Itt írjon a(z) ImmunhemolyticAnemia-ról/ről <>
The pathogenesis and characteristics of the Immune mediated hemolytic anemia (IMHA) in dogs and cats
Santama Eleni Lea, Pavlidou Mikaela, Modestou Stylianos
Contents
Introduction
Paul Ehrlich in the beginning of the 20th Century proposed the idea of “horror autotoxicus”. This idea suggested that any biological organism is able to endure and recognise its own tissue. However, had the above system become intolerant, an autoimmune disease would be caused.[1] In the following passage the definition of Immune Mediated Haemolytic Anaemia will be discussed in depth. Following, its causes will be detailed using data retrieved from various scientific articles and specialisation books. Moreover, the symptoms presented in the disease will be stated, that one along with the diagnostic methods and tests can use to identify the disease. Lastly, the treatments available and their effectiveness will be mentioned, using proof from the findings collected from the aforementioned sources.
What is Immune Mediated Haemolytic Anaemia
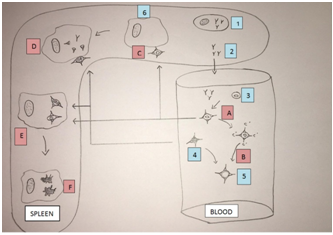
Immune anaemia is caused due to antibody adherence to the cell membrane of a red blood cell which may or may not have a complement fixation. This interaction causes the red blood cell to become spherical which reduces their lifespan by either causing their lysis by the monocytes and phagocytes of the body’s immune system or when the cell membrane forms a complement with the immunoglobulins and an attack complex is created which causes intravascular haemolysis. (Fig. 1)
|
Fig. 1 1 – Lymphocyte, 2 - Free Antibodies, 3 – Erythrocyte, 4 – Spherocyte, 5 – Ghost Erythrocyte, 6 – Macrophage A – Complement reaction, B – Intravascular haemolysis, C – Attachment to macrophage, D – Partial phagocytosis, E – Erythrophagocytosis, F – Extravascular haemolysis.
Immune mediated haemolytic anaemia is serologically caused by two types of antibodies (or no detectable antibodies): warm-antibodies (usually IgG or IgA), cold-antibodies(usually IgM). Further classification exists when considering the causes, Idiopathic (primary) and Symptomatic (secondary) immune haemolytic anaemias. The above could be even further categorised as being isoimmune, drug-induced, associated with infectious disease or associated with lymphoid or other malignancy.
Idiopathic Immune Haemolytic Anaemia
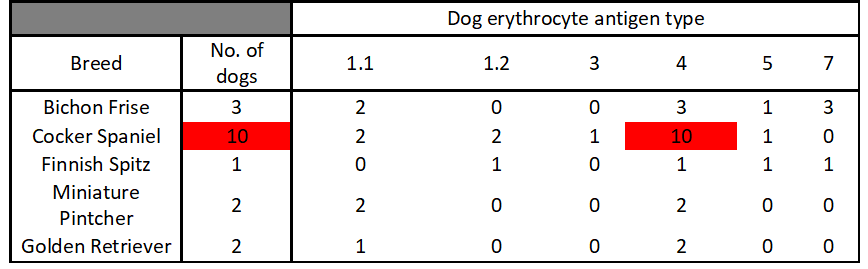
Most commonly observed in dogs and cats but probably occurs in all species. All breeds of dogs may be affected especially Cocker Spaniels. Other susceptible breeds are Bichon Frise, Miniature Pinschers, Rough-coated Collies, and Finnish Spitz. Sex is also considered to play a role in IMHA development as there are more cases of IMHA in females especially spayed ones. Blood type is assumed to play a role in the susceptibility for the disease, with DEA4 being the most common.[2]
|
Table 1 The most common blood type among dogs with Immune Mediated Haemolytic Anaemia was DEA 4 and Cocker Spaniels seem to be the most susceptible to the disease[3]
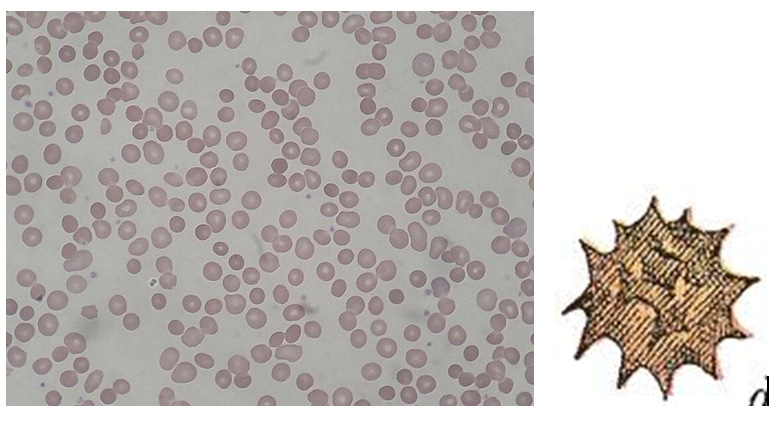
When viewed under the microscope anaemia is macrocytic and slightly hypochromic, with a normal haemoglobin concentration. Spherocytosis, leptocytosis and marked anisocytosis are observed. (Fig. 3)
|
Fig. 2 Normal Red blood cells (EM) [4]
|
Fig. 3 Spherocytes [5]
It is commonly referred to as autoimmune haemolytic anaemia since the factors that initiated the immune haemolysis are unclear. They have been however, associated with infections, neoplasia and vaccinations, thus may not be autoimmune.
