|
Size: 5817
Comment:
|
Size: 6082
Comment:
|
| Deletions are marked like this. | Additions are marked like this. |
| Line 23: | Line 23: |
| It is commonly referred to as autoimmune haemolytic anaemia since the factors that initiated the immune haemolysis are unclear. They have been however, associated with infections, neoplasia and vaccinations, thus may not be autoimmune. | It is commonly referred to as autoimmune haemolytic anaemia since the factors that initiated the immune haemolysis are unclear. They have been however, associated with infections, neoplasia and vaccinations, thus may not be autoimmune. |
| Line 26: | Line 26: |
| Line 28: | Line 27: |
Many drugs have been observed to cause immune thrombocytopenia and these same drugs are linked to Coombs-positive haemolytic anaemia. Some of these drugs are: quinidine, quinine (tonic water), penicillin, insecticides, chloropromazine and dipyrone. [6] More specifically in cats propylthiouracil and in dogs cephalosporins, levamisole and pirimicarb are also highly associated with the above observation. It is usually highly specific with some drugs needing only small doses to cause the disease. [7,8,9,10] Haemolytic anaemia caused by drugs is said to have two types. One type, is induced when an antibody reacts solely with the drug-exposed cells; while the second type, the reaction of the antibody and the red blood cells when the drug is not present. The latter one had it not been for the history of drug exposure and aggravation with retreatment, would have been confused with autoimmune haemolytic anaemia.[11] |
Many drugs have been observed to cause immune thrombocytopenia and these same drugs are linked to Coombs-positive haemolytic anaemia. Some of these drugs are: quinidine, quinine (tonic water), penicillin, insecticides, chloropromazine and dipyrone. [6] More specifically in cats propylthiouracil and in dogs cephalosporins, levamisole and pirimicarb are also highly associated with the above observation. It is usually highly specific with some drugs needing only small doses to cause the disease. [7,8,9,10] Haemolytic anaemia caused by drugs is said to have two types. One type, is induced when an antibody reacts solely with the drug-exposed cells; while the second type, the reaction of the antibody and the red blood cells when the drug is not present. The latter one had it not been for the history of drug exposure and aggravation with retreatment, would have been confused with autoimmune haemolytic anaemia.[11] |
| Line 33: | Line 30: |
| Some sources seem to suggest a correlation between the use of vaccines and the development of Immune Mediated Haemolytic Anaemia. One of these studies conducted by Derek Duval and Urs Giger which tested 58 dogs over a 27 month period and compared to a randomly selected control group comprising of 70 dogs simultaneously with the non-control group. “Fifteen of the dogs (26%) had been vaccinated within 1 month of developing IMHA”. (Fig. 4) The control group saw no increase in the frequency of appearance of the disease. “In the recently vaccinated dogs; combination vaccines from various manufacturers against canine distemper, adenovirus type II, leptospirosis, parainfluenza and parvovirus (DHLPP) were involved in each case”. Two groups were created, one including the “dogs vaccinated within 1 month of developing IMHA and the other which included dogs that developed IMHA more than 1 month after vaccination”. The former group showed a significantly decreased platelet number and “a trend towards increased prevalence of intravascular haemolysis and autoagglutination” when compared to the latter group.[12] | |
| Line 34: | Line 32: |
| Some sources seem to suggest a correlation between the use of vaccines and the development of Immune Mediated Haemolytic Anaemia. One of these studies conducted by Derek Duval and Urs Giger which tested 58 dogs over a 27 month period and compared to a randomly selected control group comprising of 70 dogs simultaneously with the non-control group. “Fifteen of the dogs (26%) had been vaccinated within 1 month of developing IMHA”. (Fig. 4) The control group saw no increase in the frequency of appearance of the disease. “In the recently vaccinated dogs; combination vaccines from various manufacturers against canine distemper, adenovirus type II, leptospirosis, parainfluenza and parvovirus (DHLPP) were involved in each case”. Two groups were created, one including the “dogs vaccinated within 1 month of developing IMHA and the other which included dogs that developed IMHA more than 1 month after vaccination”. The former group showed a significantly decreased platelet number and “a trend towards increased prevalence of intravascular haemolysis and autoagglutination” when compared to the latter group.[12] |
{{attachment:months.png|pop-up text}} < >'''Fig 4.'''< >''A comparison of the appearance of IMHA between the vaccine and non-vaccine group Control group represented by black solid line The majority of the non-control group developed IMHA a month after vaccination [13]'' |
Itt írjon a(z) ImmunhemolyticAnemia-ról/ről
Introduction
Paul Ehrlich in the beginning of the 20th Century proposed the idea of “horror autotoxicus”. This idea suggested that any biological organism is able to endure and recognise its own tissue. However, had the above system become intolerant, an autoimmune disease would be caused.[1] In the following passage the definition of Immune Mediated Haemolytic Anaemia will be discussed in depth. Following, its causes will be detailed using data retrieved from various scientific articles and specialisation books. Moreover, the symptoms presented in the disease will be stated, that one along with the diagnostic methods and tests can use to identify the disease. Lastly, the treatments available and their effectiveness will be mentioned, using proof from the findings collected from the aforementioned sources.
