Methylamino-alanine as a Potential Trigger for Neurodegenerative Disorders
By: Thita Chanthasukh, Jihun Jung, Damin Lee
Contents
Abstract
Scientific researches predict that by 2040, neurodegenerative diseases will overtake cancer as the second most common cause of death among elders. Neurodegenerative disorders emerge when the neurons of the nervous system lose their functions and die. In turn, it may impair cognition, mobility, sensation, and the coordination of the body. Some of the most notorious neurodegenerative diseases are Alzheimer’s disease, Huntington’s disease, and Parkinson’s disease. The effects and causes of these disorders are so diverse that even though they threaten millions of lives worldwide, many are yet to be discovered and cured.
In this paper, we will be examining one potential risk factor of neurodegenerative disorders, Beta-N-methylamino-L-alanine (BMAA). Although it has been years since discovery, a large part of the potential of BMAA still remains a mystery. BMAA is a nonprotein amino acid first discovered with the high incidence of Amyotrophic Lateral Schlartosis/Parkinsonism Dementia Complex (ALS/PDC) in Guam. It is essential to understand the mechanisms and dangers of BMAA because this neurotoxin can be prevalent in all levels of the trophic level due to biomagnification. As veterinarians, we should understand the consequences of BMAA as it can be incorporated into plant and animal proteins. We will discuss the discovery, effects, and neurological disorders of BMAA. Furthermore, we will conclude the paper by assessing the significance of BMAA in our studies.
The Discovery and Structure of BMAA
|
Figure 1 Structure of Beta-methylamino-L-alanine |
BMAA is a non-protein amino acid, which is produced from blue-green algae (various types of cyanobacteria) in various environments and is known to be concentrated in fish and shellfish. It is thought to be closely related to neurodegenerative diseases such as Amyotrophic Lateral Sclerosis/Parkinsonism Dementia Complex (ALS/PDC). Amyotrophic lateral sclerosis (ALS) is also called Lou Gehrig’s disease. It is a neurodegenerative disease characterized by progressive muscle weakness. This results in a gradual decrease in the number of motor neurons that control the voluntary muscles.
The regions where the disease occurred frequently were Guam, western New Guinea, and the Marianas islands in Japan. The local residents of these regions mainly consumed traditional food ( raw meat, etc.) and tended to have frequent contact with animals. As a result of conducting an epidemiological study on the eating habits of local residents and various environmental factors, the amino acid BMAA was identified as a potent causative agent.
Scholars formed a controversial hypothesis that the exposure to BMAA leads to a variety of neurodegenerative diseases, including AD.
The Effect and Mechanism of BMAA
From a molecular level BMAA has various effects on the molecular level which significantly links to the degeneration of neuron function. Recent studies have shown that BMAA affects many types of receptors including NMDA (N-methyl-D-aspartate) and AMPA (alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid)/Kainate receptor, Glutamate receptor 5 (mGluR5). In addition, the consequence of the malfunction of these receptors may lead to further effects such as induction of oxidative stress and depletion of glutathione.
Glutamate Sensitive Receptor
In order to understand the effects caused by BMAA, basic physiology of NMDA and AMPA /Kainate receptors should be mentioned. As shown in Figure 1, NMDA, AMPA, and Kainate receptors are part of the glutamate-sensitive receptor group, respectively, which also acts as an ion channel. They are named after the agonist that activates them. On the membrane surface of the glutamate-sensitive receptor, five transmembrane domains of these receptors can be found.
|
Figure 2 Three different types of Glutamate sensitive receptors and their basic mechanism |
https://www.frontiersin.org/articles/10.3389/fncel.2015.00091/full |
Glutamate-sensitive ion channel receptors found in the postsynaptic membrane are known to be permeable for sodium potassium and calcium ions which play an important role in the excretory system of the central nervous system.
AMPA-type receptors are sensitive to action potential with lower frequency. Activation of this receptor leads to small sodium ion influx. As a consequence, depolarization is initiated. On the other hand, a higher NMDA-type receptor is more sensitive to action potential with higher frequency. In normal physiological conditions, magnesium ions help the receptor to be in a closed, inactive state. Depolarisation causes disassociation of the magnesium ion. Hence, the receptor becomes activated and opened. Activation of the receptor allows sodium, potassium and calcium to get inside the cell.