Causative Agents
Drug-induced Haemolytic Anaemia
Many drugs have been observed to cause immune thrombocytopenia and these same drugs are linked to Coombs-positive haemolytic anaemia. Some of these drugs are: quinidine, quinine (tonic water), penicillin, insecticides, chloropromazine and dipyrone. [6] More specifically in cats propylthiouracil [7] and in dogs cephalosporins, levamisole [8] and pirimicarb [9] are also highly associated with the above observation. It is usually highly specific with some drugs needing only small doses to cause the disease.[10] Haemolytic anaemia caused by drugs is said to have two types. One type, is induced when an antibody reacts solely with the drug-exposed cells; while the second type, the reaction of the antibody and the red blood cells when the drug is not present. The latter one had it not been for the history of drug exposure and aggravation with retreatment, would have been confused with autoimmune haemolytic anaemia.[11]
Vaccine-induced Haemolytic Anaemia
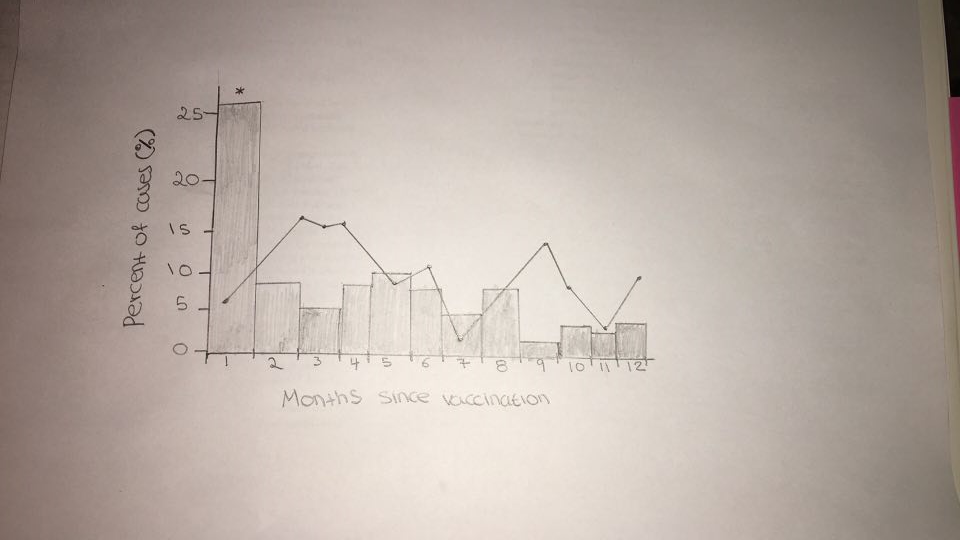
Some sources seem to suggest a correlation between the use of vaccines and the development of Immune Mediated Haemolytic Anaemia. One of these studies conducted by Derek Duval and Urs Giger which tested 58 dogs over a 27 month period and compared to a randomly selected control group comprising of 70 dogs simultaneously with the non-control group. “Fifteen of the dogs (26%) had been vaccinated within 1 month of developing IMHA”. (Fig. 4) The