Impacts of Sleep Loss and Stress
Introduction
Stress is the body’s response towards daily life, in terms of noxious stimuli. There is a correlation between the severity of the stress response, due stimulus intensity, with the length of sleep. The process of sleep is a function of the body by which several hours are used to act on the regulatory systems of the internal environment; balancing out hormone production and breakdown and maintaining a healthy immune system. The average human can survive several days of sleeplessness but the reduction of sleep periods can result in diminishing heath and functioning. (Derrer, 2014)
This essay attempts to look at the various causes and subsequent outcomes of sleep deprivation.
Contents
Types and Causes
Sleep deprivation occurs when sleep is insufficient to support typical body functions, either as a result of an inefficient sleep period (quantity) or a disturbance in sleeping pattern (quality). It can be either acute; no sleep/ a reduction in total sleep time or it can be chronic; where an individual consistent sleep levels are less than that required for optimal functioning. (Orzeł-gryglewska, 2010)
General sleep reduction- caused by daily sleep time reduction below level of optimum needs, absence of a single nights sleep or a shift in sleep in relation to circadian pattern. Examples include social eccentrics (partying), late shifts of work and general factors from contemporary lifestyle.
Considerable sleep reduction- caused by lengthened insomnia over several days or complete sleep deprivation. Examples would include, experimental conditions or possible extreme situations, i.e., torture.
Sleep reduction due to pathological processes- caused by depression, anxiety disorders, addiction/ chemical substance abuse, somatic/painful diseases or sleep disorders, i.e., subjective, idiopathic and psychophysiological insomnia. The sleep in these disorders is of low quality, delayed and shortened, and some genetic factors or enhanced by old age and chronic stress or traumatic experiences. (Orzeł-gryglewska, 2010)
These different types of sleep deprivation can roll on to have an effect on the different systems inside the body as well as cognitive and general body function. Discussed below in more detail.
Effects
Physiological
Cardiovascular Effects
Sleep deprivation, like smoking is now noted as one of the main causes of developing heart disease. The possible reasoning for this, is that a decrease in sleep results in increased blood pressure, and sympathetic overactivity; known precursors for developing coronary heart disease. Sleep deprivation may be caused by sleep apnea which also can be a factor in developing heart disease (Quan, 2009).
Increased Blood Pressure and Sympathetic Overactivity
Studies performed on healthy individuals, showed a significantly larger systolic blood pressure following one night of sleep deprivation, compared with non-sleep deprived individuals. One experiment examined the theory of this systolic increase being linked with stress induced reaction. They created a control, in which subjects were not exposed to any form of stressful situation, following sleep deprivation (Franzen et al, 2011). The same increase in systolic pressure was observed. Therefore highlighting a clear link between sleep deprivation and increased blood pressure. Without adequate rest periods sympathetic overactivity results. Normally, heart rate is controlled by a balance between the parasympathetic nervous system and the sympathetic nervous system. The parasympathetic innervation via the vagus nerve causes a decrease in heart rate by having a direct depressor effect on the sympathetic nervous system. Sympathetic nervous system elevates the heart rate by causing an muscarinic Acetylcholine activated elevation in cAMP, which causes elevation in heart rate Sympathetic overactivity, leads to inadequate depression via the parasympathetic vagus nerve and the heart rate remains increased as a result. Figure 1.1 highlights the parasympathetic suppressant effect on the heart rate. Long term sympathetic over-excitability results in hypertension, which leads to cardiovascular disease (Ayas et al, 2003).
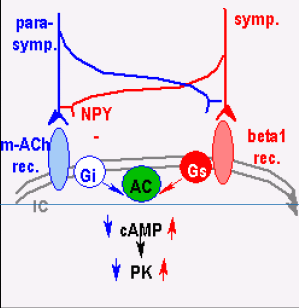
Fig 1. Sympathetic and Parasympathetic control of Heart Rate. This shoes the effect of the parasympathetic and sympathetic system on heart rate. Elevation in sympathetic activity counteracts the depressor effect of the parasympathetic system thus, resulting in increased heart rate (Barta, 2014).
