Multiple Organ Failure as a Potential Protective Endocrine-Mediated Response to Chronic Stress
Homeostasis is the coordinated system of physiological and biochemical processes which regulate and maintain most of the steady states in the organism, attempting to keep the internal conditions relatively constant, for example: pH, internal temperature, etc; in a state of equilibrium. This concept is essential to the understanding of stress.
In everyday life, there are numerous factors that recurrently disrupt homeostasis, such as, environmental factors or internal and external stimuli. This coordinated system then works to keep the organism in an incessant flux around particular variables that could be considered optimal conditions for it to live and survive. Stimuli that cause deviation relatively far from the optimal equilibrium, are termed as stressors. These could include: physical stimuli such as pain; exposure to pathogens such as bacteria or viruses; nutritional deficiencies; emotional or psychic trauma. This deviation from homeostasis caused by stressors, and the organism’s specific response to them, involving a number of processes which strive to restore normal body conditions, can be perceived as Stress. The burden of chronic stress and accompanying changes in personal behaviours is called Allostatic overload (Del Giudice et al., 2011; McEwen, 2008).
As per the event, specific responses to stress is conducted by Sympathetic nervous system (SNS) activation which leads to the Cannon’s reaction, or so-called Fight-or-Flight response. This state cannot be maintained for extended periods of time as it could be detrimental to the physical and mental health of the organism. The Parasympathetic nervous system (PNS) seeks to returns the conditions to the more optimal range. This restoration consumes a lot of energy and resources, putting a lot of strain on the body, but seeks to focus it to repress the immediate problem. One such process to overcome chronic stress is multiple organ failure caused by the organism's own system (McEwen, 2008).
Contents
Stress Response
The system that carries out the stress response lies in the endocrine, and central and peripheral nervous systems. The primary effectors for the stress response are: Corticotropin-releasing hormone (CRH); Vasopressin (ADH); Proopiomelanocortin-derived (POMC) peptides such as α-melanocyte-stimulating hormone and β-endorphin; the glucocorticoids; and the catecholamines, norepinephrine and epinephrine are all principals of the stress system (Keenen et al., 2007).
|
Autonomic Nervous System
The function of the Parasympathetic Nervous System (PNS) is to promote vegetative functions, as well as decrease physiological arousal, via the cholinergic fibres that innervate organs by the parasympathetic branches of the autonomic system. However, in the digestive tract, this does not include fibres that release adenosine triphosphate (Lovallo and Sollers, 2007).