control group saw no increase in the frequency of appearance of the disease. “In the recently vaccinated dogs; combination vaccines from various manufacturers against canine distemper, adenovirus type II, leptospirosis, parainfluenza and parvovirus (DHLPP) were involved in each case”. Two groups were created, one including the “dogs vaccinated within 1 month of developing IMHA and the other which included dogs that developed IMHA more than 1 month after vaccination”. The former group showed a significantly decreased platelet number and “a trend towards increased prevalence of intravascular haemolysis and autoagglutination” when compared to the latter group.[12]
|
Fig. 4 A comparison of the appearance of IMHA between the vaccine and non-vaccine group Control group represented by black solid line The majority of the non-control group developed Immune Mediated Haemolytic Anaemia a month after vaccination [13]
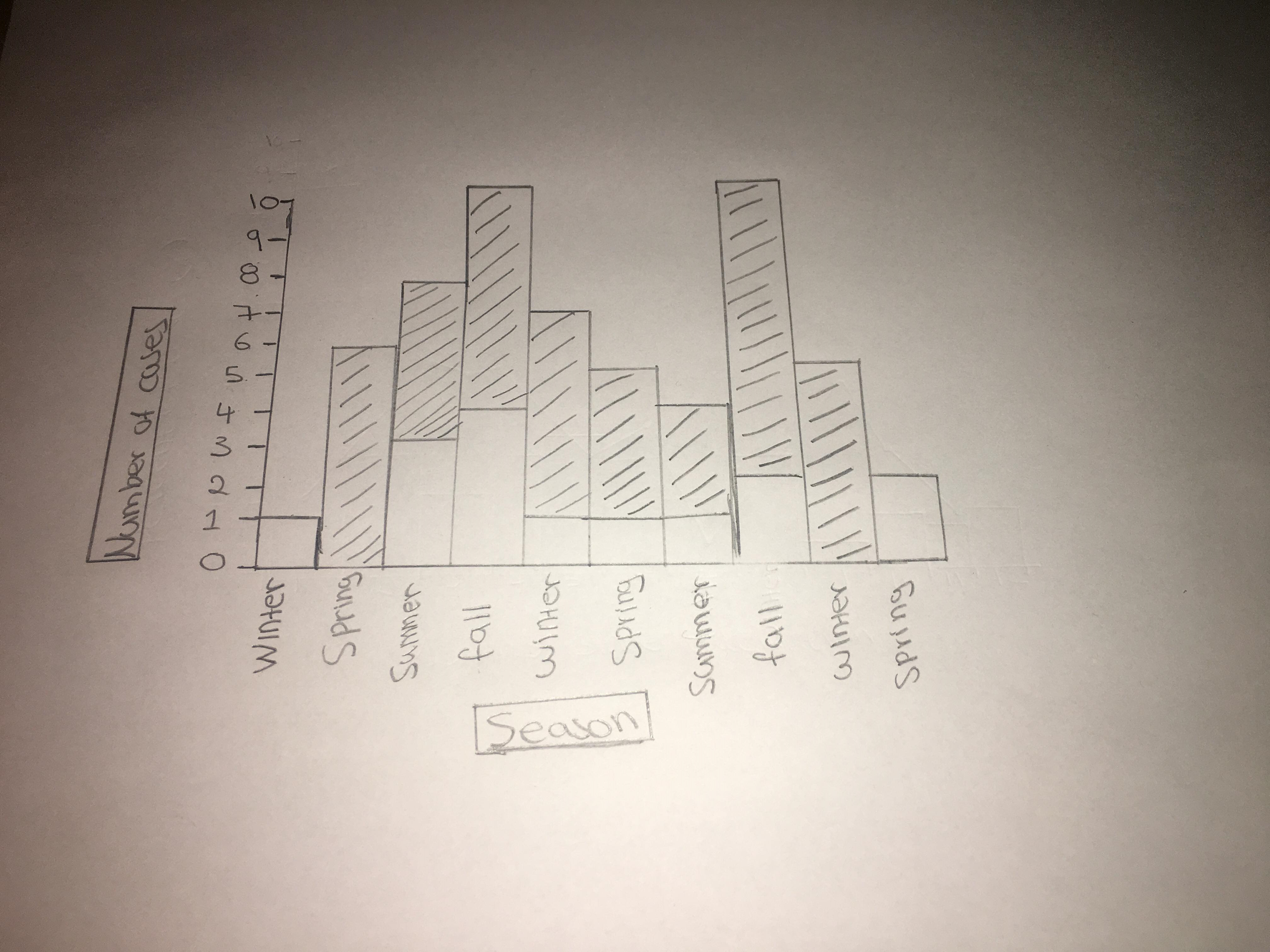
Seasonality may also affect the development of Immune Mediated Haemolytic Anaemia since in the fall there was a slight increase in its appearance both dog groups [14] (Fig. 5)
|
Fig. 5 The effect of seasonality
IMHA provides a high mortality rate in both vaccine and non-vaccine groups, with the vaccine group having a higher mortality rate, “with the majority of fatalities (>75%) occurring in the first 3 weeks after presentation.” In conclusion, vaccines have a positive correlation in the appearance of Immune Mediated Haemolytic Anaemia.