Sleep Apnea
Obstructive sleep apnea, a cause of sleep deprivation is also linked in patients developing heart disease. During sleep, there is a natural loss in muscular tone including muscles which encapsulate the pharynx. The pharynx and upper airspace is composed of muscles and soft tissue. With this loss of tone, in some patients, it can cause the airway to “collapse” , thus obstructing the airway. This airway occlusion results in decreased intrathoracic pressure, which therefore leads to an increased afterload of venous return, causing right ventricular distention and the interventricular septum to shift. Combination of these events causes a decrease in left ventricular stroke volume which decreases the cardiac output significantly (Latina et al, 2013).
Cardiac output decrease causes pulmonary stretch receptors to activate the sympathetic nervous system. Also hypoxia and hypercapnia caused by airway obstruction, stimulate peripheral and central chemoreceptors, also resulting in sympathetic activation. This sympathetic activation increases blood pressure by causing vasoconstriction in an effort to overcome these adverse effects. In a patient suffering with obstructive sleep apnea, they can encounter these surges hundreds of times per night, resulting in huge fluctuations in heart rate and blood pressure. In the long term, hypertension results, which can then lead to heart disease.
Obesity
Chronic sleep loss has a huge impact on neuroendocrine function and glucose metabolism, both which are underlying risk factors in obesity development. Sleep deprivation causes alterations in both metabolic and endocrine mechanisms. Such as; Decrease glucose tolerance and insulin sensitivity, Increased cortisol concentrations in the evening, Increased ghrelin concentration, Decreased leptin levels.
These factors result in increased appetite and therefore at a higher risk of developing obesity. The brain, requires a constant glucose supply, even when food intake that provides the glucose does not occur. During sleep, this supply must be maintained. Studies have found that tolerance to glucose and insulin differed following sleep deprivation. Lack of sleep resulted in an increase in blood glucose level, lower insulin response and a slower glucose tolerance. Prolonged sleep deprivation may result in insulin resistance and development of type 2 diabetes by its effect on mechanisms of blood glucose level regulation. Or it may also indirectly result in type 2 diabetes by causing an increased appetite (Morsell et al, 2010). Ghrelin is a stomach-derived peptide which has a primary role in energy balance by increasing food intake and bodyweight along with reduction in body fat utilization. Ghrelin has been identified as a sleep inducing factor by inducing slow-wave sleep and night time release of growth hormone, adrenocorticotropic hormone (ACTH) and cortisol. Ghrelin concentration was seen to increase individuals in the morning following sleep deprivation (Leproult and Cauter, 2010; Russel et al, 2012). Leptin, an adipocyte derived hormone is involved in energy metabolism and fat utilization. Under normal circumstances, leptin is involved with reducing feed intake. Leptin is involved in a insulin containing reflex mechanism in which, an increase in insulin following feed intake causes an increase in leptin. Leptin levels decrease following a night a sleep deprivation, which causes an increase in feed intake Sleep derived increase in ghrelin levels and decreased insulin result in a remarkable increase in appetite as there is a strong correlation between increased ghrelin-to-leptin ratio and increased appetite (Sharad et al, 2004).
Orexin Neurons
Orexin-containing neurons of the lateral hypothalamus have a crucial role in sleep and are involved in the regulation of energy homeostasis. Their site of action is in the same area as the leptin and ghrelin hormone response region, and they partake in its synthesis and secretion. As mentioned above leptin and ghrelin are the main hormones involved in feed intake. Decrease in leptin and increase in ghrelin, following sleep deprivation, suppress the activity of orexin neurons which also leads to increase in feed intake, but orexin also affects energy expenditure (Leproult and Cauter, 2010). Decreased orexin activity, causes a decrease in energy expenditure, causing an increased body mass index (BMI) from increased fat storage and less fat store energy utilisation.