What is Immune Mediated Haemolytic Anaemia
Immune anaemia is caused due to antibody adherence to the cell membrane of a red blood cell which may or may not have a complement fixation. This interaction causes the red blood cell to become spherical which reduces their lifespan by either causing their lysis by the monocytes and phagocytes of the body’s immune system or when the cell membrane forms a complement with the immunoglobulins and an attack complex is created which causes intravascular haemolysis. (Fig. 1)
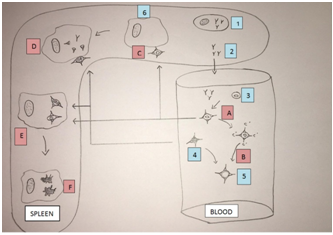 < >Fig 1.< >1 – Lymphocyte, 2 - Free Antibodies, 3 – Erythrocyte, 4 – Spherocyte, 5 – Ghost Erythrocyte, 6 – Macrophage A – Complement reaction, B – Intravascular haemolysis, C – Attachment to macrophage, D – Partial phagocytosis, E – Erythrophagocytosis, F – Extravascular haemolysis.
< >Fig 1.< >1 – Lymphocyte, 2 - Free Antibodies, 3 – Erythrocyte, 4 – Spherocyte, 5 – Ghost Erythrocyte, 6 – Macrophage A – Complement reaction, B – Intravascular haemolysis, C – Attachment to macrophage, D – Partial phagocytosis, E – Erythrophagocytosis, F – Extravascular haemolysis.
Immune mediated haemolytic anaemia is serologically caused by two types of antibodies (or no detectable antibodies): warm-antibodies (usually IgG or IgA), cold-antibodies(usually IgM). Further classification exists when considering the causes, Idiopathic (primary) and Symptomatic (secondary) immune haemolytic anaemias. The above could be even further categorised as being isoimmune, drug-induced, associated with infectious disease or associated with lymphoid or other malignancy.
Idiopathic Immune Haemolytic Anaemia
Most commonly observed in dogs and cats but probably occurs in all species. All breeds of dogs may be affected especially Cocker Spaniels. Other susceptible breeds are Bichon Frise, Miniature Pinschers, Rough-coated Collies, and Finnish Spitz. Sex is also considered to play a role in IMHA development as there are more cases of IMHA in females especially spayed ones. Blood type is assumed to play a role in the susceptibility for the disease, with DEA4 being the most common.[2]
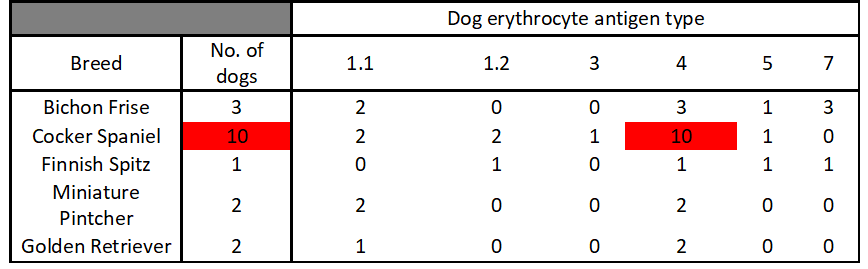 < > Table 1< >The most common blood type among dogs with IMHA was DEA 4 and Cocker Spaniels seem to be the most susceptible to the disease[3]
< > Table 1< >The most common blood type among dogs with IMHA was DEA 4 and Cocker Spaniels seem to be the most susceptible to the disease[3]
When viewed under the microscope anaemia is macrocytic and slightly hypochromic, with a normal haemoglobin concentration. Spherocytosis, leptocytosis and marked anisocytosis are observed. (Fig. 3)
 < >Fig 2.< >Normal Red blood cells (EM) [4]
< >Fig 2.< >Normal Red blood cells (EM) [4] 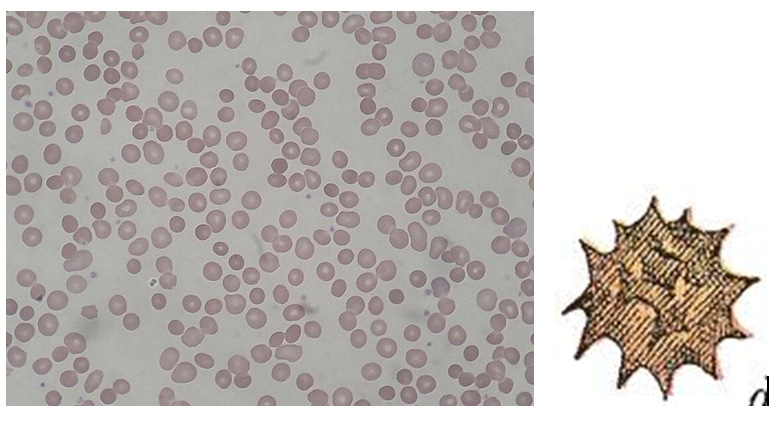 < >Fig 3.< >Spherocytes [5]
< >Fig 3.< >Spherocytes [5]
It is commonly referred to as autoimmune haemolytic anaemia since the factors that initiated the immune haemolysis are unclear. They have been however, associated with infections, neoplasia and vaccinations, thus may not be autoimmune.