Infectious Haemolytic Anaemia
Infectious agents have also been reported to cause haemolytic anaemia, some of them being:
- Ehrlichiosis (caused by Ehrilichia species)
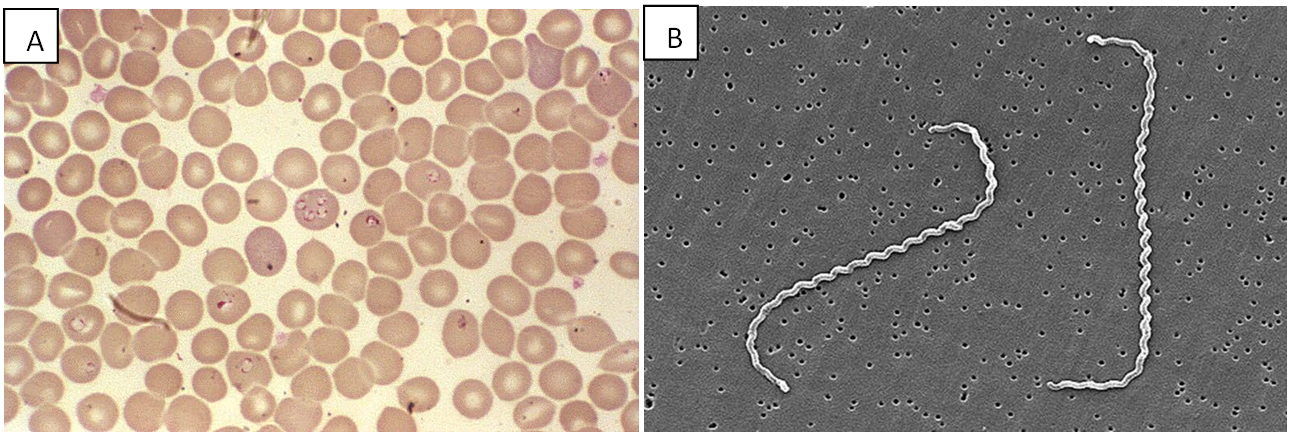
- Babesiosis (caused by Babesia species) (Fig. 6)
- Anaplasma phagocytophilum
- Haemobartonella canis
- Leptospirosis (caused by Leptospira species) [15] (Fig. 6)
|
Fig. 6 A. Babesia species parasites in mammalian cells B. Leptospira species (EM) [16]
Other
In cats, Feline Leukemia Virus(FeLV) and Feline Immunodeficiency Virus (FIV) , Feline Infectious Peritonitis (FIP) and Cytauxzoon felis are among the most frequent causes of IMHA, even though AIHA can also occur. [17] Incompatible blood transfusion in both dogs and cats may lead to haemolytic anaemia developing. This can be prevented however, with blood testing and crossmatching tests.