Growth Hormone
The release of growth hormone from the adenohypophysis is stimulated by hypothalamic derived Growth Hormone Releasing Factor (GHRF) and is inhibited by somatostatin (growth hormone inhibiting factor, GHIF). GHRF is also involved with inducing slow-wave-sleep, but its release is highly dependent upon the duration and quality of sleep. GH has a circadian rhythm, meaning the majority of GH pulses occur shortly after the onset of sleep (figure 2). GH exerts its effects on various organs and tissues, while also stimulating release of further hormones in the liver. It is referred to as an anabolic hormone, as its involved in increasing amino acid uptake, protein synthesis which leads to increased growth. A decline in sleep duration and quality was found to decrease GH availability in the body (Redwine et al, 2000).
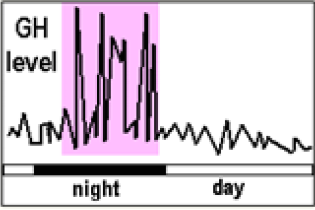
Fig 2. The Circadian Pattern of Growth Hormone. Diurnal levels are minimal in comparison with nocturnal levels. Sleep deprivation results in decreased growth hormone levels, affecting the circadian rhythm of growth hormone (Barta, 2014).
A decrease in sleep, leads to a decrease release in growth hormone, which has been linked with dwarfism in younger animals and people. A lack of GH is also linked with increased weight gain, as GH is involved lipolysis of adipose tissue, to mobilize fatty deposits for energy need during anabolic processes. It also has a insulin suppressant effect by decreasing insulin-dependent uptake of glucose by adipose tissues (Maurovich and Sonka, 2008). GH stimulates liver synthesis of Insulin-like growth factor (IGF-I), involved in bone growth and metabolism.
The Corticotropin Axis
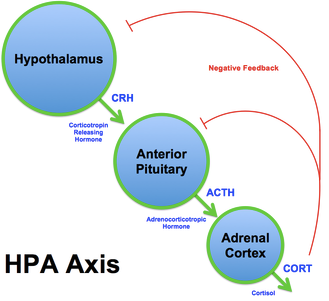
Fig 3. The Corticotropin Axis (Wikipedia, 2014).
The corticotropin axis, involves Adrenocorticotropic Hormone (ACTH) released from the adenohypophysis in response to corticotropin releasing hormone (CRH) from the hypothalamus. ACTH then causes the adrenal cortex to release cortisol, and this collectively is referred to as the corticotropin axis (Figure 3). Sleep deprivation is associated with alterations in the 24 hour cortisol release pattern, with elevated levels in the evening and the morning. As opposed to the regular diurnal rhythm of cortisol elevation on occurring during the evening (Redwine et al, 2000;Maurovich and Sonka, 2008). Cortisol is involved in gluconeogenesis, which is the use of glycerol, lactic acid and amino acids in the liver to form glucose. It also has an important role in glycogenolysis which also results in an increased blood glucose concentration.
Thyrotropin (TSH)
TSH normally shows decreased diurnal levels which then rapidly increase during the evening and reaching the maximum levels at night at the start of sleep onset. Sleep deprivation results in a significant decrease in this night peak of TSH and the overall 24hr concentration of TSH shows a decrease as a result. TSH stimulates the thyroid gland to release Thyroxine (T4), which is later converted into Triiodothyronine (T3). T3 is one of the main hormones involved in metabolism; including protein, lipid and carbohydrate metabolism. It increases lipolysis, gluconeogenesis, and protein break down all of which are involved with decreasing BMI (Leproult and Cauter, 2010).