Causative Agents
Drug-induced Haemolytic Anaemia
Many drugs have been observed to cause immune thrombocytopenia and these same drugs are linked to Coombs-positive haemolytic anaemia. Some of these drugs are: quinidine, quinine (tonic water), penicillin, insecticides, chloropromazine and dipyrone. [6] More specifically in cats propylthiouracil and in dogs cephalosporins, levamisole and pirimicarb are also highly associated with the above observation. It is usually highly specific with some drugs needing only small doses to cause the disease. [7,8,9,10] Haemolytic anaemia caused by drugs is said to have two types. One type, is induced when an antibody reacts solely with the drug-exposed cells; while the second type, the reaction of the antibody and the red blood cells when the drug is not present. The latter one had it not been for the history of drug exposure and aggravation with retreatment, would have been confused with autoimmune haemolytic anaemia.[11]
Vaccine-induced Haemolytic Anaemia
Some sources seem to suggest a correlation between the use of vaccines and the development of Immune Mediated Haemolytic Anaemia. One of these studies conducted by Derek Duval and Urs Giger which tested 58 dogs over a 27 month period and compared to a randomly selected control group comprising of 70 dogs simultaneously with the non-control group. “Fifteen of the dogs (26%) had been vaccinated within 1 month of developing IMHA”. (Fig. 4) The control group saw no increase in the frequency of appearance of the disease. “In the recently vaccinated dogs; combination vaccines from various manufacturers against canine distemper, adenovirus type II, leptospirosis, parainfluenza and parvovirus (DHLPP) were involved in each case”. Two groups were created, one including the “dogs vaccinated within 1 month of developing IMHA and the other which included dogs that developed IMHA more than 1 month after vaccination”. The former group showed a significantly decreased platelet number and “a trend towards increased prevalence of intravascular haemolysis and autoagglutination” when compared to the latter group.[12]
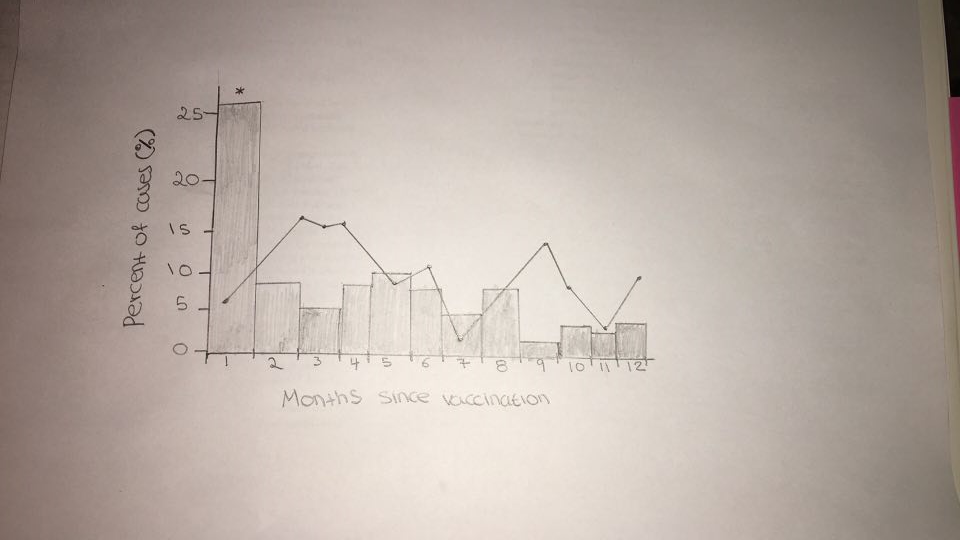 < >Fig 4.< >A comparison of the appearance of IMHA between the vaccine and non-vaccine group Control group represented by black solid line The majority of the non-control group developed IMHA a month after vaccination [13]
< >Fig 4.< >A comparison of the appearance of IMHA between the vaccine and non-vaccine group Control group represented by black solid line The majority of the non-control group developed IMHA a month after vaccination [13]