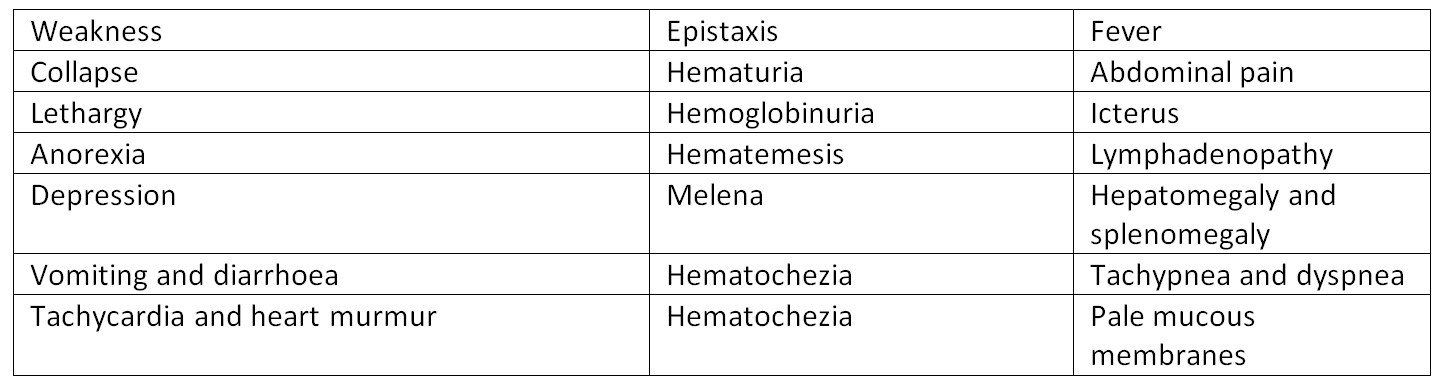
Symptoms
In both dogs and cats the following symptoms may be observed:
|
Table 2 The observed symptoms [18], [19], [20]
Diagnosis and Treatment
“Detection of microspherocytes in a blood smear is almost proof of IMHA but recognition may be difficult, especially in the cat”. [21]
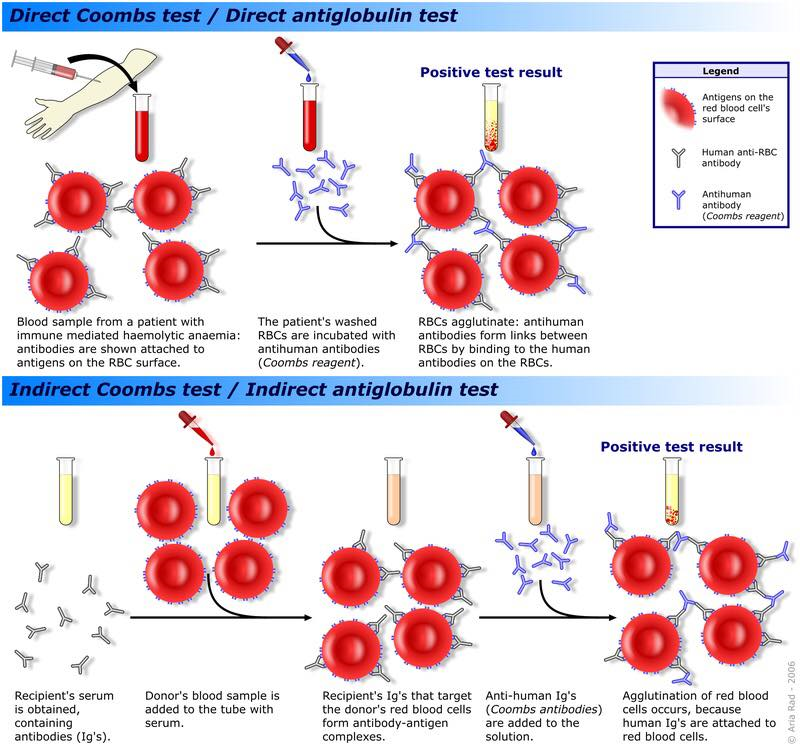
Coombs Test
The aim of the test is to detect the presence of immunoglobulins directly or indirectly bound to the red blood cells (ESAIg) or complement on red blood cells. Most frequently used in the detection of Immune Haemolytic Anaemia. An antiglobulin for the intended species (eg. dog) in prepared in another species(eg. sheep or rabbit). Method: The patient’s red blood cells are washed thrice with saline solution in order to remove the unbound proteins. Antiglobulins are then added (eg. Anti-IgG) which will bind to the corresponding immunoglobulins. A positive reaction occurs when agglutination is observed indicating that the erythrocytes are coated with C3 molecules or approximately 500 molecules of immunoglobulins. (Fig. 7)
|
Fig. 7 Coombs Test as a diagnostic tool for Immune Mediated Haemolytic Anaemia[22]
Usually cases of immune anaemia are beneath the sensitivity of the reagents of the Coombs test therefore, false positives and false negatives can be observed. In cats Coombs test has been proven as a less reliable method in identifying IMHA. The above issue has been expressed in an article where Coombs test was performed on 92 cats. The results were: “negative in 5 healthy, in 9 sick non-anaemic, and in 55 cats with different types of anaemia, and positive in 18 anaemic cats.” [23]
Treatments
Some of the existing treatments are blood transfusions, crystalloids, antibiotics. [24]
Immunosupression
-Glucocorticoid treatment: Is the primary choice of treatment. “They reduce the phagocytosis in red blood cells, complement fixation, antibody production and inflammation. Typically, prednisolone is used or another choice is dexamethasone. Cats require a higher dose than dogs.” [25, 26, 27]
-Cyclosporine: “has also been used as an immunosuppressant when combined with other drugs.” [28, 29]
Supportive Therapy
-Doxycycline: indicated for Mycoplasma infection
-H2-blockers [30]
However, even with the above mentioned treatments being available, some patients do not respond positively to them, leading to immediate death. And even if they ultimately survive, cases of relapse have been reported to frequently occur. [31]
Conclusion