The equilibrium between the PNS and SNS, with the PNS tonic activation, ensures proper regulation of Sympathetic-induced arousal. This mechanism is carried out by self-regulation, rest and collective engagement. The deactivation of the PNS would result in the termination of the counterbalance of the sympathetic activation, leading to the full release of the SNS effect. Withdrawal of Parasympathetic activity causes an immediate increase of arousal and restores awareness in an instance encountering an unexpected event. If the withdrawal of parasympathetic activity is inadequate, the SNS can exhibit a second layer of response. If PNS effect on SNS does not suffice in coping with a stressful situation, the Fight-or-Flight response will be mediated by the Locus Coeruleus (LC). SNS activation, can be conducted through two pathways: Direct noradrenergic innervation of the visceral organs (fast); or a Hormonal pathway through innervation of the adrenal medulla (slow) (the sympathetic-adrenal-medullary pathway; (Goldstein and Kopin, 2008; Gunnar and Vazquez, 2006). This facilitates the release of catecholamines by the adrenal medulla. These lead to an increased heart rate, respiratory rate, vascular perfusion of skeletal muscle and glucose released into the bloodstream, while simultaneously decreasing the functioning of less important body processes to increase immediate energy availability. The epinephrine- norepinephrine balance can be attributed with specific behavioural reactions to the stressors, with “high NE/E ratios associated with proactivity and dominance and low ratios associated with fear and anxiety" (Korte et al., 2005; Netter, 1983, 1987)
HypothalamoPituatary Adrenal Axis
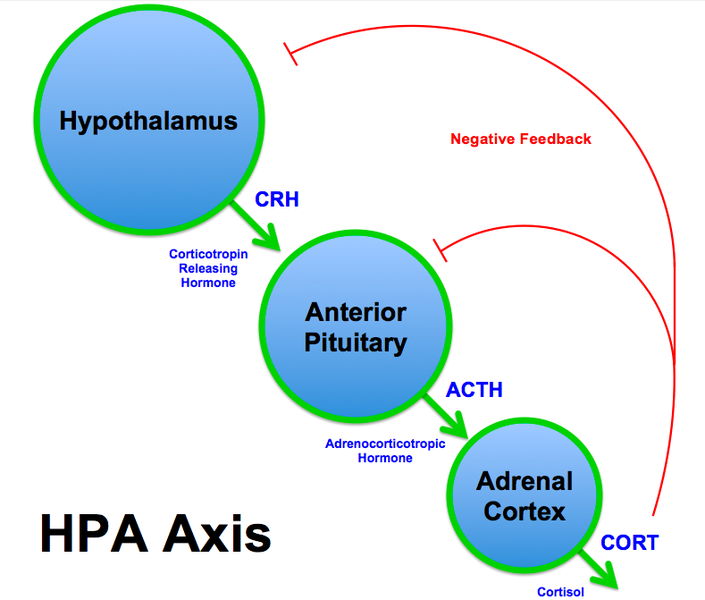
The HypothalamoPituatary Adrenal (HPA) axis, the schematics of which are shown in Figure 1, is an intricate set of interactions among three endocrine glands, being the hypothalamus, pituitary gland, and adrenal glands. These interactions constitute a major part of the neuroendocrine system responsible for the response to stress, as well numerous body processes that affect the organism both physically and mentally. These include regulation of energy stores and their expenditure, sexuality, digestion, the immune system as well as emotions.
Fundamentally, the HPA axis responds to stressors through the release of cortisol in a long term, delayed process. The Hypothalamus secretes Corticotropin Releasing Hormone (CRH) and Vasopressin (ADH) into the portal circulation of the pituitary gland by neurons of the Paraventricular nucleus (PVN). These elicit the release of Pro-Opiomelanocortin polypeptide (POMC) from the Adenohypophysis, which can then be cleaved into several hormones. This includes Adrenocotricotropic hormone (ACTH). ACTH, through systemic circulation, arrives at the cortex of the Adrenal gland and stimulates the release of Cortisol. The main task of Cortsiol is to redistribute and allocate energy to the organs and tissues that require it the most during a stress response. CRH itself, also takes part in the physio- and psychological response to stressors (Del Giudice et al., 2011; Keenen et al., 2007).
General Adaptation Syndrome