The Effect of BMAA on Glutamate-sensitive Receptors
BMAA has the ability to bind NMDA and AMPA/Kainate receptors directly. Figure 2 depicts what happens when BMMA is carbonated. If BMAA is carbonated, the effect of the binding to these receptors is even much stronger as the molecular structures of BMAA now resemble that of glutamate.
|
Figure 3 Once L-BMAA is carbonated, the molecular structure of BMAA is now resembling that of glutamate |
Structurally, most of the NMDA and AMPA type of receptors contain two binding sites for glutamate. Binding of the glutamate to the receptor, together with co-activator glycine and magnesium ions, causes the ion channel to be opened. As mentioned previously, cations including calcium are able to flow through the channel receptor once the receptor is activated. The effect of increasing calcium ion concentration is numerous. Calcium ions are able to act as secondary messengers which leads to the activation of intracellular signaling cascades, induce negative molecular effects such as damaging mitochondria or the increasing production of reactive oxygen species. In relation to the neuron, high calcium ion concentration acts as an antagonist against the function of excitatory amino acids transport 2 (EAAT2). Because EAAT2 is responsible for removing extracellular glutamate and preventing over-excitation of the neurons, overly high concentration of calcium ions, EAAT2 function is inhibited.
In addition to ionotropic glutamate receptors, BMAA also affects metabotropic glutamate receptors (mGluRs). In a cyclic process, BMAA is also able to induce glutamate release via system Xc which is induced through the activation of Glutamate Receptor 5 (mGluR5). According to Liu et al (2010), BMAA inhibits the cystine/ glutamate antiporter system Xc is able to induce the production of reactive oxygen species via glutathione depletion.
The Effect of BMAA on the Neuron
Different types of neurons are affected by BMAA differently. This is mainly due to their sensitivity to AMPA/Kainate receptors and its permeability to calcium ions. This characteristic can be found in motor neurons, more precisely cholinergic neurons. According to Liu et al (2010), even BMAA concentrations as low as 30 mM can lead to the death of cholinergic neurons through AMPA/Kainate receptors.
The NMDA receptor is found in high numbers in the limbic system of the brain, including the amygdala and hypothalamus. These regions of the brain are significantly associated with learning abilities, emotions and vegetative function. Thus, the effect of BMAA toxicity exerted on suggested the possible sensitivity and cause of the neurodegenerative disorders.
The Effect of BMAA on the Protein
In addition to the molecular effect of BMAA on the receptors. According to Cox et al (2013), BMAA has the ability to bind to the amino acid chain of protein and their disassociation is possible through acid hydrolysis. This information suggested that BMAA is able to be released in the body through proteolytic cleavage once the intake happens. The significance lies in the ability for the BMAA to mimic one of the 20 standard amino acids and misoperation into proteins. BMAA is found to be miscoperate and replace serine in human protein. However, the significant effect arises in the case when BMAA replacement happens in the site that is responsible for normal functioning of the protein. In contrast, if BMAA is coerced into a neuronal protein that is unable to degrade these proteins, BMAA-induced accumulation in a particular area of the brain can be observed.
According to Cox et al (2013), both in vitro and in vivo demonstrate the effects induced by BMAA misfolding and protein misfolding. From an in vitro experiment, it is found that BMAA exerted the effect on neuroblastoma cells, causing the apoptosis of these cells similarly to other non-protein amino acids. Furthermore, dysregulation of cellular protein balance and endoplasmic reticulum (ER) stress can also be observed. These effects together contribute to the neurodegeneration and aggregation of BMAA in the motor neuron. As a long term effect, this could lead to chronic toxicity.
Latency effect of BMAA
BMAA does not only cause direct immediate effects on the molecular level. However, long term effects of the incorporation of BMMA can be seen through the association of ALS in migrants to and from Guam. From this, it is possible to draw the connection between the exposure time and the onset effect of BMAA on neural degeneration which demonstrates that BMAA with other environmental effects can also have long term consequences on the neurons. The evidence from studies conducted by Banack et al (2010), summarize the evidence demonstrating the long term effect of BMAA exposure in migrates to and from Guam. As shown in the table, people who migrated from Gaum showed neurodegenerative development up to 34 years later.