All in all, Immune Mediated Haemolytic Anaemia is a dreadful disease that many animals succumb to, since as implied by the data collected it has a very high mortality rate. The many causes of this disease ranging from drugs, vaccines and infections make it a tough disease to tackle even though there are a number of tests available to make a diagnosis. Even though the Coombs test is available to make a diagnosis in time; the data mentioned above suggest that it is inefficient, because of the appearance of false positives and false negatives, thus making the situation even more complicated. Although many treatments are available for the patients, they seem to not be very effective, since many do not respond to the drug used and even if there is survival, relapses occur. In the upcoming years more researches will be conducted broadening the knowledge available for this disease and hopefully finding more efficient treatment possibilities.
Bibliography
- [1] Nash AS, Kirkham D, Finnett SL, Bennett D (1981); Primary autoimmune hemolytic anemia in the dog; Vet Rec, 109:150-153
- [2] Sybille A. Miller, Ann E. Hohenhaus, Anne S. Hale (January 15, 2004); Case-control study of blood type, breed, sex, and bacteremia in dogs with immune-mediated hemolytic anemia; JAVMA, 224, No. 2
- [3] Sybille A. Miller, Ann E. Hohenhaus, Anne S. Hale (January 15, 2004); Case-control study of blood type, breed, sex, and bacteremia in dogs with immune-mediated hemolytic anemia; JAVMA, 224, No. 2
[4] Wikipedia Commons URL: https://en.wikipedia.org/wiki/Red_blood_cell - last accessed: 26/04/18
[5] Wikipedia Commons URL: https://en.wikipedia.org/wiki/Spherocytosis & https://en.wikipedia.org/wiki/Red_blood_cell - last accessed: 26/04/18
- [6] Peter C.Kennedy, Nigel Palmer, K.V.F Jubb; Pathology of Domestic Animals; 3rd Edition, 3:136
- [7] Steven L. Stockham, Michael A. Scott (2008); Fundamentals of Veterinary Clinical Pathology; 2nd Edition; Iowa; Blackwell Publishing Professional; Chapter 3, p. 179
- [8] Steven L. Stockham, Michael A. Scott (2008); Fundamentals of Veterinary Clinical Pathology; 2nd Edition; Iowa; Blackwell Publishing Professional; Chapter 3, p. 180
- [9] Steven L. Stockham, Michael A. Scott (2008); Fundamentals of Veterinary Clinical Pathology; 2nd Edition; Iowa; Blackwell Publishing Professional; Chapter 3, p. 180
- [10] Steven L. Stockham, Michael A. Scott (2008); Fundamentals of Veterinary Clinical Pathology; 2nd Edition; Iowa; Blackwell Publishing Professional; Chapter 3, p. 180
- [11] Peter C.Kennedy, Nigel Palmer, K.V.F Jubb; Pathology of Domestic Animals; 3rd Edition, 3:136
- [12] Urs Giger, Derek Duval (1996); Vaccine-Associated Immune-Mediated Hemolytic Anemia in the Dog; J Vet Intern Med, 10:290-295.
- [13] Urs Giger, Derek Duval (1996); Vaccine-Associated Immune-Mediated Hemolytic Anemia in the Dog; J Vet Intern Med, 10:290-295.