Immunological
Sleep deprivation has a variety of significant effects, as factor of physiological stress on pathological inflammatory responses via interactions with neuroendocrine functioning and the immune system, mainly resulting in the depression of the immune system and theres a strong correlation between infectious disease and prolonged sleep time as a symptom of healing. Sleep allows for the increase in lymphocyte activity. (Besedovsky, 2011)Deprivation mainly results in lowered resistance to infections but doesn’t result in fever or an inflammation. In sleep deprived animals infections of tissues and lymph are induced by self intestinal flora and this can only be made possible via immunological suppression. Inflammatory mediators such as IL-6/1 and TNF, inflammatory markers produced by active lymphocytes are particularly affected by sleep deprivation and restoration, as sleep is the indication of the circadian rhythm. Generally in young adults, experimentally, the secretion of ILs tends to depend on duration/quality of sleep, by which acute sleep deprivation causes an increase in daytime IL-6 production which then results in drowsiness and fatigue effectively reducing neurocognitive performance and fatigue. TNF secretion is also shifted from night time to daytime secretion as sleep tends to increase the redistribution of T cells to lymph nodes, aggregating the decreased mental/cognitive performance and daytime fatigue. (Orzeł-gryglewska, 2010) This then further perpetuates the cycle of insomnia making it difficult for insomniacs to fall asleep. Furthermore other studies have linked a drop in cytokine production levels in response to acute sleep deprivation as an immediate stress response. Reduction on cytokine levels decreases the promotion of antigen presenting and Th cells, and further studies show that sleep after a virological vaccination resulted in a persistent increase of antigen specific cells, collecting the two suggests that sleep has a specific role in immunological memory, all of which is influenced by hormonal levels during slow wave sleep.
Effect on brain functioning
Experiments were carried out on a patient with 72hours of sleep deprivation with brain metabolic rate being observed in the process, generally no significant interhemispheric difference where detected. Decrease in activity varied from 6-15% in various areas of the brain. Tends to be hypometabolism of glucose in the hypothalamus as well as lobes of the Telencephalon. (Orzeł-gryglewska, 2010) In general activity of the prefrontal and parietal cortex tends to decrease in some cases, like arithmetic problem serving whilst in memory testing there tended to be higher activity in the right hemisphere, mainly because the need for verbal communication precedes that of problem solving. After sleep deprivation, decreased P3 amplitude in frontal and apical skull regions was noted. Prefrontal functions tend to be relocated to different areas of the brain and so with restoration of sleep these areas can recover quickly, proven with a 30 minute sleep rebound by which the delta waves of EEG recorded from the prefrontal area showed a significant greater power than other areas. (Orzeł-gryglewska, 2010) (Aigboje,2014) The EEG provides an more lateral way to assess functioning, by recording delta and theta waves of various brain regions. During initial stages of SD the wave readings increase, and standing upright helps maintain such levels regardless of length of deprivation. Alpha waves weren’t present until the 20th hour. Functional clusters of EEG can also be assessed. (Orzeł-gryglewska, 2010)This is where a group of brain areas cooperate with one another more closely than other areas. In rested subjects, the symmetrical dominant cluster in the EEG signal included the F7, F8, C3 and C4 locations and after 24 hours of wakefulness, the cluster comprised the C4, F8, F3, F4 and O1 locations, which indicates that after sleep deprivation, the F3/F4 and O1 locations are functionally associated with C4 and F8. The findings show that the locations of the functional cluster has changed, moving predominantly to the right hemisphere, giving insight into the functioning of the brain in a sleep deprived status. (Orzeł-gryglewska, 2010) (NCBI (National center for Biotechnology information), 2008)