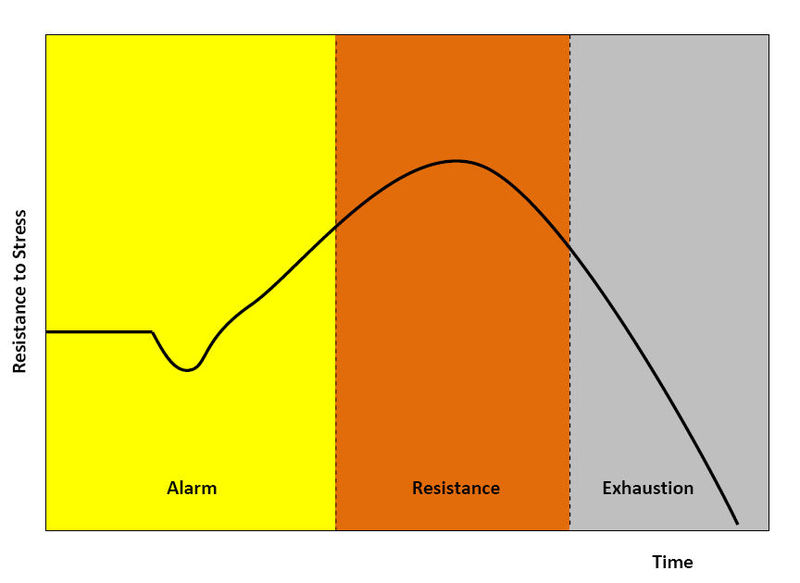
General Adaptation Syndrome (GAS) outlines an organism’s stress response. It is mediated by the interactions of the HPA axis, and, as shown in Figure 2, can be distinguished into separate phases (Taylor et al., 2012):
Initial phase
|
The primary factor in the development of stress is the immediate release of ACTH. It acts on the adrenal glands and stimulates the secretion of catecholamines i.e., Epinephrine, Norepinephrine, and Dopamine, which in turn cause an increase in blood pressure, and heart and respiratory rates. This can be referred to as Cannon's alarm response, or the Fight-or-Flight theory, and is under the influence of the Sympathetic nervous system (Taylor et al., 2012)
Phase of Resistance
In this phase, Catecholamine levels decline, however, ACTH levels still remain high resulting in the production of Glucocorticoids by the adrenal cortex, which play an important role in providing the optimal conditions for the body's ability to resist stress. They decrease the functioning of relatively less important processes, not required for immediate survival, such as functioning of the digestive tract, energy storing processes, immune system and insulin secretion, even though hyperglycemia occurs due to excessive gluconeogenesis. Fat oxidation becomes the main energy source. Carbohydrate synthesis is made possible by the utilisation of amino acids, that are released during the breakdown of muscle. Due to these factors, the organism is able to withstand the effects of stress for a long time, however, over exposure to these factors over a prolonged perioid could result in one of the following two phases (Taylor et al., 2012).
Phase of Exhaustion
Persistence of stress would result in depletion of available energy reserves, which would lead to collapse and, in due course, death of the animal (Taylor et al., 2012).
Phase of Adaptive Disorders
Adaptive disorders, not shown in Figure 2, follow the resistance phase, and aim to redirect the body's energy and focus, at the expense of another organ's supply and functioning, to systems that would allow it to combat the stress. For example arthritis, chronic hypertension, ulcers or multiple organ failure (Singer et al., 2004; Taylor et al. 2012).
Multiple Organ Failure
|
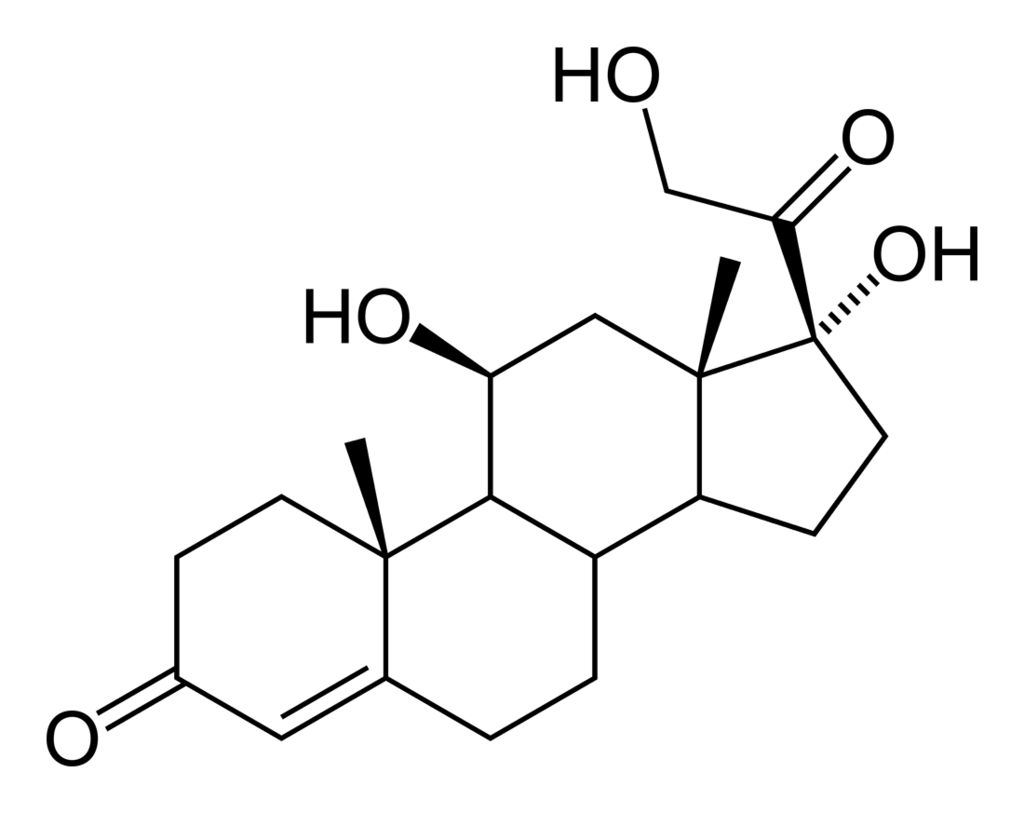
Sepsis and other critical illnesses lead to a biphasic inflammatory, immune, hormonal, and metabolic response. A pronounced increase in the secretion of the stress hormones with an associated increase in mitochondrial and metabolic activity, marks the acute phase. As a result of the changes in the endocrine profile and intense inflammation, energy production, metabolic rate, and normal cellular processes decrease drastically, thereby resulting in Multiple Organ Dysfunction (failure). The decline in organ function is triggered by a decrease in mitochondrial activity and oxidative phosphorylation, leading to reduced cellular metabolism. This effect on mitochondria might be the consequence of acute-phase changes in hormones and inflammatory mediators. Cortisol, Figure 3, for example, is responsible for the redirection of energy sources away from the failing organs, and towards body process that require it more, so that the stress could be overcome (Singer et al., 2004).