Migration |
Number of migrants affected |
Neurodegenerative disorder |
Duration of neurodegenerative development |
From Gaum: Chamoro migrants |
28 |
ALS |
1-34 years after |
|
PDC |
|
|
To Gaum: Filipino migrants |
10 |
ALS |
1-32 years after |
2 |
Parkinsonism-dementia |
13-26 years |
|
7 |
PDC |
5-24 years |
|
Children born in Gaum of Filipino and Chamorro parents |
10 |
ALS |
- |
6 |
PD |
- |
Table 1 Long-term effect of BMAA exposure on migrants to and from Gaum (ALS: Amyotropic lateral sclerosis; PDC: Parkinsonism-Dementia Complex) |
Experiment on the Effect of BMAA
There is plenty of experimental evidence that supports the hypothesis that BMAA is the cause of ALS. In this chapter, we will summarize the experiments that support this hypothesis and those that oppose this hypothesis.
Experiments that Support this Hypothesis
Let's start off with discussing the experiments that support this hypothesis. The hypothesis that BMAA is associated with the pathogenesis of neurodegenerative diseases and behavioral deficits has been substantiated in studies of rodents, monkeys, and insects exposed to BMAA (Karlsson et al, 2009).
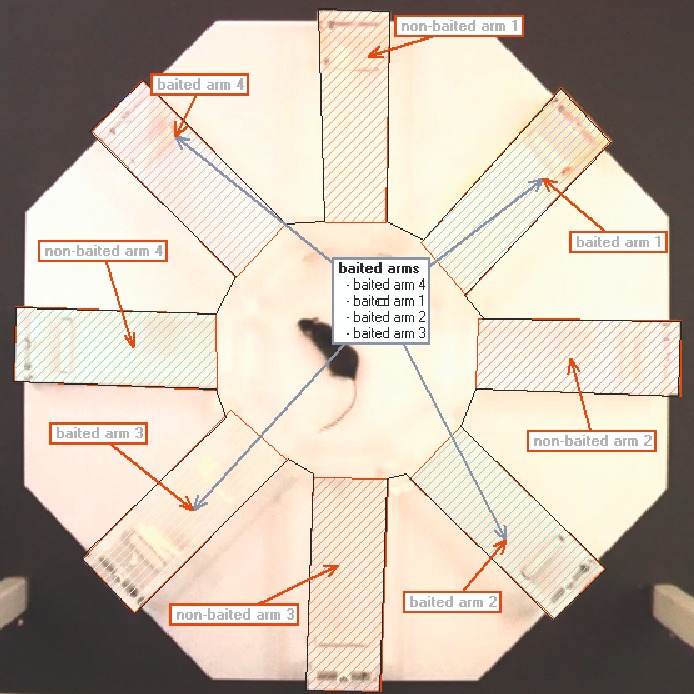
Karlsson and his colleagues experimented the effects of exposure to BMAA on rats. Previous studies experimented by Karlsson and his colleagues revealed that although BMAA could be transduced across the blood-brain barrier in neonatal rats, access to the brain of adult rats is limited. It has since been shown that BMAA is a developmental neurotoxic agent capable of inducing a series of changes, inducing long-term learning and memory deficits (Karson et al, 2009). The spatial learning and memory of adult rodents treated with BMAA during the neonatal period were investigated using the Radial Arm Maze test (RAM test).
|
Figure 4 Radial arm maze test (RAM test) |
The results revealed that BMAA-treated rats exhibited learning disabilities, but no difference in memory. In other words, the most prominent effect of BMAA is spatial learning disability. Exposure to BMAA has been suggested to be associated with the neurodegenerative disease ALS/PDC, and the results of this experiment indicate that BMAA-induced impairment is due to impaired spatial learning and not to changes in motor ability or general activity.
The temporal lobe, including the hippocampus, entorhinal cortex, and the perirhinal cortex, is important for reference memory and working memory (Myhrer, 2003). Studies in adult rats have shown that hippocampus neurons are the most sensitive neurons to BMAA. Karlsson and his colleagues subsequently observed long-term changes in the hippocampus of BMAA treated adult rats using histopathology, immunohistochemistry (IHC), transmission electron microscopy, and proteomics. To summarize only the results of this experiment, no histopathological damage was observed in the hippocampus after 2 weeks of BMAA exposure, whereas distinct pathological changes in the hippocampus were observed 3 month and 6 month after BMAA exposure.
In conclusion, this study revealed that BMAA induces neurodegeneration, astrogliosis, microglial activation, and mineralization. In addition, BMAA-induced hippocampus changes were progressive, and showed increased severity at later time points.
Potential Exposure to BMAA
Humans and animals can be exposed to BMAA in various ways including through dietary or environmental conditions.