Psychological
Depression
Depression is a very common symptom and can affect day-to-day life activities. One of the main causes is a low mood and low self-esteem. Problems like losing a job or failing an exam can cause depression (Dr Kenny, 2014)
Obstructive sleep apnea (OSA) is a disease where the walls of the throat relax and narrow during sleep, interrupting normal breathing. (Dr Parry, 2014) There are two types: Apnoea is where the muscles and soft tissues in the throat relax and collapse sufficiently to cause a total blockage in the airflow for 10 seconds or more. Hypopnoea is a partial blockage of the airway that results in an airflow reduction of greater than 50% for 10 seconds or more (Dr Parry, 2014)
Symptoms for this disease include poor sleep quality, daytime sleepiness and mainly depression, where 50% of the population with OSA are also depressed. The severity of OSA is distinguished by the number of partial or complete cessations of breathing per hour during sleep, the apnea/hypopnea index (AHI). However, despite of these symptoms and relationships studies carried out fail to prove that the relationship between depression and OSA; however, as mentioned previously half of the population with OSA are depressed (A. Woo, 2010)
Memory and cognitive impairment
Sleep, while being not the sole function, supports the formation of memory. It is the most important function as it helps to establish the state of consciousness during wakefulness. It is emphasised that consciousness and the formation of long lasting memory are two mutually exclusive processes that cannot take place in brain’s neuronal networks one after another (Wilhelm, 2011, page 1)
Stability versus plasticity in memory
Refers to how the brain maintains previously learned memories while it continues to learn new things that in most cases override the old memories. There are 2 separate memory stores 1. Learns at a fast rate and hold information only temporarily 2. Leans at a slow rate and serves as long-term storage, however, there is also a slow rate of forgetting too. (Jan Born, 2011, page 2) Newly encoded memory traces are reactivated, upon subsequent periods of consolidation, and therefore become increasingly and gradually reorganised so that the representation in the brain in the slow learning long-term store are strengthened. Because encoding of information is used for both types of memory storage, it could interfere and disturb the proper consolidation process; therefore, to prevent this from happening, reactivation and redistribution of memories takes place during consolidation in offline periods e.g. during sleep when there is no encoding demands. The reason that this takes place during sleep is because it involves reactivation of fresh memory representations to promote their redistribution to the long-term store. These processes could largely interfere with the brain’s normal processing of external stimuli. There is also a contrast example, that during wakefulness synaptic consolidation may occur as well. (Wilhelm, 2011, page 2)
Research and evidence
There is now strong evidence that provides us and to come to the conclusion that the duration of sleep does have an effect on memory. During the duration of sleep, research shows that major memory systems e.g. for declarative memories (word pairs and card pair locations) and for procedural memories (finger taping skills). Furthermore, the memory was only acquired after the learning phase- this was proven by performing a certain test on individuals prior to sleep and the same test after the duration of sleep and, as predicted, the knowledge was better after the duration of sleep. (Ayoub, 2011, page 5)
Moreover, there are also other factors that facilitate access of a memory to sleep-dependant consolidation processes. Emotional memories were shown memory consolidation during post-learning sleep. Leading on from this, there was a difference in emotional and neutral memories such that emotional memories were remembered more than the neutral ones. Learned tasks with reward at the end also was proven increase memory consolidation compared to learned tasks without reward (Ayoub, 2011)
