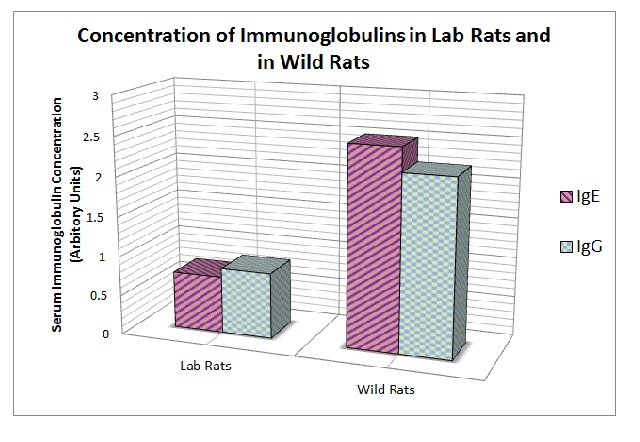
Figure 4: Concentration of Immunoglobulins in Lab Rats and Wild Rats
Relevance to Public Health and how we live
Studies that support the Hygiene Hypothesis should influence our attitude to Public Health especially in Westernised countries where ‘excessive’ cleanliness in the home and during early childhood is encouraged and considered to be correct. Perhaps societies should regard ‘excessive’ domestic cleanliness as something to be avoided so that our immune systems are exposed and sensitised to as wide variety of antigens as possible, - to ‘future proof’ us against the development of immune diseases, such as asthma, in later life. This message should perhaps be included as part of our school and public education systems and media.
Application to Veterinary Practice
Veterinary medical practice has also seen an improvement in the hygiene of working conditions and utensils. We note a more sterile environment such as the decontamination of forceps and scalpels in an autoclave and in surgery where physicians "scrub up” before entering a ‘clean‘ i.e. ‘sterile‘ operating theatre. Furthermore, there is an expansion in the amount of medicines available. Hungary, before the fall of communism had 75 remedies, now there is more than 2000 available treatments in which we can administer to patients. We can apply the hygiene hypothesis to the veterinary situation also. Although we see an increase in cleanliness to improve the heath of animals, it may work to our detriment in causing almost as much harm as it rectifies.
Arguments against the Hygiene Hypothesis
The Hygiene Hypothesis remains a ‘hypotheses’ and several studies have been conducted that question its validity. In 1992, data were gathered about intercity African American children in the United States, who have very high numbers of asthma. The study showed that many of these children had been sensitized to common allergens found around them; however, they still developed asthma at the same rate as those children who were not sensitized to the same allergens (R. Call et Al, 1992). In addition to this finding it is accepted that some allergies have a genetic component. A child who has two parents with allergies has a 75% chance of also developing allergies. There are genetic links that have been found between certain types of allergic responses which complicates the idea of how much immunity is inherited and how much can be developed (Alberto Rubio Tapia MD et Al, 2011).
Conclusion
The question as to whether there is an inverse relationship between the incidence of infectious diseases and the immune diseases cannot be answered without difficulty. Scientists have been and are still examining this matter for years, providing evidence that contradicts or builds upon previous findings.
Evidence that there is an inverse relationship includes the discovery of the ‘Hygiene Hypothesis’. Devised in 1964, this theory explains that living in a clean environment may have adverse effects, leading to a greater susceptibility to immune disorders later in life. This is thought to be due to a lack of interaction with infectious diseases from an early age.
Adding to the evidence of this relationship, a graph taken from reports of the ‘Centres for Disease Control and Prevention’ indicates a definite decrease in the incidence of infectious diseases between the years of 1950 and 2000. Although some mild abnormalities, the negative correlation between the two criteria is evident for all five diseases analysed. The subsequent graph taken from ‘Swarbrick et al’ illustrates that the incidence of immune disorders increases between the years of 1950 and 2000.
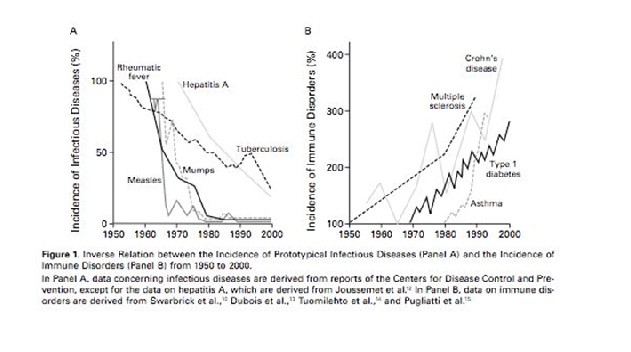
Figure 5: Graph showing the inverse relationship between the incidence of Prototypical Infectious Diseases and the Incidence of Immune Disorders from 1950 - 2000
Although there is strong evidence to support the fact that hygiene is beneficial to the human race and the animal kingdom, the degree of cleanliness should be monitored. The number of bacterium we are exposed to and the extent of our own personal hygiene must be in balance i.e. we cannot completely eradicate our exposure to bacteria without negative effects on our own health.