BMAA can be exposed to dietary sources consumed by humans and animals fed on cycad seed and its by-product as well as flying foxes. Banack et al (2010) have reported that symbiotic cyanobacteria in the root of plants such as Cycas micronesica is responsible for BMAA production in cycad seed. In addition to plant derived BMAA, Banack et al (2010) also reported that BMAA can is concentrated in crustaceans, mollusks and certain fish feed on benthos. Direct exposure by consumption of these sources and indirect consumption of animals that are fed on cyanobacteria-containing feed explains the accumulation of BMAA in the food chain and in the brain of ALS patients.
Exposure to BMAA is not only limited in adulthood, but also in fetal ages. BMAA is able to indirectly cross from the material exposure into the uterus. This phenomenon is demonstrated in rodents and in postnatal age from contaminated water and food (Karlsson, Lindquist, et al, 2009). The possible exposure and the effect of BMAA during fetal ages is also supported by the findings from Banack et al (2010) (can be found in the Latency effect of BMAA).
Potential Exposure According to Location
Although many studies have pointed out that the cause of neurodegenerative disorders happens in high incidents in Guam, many different parts across the world also share the risk for exposure to BMAA as a consequence of BMAA production of cyanobacterial species in the aquatic and aerosol ecosystem. This indicates that the source of exposure to BMAA is not only confined to dietary reasons.
China
In China, Fai Cai soup is reported to contain BMAA though Nostoc flagelliforme.
Nostoc flagelliforme, referred as “Fai Cai” in Mandarin, is cyanobacterium grown and harvested in the Western part of China. This Fa Cai soup, as shown in Figure 6, is popularly consumed by Chinese people during New Year’s celebration. Nostoc flagelliforme is reported to have variable concentration up to 0.66 µg/g (Banack et al, 2010). However, Nostoc flagelliforme is now banned by the government to decrease the risk of exposure to BMAA in the future.
|
Figure 6 Fa cai soup, which is a common Chinese cuisine |
Peruvia
The risk of exposure of Peruvia people lies in the consumption of Nostoc Immune (Nostocales) or “llullucha” which can be found in the Peruvian highland lake. Nostoc Immune is commonly collected by the native people, eaten directly, added to salad, picante or traded locally and between cities. People believed that it is a source of high nutrition and can function to prevent UV damage via the unusual amino acid they produce. However, BMAA is detected in Nostoc immune marketed in Peruvia while the average BMAA concentration is 10 0.66 µg/g.
United Kingdom Netherland
The presence of BMAA is mainly related to the presence of cyanobacterial blooms in aquatic water systems including both fresh and marine water. This becomes the potential risk for BMAA exposure of both humans and animals via water consumption and activities. Studies shows that from twelve water bodies, BMAA can be detected in a free amino acid form or it can be associated with proteins. The concentration is ranged from undetectable to 276 µg/g and from 6- 48 µg/g, respectively. Similarly, in the Netherlands, BMAA is found to be presence in urban water, more precisely scum materials.
Australia
The presence of cyanobacteria is also reported to be detected in eleven samples taken from freshwater in Eastern Australia. Nineteen single-species cyanobacterial cultures are extracted and analyzed. The laboratory investigation shows that BMAA can be detected in 17 out of 19 isolates. The detection of this toxin leads to further questions and concern of public health and food security in Australia as the water is also being used for agricultural purposes.
Neurodegenerative Disorders
Since the detection of BMAA in Gaum, it has been postulated that BMAA may trigger several neurodegenerative diseases: Amyotrophic Lateral Sclerosis (ALS), Parkinsonism, Alzheimer’s disease, Lewy body disease, and progressive supranuclear palsy (PSP). Generally, neurodegenerative disorders are caused by protein misfolding and aggregation, with variations in the brain where it occurs.
Amyotrophic Lateral Sclerosis (ALS) is a motor neuron disease that progresses rapidly. Around 2.6 people per 100,000 per year in Europe while more than 1.5 per 100,000 per year in the United States with the average year of 47 to 63 are diagnosed with this disease (Odie Lastrawan et al, 2021). ALS can be identified into two types. Sporadic ALS occurs randomly without any clear risk factors. Familial ALS is inherited from a parent and makes up around 5 to 10% of all ALS cases due to the defect in the C9ORF72 gene. The role of BMAA on the etiology of ALS is still an area of uncertainty, but it has been proposed that the misincorporation of BMAA into SOD1, which is a Cu, Zu superoxide dismutase, promotes the onset of ALS. SOD1 is a protein coding gene. Specifically, BMAA replaces each serine in SOD1, structurally modifying SOD1 (Proctor and Dokholyan, 2019). Currently, ALS has no cure with only treatments to relieve symptoms. With the progressive loss of both lower and upper motor neurons, a patient suffers muscle weakness and paralysis and eventually dies.