- [14] Urs Giger, Derek Duval (1996); Vaccine-Associated Immune-Mediated Hemolytic Anemia in the Dog; J Vet Intern Med, 10:290-295.
- [15] Andrew Mackin, Andrea Balch (2007); Canine Immune-Mediated Hemolytic Anemia: Pathophysiology, Clinical Signs, and Diagnosis; Compendium; 29, No. 4
[16] Wikipedia Commons (A - URL: https://en.wikipedia.org/wiki/Babesia - last accessed:26/04/18 & B - URL: https://en.wikipedia.org/wiki/Leptospira - last accessed: 26/04/18)
[17] M.J. Day (1998); Immune-Mediated Hemolytic Anemia, Veterinary Quarterly, 20:sup1, S39-S40,DOI: 10.1080/01652176.1998.10807400 URL: https://www.tandfonline.com/doi/pdf/10.1080/01652176.1998.10807400 - last accessed: 26/04/18
- [18] Mitchell K, Kruth S (2010); Immune Mediated Hemolytic Anemia and Other Regenerative Anemias; Textbook of Veterinary Internal Medicine, 7th Edition; St. Louis, Saunders Elsevier, p. 761-69
- [19] Abrams-Ogg ACG (2011); Immune-Mediated Hemolytic Anemia and/or Thrombocytopenia in the Dog: Is There Anything More I Can Do?; Western Veterinary Conference
- [20] Kohn B (2007) Immune-Mediated Hemolytic Anemia in Cats; ECVIM-CA Congress; 17th Edition.
[21] M.J. Day (1998); Immune-Mediated Hemolytic Anemia, Veterinary Quarterly, 20:sup1, S39-S40, DOI: 10.1080/01652176.1998.10807400 URL: https://www.tandfonline.com/doi/pdf/10.1080/01652176.1998.10807400 - last accessed: 26/04/18
[22] Wikipedia Commons URL: https://en.wikipedia.org/wiki/Coombs_test - last accessed: 26/04/18
[23] Wolfgang Leibold, Vera Eckmann, Mareike Ottenjann, Christiane Weingart, Barbara Kohn (2006); Primary Immune-Mediated Hemolytic Anemia in 19 Cats: Diagnosis, Therapy, and Outcome (1998–2004); J Vet Intern Med, 20:159–166 URL: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1939-1676.2006.tb02836.x - last accessed: 26/04/18
[24] Wolfgang Leibold, Vera Eckmann, Mareike Ottenjann, Christiane Weingart, Barbara Kohn (2006); Primary Immune-Mediated Hemolytic Anemia in 19 Cats: Diagnosis, Therapy, and Outcome (1998–2004); J Vet Intern Med, 20:159–166 URL: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1939-1676.2006.tb02836.x - last accessed: 26/04/18
- [25] Mitchell K, Kruth S (2010); Immune Mediated Hemolytic Anemia and Other Regenerative Anemias; Textbook of Veterinary Internal Medicine, 7th Edition; St. Louis, Saunders Elsevier, p. 761-69
- [26] Abrams-Ogg ACG (2011); Immune-Mediated Hemolytic Anemia and/or Thrombocytopenia in the Dog: Is There Anything More I Can Do?; Western Veterinary Conference
- [27] Jutkowitz LA (2013); Immune-Mediated Hemolytic Anemia: Current Perspectives on Diagnosis and Treatment; Western Veterinary Conference
- [28] Mitchell K, Kruth S (2010); Immune Mediated Hemolytic Anemia and Other Regenerative Anemias; Textbook of Veterinary Internal Medicine, 7th Edition; St. Louis, Saunders Elsevier, p. 761-69
- [29] Jutkowitz LA (2013); Immune-Mediated Hemolytic Anemia: Current Perspectives on Diagnosis and Treatment; Western Veterinary Conference
- [30] Mitchell K, Kruth S (2010); Immune Mediated Hemolytic Anemia and Other Regenerative Anemias; Textbook of Veterinary Internal Medicine, 7th Edition; St. Louis, Saunders Elsevier, p. 761-69 S.
[31] McCullough (2003); Vet Clin Small Anim 33, 1295-1315; URL: https://www.sciencedirect.com/science/article/pii/S0195561603001232?via%3Dihub – last accessed: 26/04/18