Though stress is often considered to have a negative effect on the body, it can play a crucial and positively role ensuring adequate performance and wellbeing of the animal, furthermore, ensure social interactions. Failure to exhibit the appropriate stress responses could lead to various physical and mental impediments. For example, decreased growth and development, and immune, endocrine and metabolic disorders could be attributed to this. However, the extent of vulnerability of an individual organism to these impediments is related to its own genetic coding (Charmandari et al., 2005).
The observed organ failure has been postulated to be a potentially protective mechanism to overcome stress. The reason for this being that the reduced cellular metabolism could prospectively heighten their chances of their survival and thus the overall survival of the organ, when exposed to profuse abuse. Singer et al. (2004) propose that "multiple organ failure induced by critical illness is primarily a functional, rather than structural, abnormality". It could be hypothesised that instead of being a 'failure' in the broad sense, it could possibly be protective, reactive mechanism of the body (Singer et al., 2004)
Benefits of Future Research
Further research relating to the processes and systematics of stress-related organ dysfunction could be greatly beneficial for our understanding. The postulation by Singer et al. (2004) that multiple organ failure could be an organism’s protective mechanism was an important step towards our understanding of the physiology behind the process. However, additional research would help attain a better grasp on the subject. In the study by McEwen (2008), it was identified that certain regions of the brain, like the hippocampus, prefrontal cortex and amygdala, showed response to chronic stress, in the form of morphological and chemical changes. It was seen that if the chronic stress lasted for weeks, the changes were still largely reversible, however, there is still no clarity as to whether prolonged exposure, of many months, would have any irreversible effects. A study such as this is one of many that could potentially help further progress in this field.
References
Journal Atricles
Gunnar MR & Vazquez D (2006). Low cortisol and a flattening of expected daytime rhythm: potential indices of risk in human development. Developmental Psychopathology, 13(3), 515-538.
Lovallo WR, Sollers JJ. (2007). Autonomic nervous system. Encyclopedia of stress, 2, 282–289.
Netter P(1987). Psychological aspects of catecholamine response patterns to pain and mental stress in essential hypertensive patients and controls, 3, 727–742.
Other References
Taylor, Shelley, and Sirois, Fuschia. (2012). Health Psychology 2nd Canadian Edition
Figures
Figure 1. Response to Stress, Wikimedia Commmons