A similar motor disease that BMAA is thought to induce is Parkinson’s disease (PD), though the disease is not considered fatal as ALS. 0.3% of the general population and 1% of the elders over 60 are estimated to have PD (García-Villa, 2022). PD is characterized by rigidity, tremor, bradykinesia, postural imbalance, or speech impediment (Nunes-Costa et al, 2020). The biomarker of PD is the presence of α-synuclein-containing (ASYN) insoluble fibrous aggregates, termed Lewy bodies (LBs), and the loss of neurons in substantia nigra. Misincorporation of BMAA into ASYN is a possible explanation for protein and misfolding that leads to the symptoms of PD. Alternative mechanisms suggest that BMAA strongly associates with melanin and by selectively inhibit the activity of certain enzymes (Nunes-Costa et al, 2020).
The etiology of notorious Alzheimer’s disease is still unknown today. Alzheimer's disease deteriorates memory and the ability to carry out any task. When the BMAA was discovered from patients suffering from ALS-PDC in Gaum around the 1970s. High amount BMAA was found in the mostportem brains of not only ALS-PDC patients but also in Canadians who died of AD (Holtcamp, 2012). Moreover in Florida, BMAA was detected in the dolphins with Aβ+ plaques, which is a hallmark of AD, supporting the hypothesis that BMAA is indeed associated with Alzheimer's disease (Davis et al, 2019). Although it was previously thought that BMAA can be one of the causations for Alzheimer's disease (AD), research from 2016 contests the accumulation of BMAA in the brain of patients diagnosed with AD. Brain samples of 20 AD patients and 20 AD control patients were analyzed for the presence of BMAA. However, it was found that none of this neurotoxin, either free or protein-bound, was detected in AD positive or negative patients (Meneely, 2016). In conclusion, this robust finding contributes to the controversy of BMAA’s role in AD up to date.
Conclusion
Lastly, we discussed the general information of Beta-N-methylamino-L-alanine (BMAA) and how it influences and aggregates neurodegenerative disorders. As acknowledged multiple times in the essay, extensive research is still required to cease the controversies existing regarding the presence of BMAA in certain diseases, like Alzheimer's disease. BMAA is also relevant to our studies since it serves as a great example of the trigger for glutamate receptors, which we learned about.
Reference
Davis DA, Mondo K, Stern E, Annor AK, Murch SJ, Coyne TM, et al. (2019): Cyanobacterial neurotoxin BMAA and brain pathology in stranded dolphins. PLoS ONE 14: (3) e0213346
García-Villa M., Leal-Cantú R., Madrigal-Salas R. G., Rodríguez-Leyva I., Quintana-Díaz M. A., and Gonzalez-García C. L. (2022): Parkinson’s disease in the state of Michoacan, evolution, and treatment. Revista Mexicana de Neurociencia 23: (1) 14–21
Holtcamp, W. (2012): The Emerging Science of BMAA: Do Cyanobacteria Contribute to Neurodegenerative Disease?. Environmental Health Perspectives 120: (3) A110–A116
Meneely, J., Chevallier, O., Graham, S. et al. (2016): β-methylamino-L-alanine (BMAA) is not found in the brains of patients with confirmed Alzheimer’s disease. Scientific Reports 6: 36363
Nunes-Costa D, Magalhães JD, G-Fernandes M, Cardoso SM, Empadinhas N (2020): Microbial BMAA and the Pathway for Parkinson’s Disease Neurodegeneration. Frontiers in Aging Neuroscience 12: 1663-4365
Odie Lastrawan I. M., Arimbawa K., & Pratiwi M. D. (2021): Clinical characteristics and neurophysiology features of amyotrophic lateral sclerosis patients at Sanglah Hospital Denpasar. Romanian Journal of Neurology, 20: (3) 330–334
Proctor EA, Mowrey DD, Dokholyan NV (2019): β-Methylamino-L-alanine substitution of serine in SOD1 suggests a direct role in ALS etiology. PLoS Comput Biol 15: (7) e1007225