Our own opinion agrees therefore, with the title that there is an inverse relationship between infectious and immune diseases.
![]()
Bibliography
►A. P. Devalapalli, A. Lesher, K. Shieh, J. S. Solow, M. L. Everett, A. S. Edala, P. Whitt, R. R. Long, N. Newton, W. Parker - 2006 - Increased Levels of IgE and Autoreactive, Polyreactive IgG in Wild Rodents: Implications for the Hygiene Hypothesis - Scandinavian Journal of Immunology
►Alberto Rubio Tapia MD, Joseph A. Murray MD, - March 2011 - Celiac Disease - US National LIbrary of Medicine, National Institutes of Health.
►Andrew H. Liu, James R. Murphy - 2003 - Hygiene hypothesis: Fact or fiction? - Journal of Allergy and Clinical Immunology
►Bianca Schaub, Roger Lauener, Erika von Mutius - 2006 - The many faces of the hygiene hypothesis - Journal of Allergy and Clinical Immunology
►D. P. Strachan - 2000 - Family size, infection and atopy: the first decade of the 'hygiene hypothesis' - Thorax
►David H. Miller - October 2007 - Primary Progressive Multiple Sclerosis - Lancet Neural.
►E., von Mutius - 2010 - 99th Dahlem conference on infection, inflammation and chronic inflammatory disorders: farm lifestyles and the hygiene hypothesis - Pub Med Central Article
►G.S. William - 1943 - The Pasteurization of Milk - Br Med J
►G. Terres, S. L. Morrison and G. S. Habicht. s.l. - 2012 - A Quantative Difference in the Immune Response between Male and Female Mice - Experimental Biology and Medicine.
►T. Jock Murray - 2009 - The History of multiple sclerosis is : the changing frame of the disease over the centuries - Journal of Neurological Sciences.
►L. Matthews, I.J. McKendrick, H. Ternent, G. J. Gunn, B. Synge, and M.E. J. Woolhouse - March 2005 - Super shedding cattle and the transmission dynamics of Escherichia Coli 0157 - Epidemiology and Infection.
►R. Call, T. Smith, E. Morris, M. Chapman, T. Platts-Mills - December 1992 - Risk factors for asthma in inner city children - The Journal of Pediatrics
►Sergio Romagnani - 2004 - The increased prevalence of allergy and the hygiene hypothesis: missing immune deviation, reduced immune suppression, or both? - Immunology
►Stearns, Stephen - 2008 - Pig worms and multiple sclerosis: the unintended consequences of hygiene - Evolution and Medecine Review
►Strachan DP - 1989 - Hay fever, hygiene, and household size - BMJ
►Thomas C. Washburn, Donald N. Medearis Jr. Barton Childs. s.l. - 1964 - Sex Differences in Susceptibility to Infections - Pediatrics
►Verthelyi, Daniela - 2006 - Female’s Heightened Immune Status: Estrogen, T Cells, and Inducible Nitric Oxide Synthase in the Balance - Endocrinology
Figure Referencing
Figure 1: Flowchart, illustrated by Kathryn Lovegrove, Maria Mulvihill, Serena Iceton
Figure 2: Diagram, illustrated by Kathryn Lovegrove, Maria Mulvihill, Serena Iceton
Figure 3: Graph, Stephen Stearns - 2008 - Pig worms and multiple sclerosis: the unintended consequences of hygiene - Evolution and Medecine Review
Figure 4: Graph, illustrated by Kathryn Lovegrove, Maria Mulvihill, Serena Iceton; data taken from: P. Devalapalli et Al - 2006 - Increased Levels of IgE and Autoreactive, Polyreactive IgG in Wild Rodents: Implications for the Hygiene Hypothesis - Scandinavian Journal of Immunology
Figure 5: Graph, Stephen Stearns - 2008 - Pig worms and multiple sclerosis: the unintended consequences of hygiene - Evolution and Medecine Review