Narcolepsy
Narcolepsy is a neurological sleep disorder that leads majority of the time, to periods of intense sleepiness during the daytime. This is one of the symptoms, the others are cataplexy, hypnagogic hallucinations, and sleep paralysis. Among people suffering with narcolepsy, disrupted night-time sleep (DNS) is a common complaint and referred as a disease-related symptom; being a larger causing problem than sleep paralysis and hypnagogic hallucination. It is proven that DNS isn’t distinguished from other sleep disorders especially primary insomnia. Common problems that are seen patients with no only narcolepsy, but with other sleep disorders too are vivid dreaming, periodic leg movements, rapid eye movement [REM] behaviour disorder, and sleep apnea. This then tells us that DNS may be a secondary disease, to initial problems like sleep apnea or insomnia. (Mignot, 2013)
Schizophrenia
Schizophrenia is a mental disorder characterized by abnormal social behaviour and failure to recognize what is real. Symptoms that are common include false beliefs, unclear or confused thinking, auditory hallucinations, reduced social engagement etc. Sleep problems in schizophrenia is very common and often medication is prescribed. Sleep research has found two specific anomalies in schizophrenia that have a proven impact on cognition: 1. Circadian rhythm – In the point of view of psychiatrists is the tendency for patients to sleep when everyone else is awake i.e. during the daytime is what they find most difficult to treat. This is called circadian rhythm disorder, and occurs when the person's circadian sleep-wake drive from the suprachiasmatic nuclei of the hypothalamus is out of synchrony with the environment; the main influence on this innate circadian timing is light. 2. Electroencephalograms of reduced sleep spindles. (Wilson, 2012)
Conclusion
We can conclude that sleep deprivation has various effects, including the decrease of activity of the immune system via cytokine and interleukin secretions. Also sleep deprivation causes a reduction in brain function, more accurately a reallocation of functions towards the right hemisphere. Decrease in sleep can lead to elevations in blood pressure which over time can lead to cardiovascular disease. There is also a strong correlation identified between sleep apnea and hypertension. Cardiac output decrease causes pulmonary stretch receptors to activate the sympathetic nervous system. This results in increased blood pressure. Chronic sleep deprivation also has an impact on neuroendocrine function and glucose metabolism. The sleep deprivation caused alterations in metabolism and endocrine function result in obesity. There is a strong link between psychological factors and sleep. Obstructive sleep apnea (OSA) is the disease that mostly is caused by stress, as mentioned previously, 50% of the population with OSA are also depressed. Memory is heavily affected by sleep where because during the course of sleep, no encoding of information is undergone, therefore, reactivation and redistribution takes place during offline periods e.g. sleep. Narcolepsy is a disorder that leads to periods of intense sleepiness during the daytime and disrupted nighttime sleep is most commonly associated with narcolepsy. Research into sleep has found two specific anomalies in schizophrenia (Circadian rhythm, electroencephalograms of reduced sleep spindles), therefore we can conclude that they are heavily linked.
Bibliography
Aigboje, H.M.;D. D.-A.(2014) (1): Sleep Deprivation: Effect on Mental Task Performance of Military Cadets. International Journal of Humanities and Social Science , 4 (1). |
Amr Ayoub, Ina Molzow,Ines Wilhelm, Jan Born, Matthias Mo¨lle, Susanne Diekelmann. 2011. The Journal of Neuroscience. Sleep Selectively Enhances Memory Expected to Be of Future Relevance. 31(5):1563–1569 |
Ayas, N. T.; White, D. P.; Manson, J. E. (2003): A prospective study of sleep duration and coronary heart disease in women. Archives of Internal Medicine, 163, 205-209. |