Oskar Karlsson, Erika Roman, Eva B. Brittebo (2009): Long-term Cognitive Impairments in Adult Rats Treated Neonatally with β-N-Methylamino-L-Alanine. Toxicological Sciences 112: (1) 185–195
Karlsson, O., Berg, A. L., Hanrieder, J., Arnerup, G., Lindström, A. K., & Brittebo, E. B. (2015): Intracellular fibril formation, calcification, and enrichment of chaperones, cytoskeletal, and intermediate filament proteins in the adult hippocampus CA1 following neonatal exposure to the nonprotein amino acid BMAA. Archives of toxicology, 89: (3) 423–436
Banack SA, Caller TA, Stommel EW (2010): The Cyanobacteria Derived Toxin Beta-N-Methylamino-L-Alanine and Amyotrophic Lateral Sclerosis. Toxins: (2) 2837-2850
Liu XQ, Rush T, Ciske J, Lobner D (2010): Selective death of cholinergic neurons induced by beta-methylamino-L-alanine. Neuro-report: (21) 55-58
Silva DF, Candeias E, Esteves AR, et al. (2020): Microbial BMAA elicits mitochondrial dysfunction, innate immunity activation, an Alzheimer’s disease features in cortical neurons. Journal of Neuroinflammation: (17) 1-18
Takahashi K, Foster JB, Lin CLG. Glutamate transporter EAAT2 (2015): regulation, function, and potential as a therapeutic target for neurological and psychiatric disease. Cellular and Molecular Life Science: (72) 3489-2506
Vyas KJ, Weiss JH (2009): BMAA – an unusual cyanobacterial neurotoxin. Amyotrophic lateral sclerosis : official publication of the World Federation of Neurology Research Group on Motor Neuron Disease: (10) 1-6
Kritis AA, Stamoula EG, Paniskaki K, Vavilis TD (2015): Researching glutamate – induced toxicity in different cell lines: a comparative/collective analysis/study. Frontiers in Cellular Neuroscience: (9) 1-12
Durves D, Augustine GJ, Fitzpatrick D, et al. (2021): Glutamate receptors. Neuroscience: (2)
Cheng J, Tang JC, Pan MX, Chen SF, Zhao D, et al. (2020): L-lysine confers neuroprotection by suppressing inflammatory response via miroRNA-575/PTEN signaling after mouse intracerebral hemorrhage injury. Experimental Neurology: (327)
Dunlop RA, Cox PA, Banack SA, Rodgers KJ (2013): The non-protein amino acid BMAA is misincorporated into human proteins in the place of L-serine causing protein misfolding and aggregation. PLoS One 8: (9) 1-6
Roney BR, Ranhui L, Banack SA, Murch S, Honegger R, Cox PA (2009): Consumption of fa cai Nostoc soup: a potential for BMAA exposure from Nostoc cyanobacteria in China?. Amyotroph Lateral Scler 2009: (10) 44-49
Johnson HE, King SR, Banack SA, Webster C, Callanaupa WJ, Cox PA (2008): Cyanobacteria (Nostoc commune) used as a dietary item in the Peruvian highlands produce the neurotoxic amino acid BMAA. J Ethnopharmacol 118: (1) 159-165
Violi JP, itrovic SM, COlville A, Main BJ, Rodgers KJ (2019): Prevalence of B-methylamino-L-alanine (BMAA and its isomers in freshwater cyanobacteria isolated from western Australia. Ecotoxicol Environ Safety: (172) 72-81
Main BJ, Bowling LC, Padula MP, Bishop DP, Mitrovic SM, Guilleme GJ, Rodgers KJ (2018): Detection of the suspected neurotoxin B-methylamino-l-alanine (BMAA) in cyanobacterial blooms from multiple water bodies in Eastern Australia. Harmful Algae: (74) 10-18
Lobner, D., Piana, P. M., Salous, A. K., & Peoples, R. W. (2007): Beta-N-methylamino-L-alanine enhances neurotoxicity through multiple mechanisms. Neurobiology of disease 25: (2) 360–366
Karlsson, O., Berg, A. L., Hanrieder, J., Arnerup, G., Lindström, A. K., & Brittebo, E. B. (2015): Intracellular fibril formation, calcification, and enrichment of chaperones, cytoskeletal, and intermediate filament proteins in the adult hippocampus CA1 following neonatal exposure to the nonprotein amino acid BMAA. Archives of toxicology 89: (3) 423–436
Proctor, E. A., Mowrey, D. D., & Dokholyan, N. V. (2019): β-Methylamino-L-alanine substitution of serine in SOD1 suggests a direct role in ALS etiology. PLoS computational biology 15: (7) e1007225