Besedovsky L.; T. L.(2011). NCBI. Retrieved 11 6, 2014, from National center for Biotechnology Information: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3256323/ |
Cauter, E. (1999): Impact of sleep debt on metabolic and endocrine function. The Lancet, 354, 1435-1439. |
David, T.; Derrer, M. (2014, 3 10).(Retrieved 11 7, 2014), from Webmd: http://www.webmd.com/sleep-disorders/guide/tips-reduce-stress |
Dr Dion Parry, (2014). Obstructive sleep apnoea. England, Leeds. NHS UK |
Dr Tim Kenny, (2014). ‘What is depression?’ England, Leeds (No 2117205) |
Emmanuel Mignot, M.D., Ph.D., F.A.A.S.M., Jacques Montplaisir, M.D., Ph.D., Josh Paul,M.A., Phyllis Zee, M.D., Ph.D., F.A.A.S.M. Thomas Roth, Ph.D.,Todd Swick, M.D., F.A.A.S.M., Yves Dauvilliers, M.D. (2013). Disrupted Nighttime Sleep in Narcolepsy. 9(9): 955–965. |
Foundation, T. N. S. (2010): Sleep Apnea and Heart Disease [Online]. Available: http://sleepfoundation.org/sleep-news/sleep-apnea-and-heart-disease [Accessed October 21st 2014]. |
Franzen, P. L.; Gianaoros, P. J.; Marsland, A. L.; Hall, M. H., Siegel, G. J.; Dahl, R. E.; Buysse, D. J. (2011): Cardiovascular reactivity to acute psychological stress following sleep deprivation. Psychosomatic medicine, 73, 679-682. |
Ines Wilhelm, Jan Born. (2011). System consolidation of memory during sleep. 76:192–203 |
Latina, J. M.; Estes, N. A. M.; Garlitski, A. C. (2013): The Relationship between Obstructive Sleep Apnea and Atrial Fibrillation: A Complex Interplay. Pulmonary Medicine, 2013, 621736. |
Leproult, R. and Van Cauter E. (2010): Role of Sleep and Sleep Loss in Hormonal Release and Metabolism. Endocrine development, 17, 11-21. |
Mary A. Woo, Paul M. Macey mail,, Rajesh Kumar, Rebecca L. Cross, Ronald M. Harper. 2010. Relationship between Obstructive Sleep Apnea Severity and Sleep, Depression and Anxiety Symptoms in Newly-Diagnosed Patients. Article ID: 10.1371 |
Maurovich-Horvate, E. P. T.; Šonka K. (2008): The Effects of Sleep and Sleep Deprivation on Metabolic, Endocrine and Immune Parameters. Prague Medical Report, 109, 275-285. |
Morselli, L.; Leproult, R.; Balbo, M.; Spiegel, K. (2010): Role of sleep duration in the regulation of glucose metabolism and appetite. Best practice & research. Clinical endocrinology & metabolism, 24, 687-702. |
NCBI (National center for Biotechnology information). (2008, 10). Retrieved 11 10, 2014, from NCBI: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2656292/ |
Orzeł-gryglewska, J. (2010). consequences of sleep deprivation. (J. Orzeł-gryglewska, Ed.) International Journal of Occupational Medicine and Environmental Health , 23 (1), 95-114. |
Quan, S. F. (2009): Sleep Disturbances and their Relationship to Cardiovascular Disease. American journal of lifestyle medicine, 3, 55s-59s. |
Ratini, M. (2014). WebMd. (M. Ratini, Ed.) Retrieved 11 8, 2014, from Web Md: http://www.webmd.com/sleep-disorders/guide/sleep-requirements |
Redwine, L.; Hauger, R. L.; Gillin, J. C.; Irwin, M. (2000): Effects of Sleep and Sleep Deprivation on Interleukin-6, Growth Hormone, Cortisol, and Melatonin Levels in Humans. The Journal of Clinical Endocrinology & Metabolism, 85, 3597-3603. |
Reiter, R. J.; D.-X. T.; Korkmaz, A.; Shuran, M. (2012): Obesity and metabolic syndrome: Association with chronodisruption, sleep deprivation, and melatonin suppression. Anuals of Medicine 44, 564-577. |
Shahrad Taheri, L. L.; Austin, D.; Young, T.; Mignot, E. (2004): Short Sleep Duration Is Associated with Reduced Leptin, Elevated Ghrelin, and Increased Body Mass Index. PLOS Medicine, 100, 263-278 |
Spiegel,K.; Leproult, R.; Van Cauter, E. (1999): Impact of sleep debt on metabolic and endocrine function. The Lancet, 354, 1435-1439. |
Sue Wilson, PhD Spilios Argyropoulos, MSc, MRCPsych, PhD. (2012). Sleep in schizophrenia: time for closer attention. 200:308-316 |
Figures
Figure 1: Bartha, T 2014, Lecture Slides- Physiology of the Heart. Slide 77: Neural Factors Influencing Heart Rate. Viewed 21st October 2014 |
Figure 2: Bartha, T 2014, Lecture Slides- Endocrinology. Slide 132: Episodic Release of GH. Viewed 29st October 2014. |
Figure 3: WIKIPEDIA. 2014. The Corticotropin Axis [Online]. Available: http://en.wikipedia.org/wiki/Hypothalamic%E2%80%93pituitary%E2%80%93adrenal_axis [Accessed 21st October 2014]. |
