|
Size: 4581
Comment:
|
Size: 10085
Comment:
|
| Deletions are marked like this. | Additions are marked like this. |
| Line 4: | Line 4: |
| Line 32: | Line 33: |
Sleep Apnea Obstructive sleep apnea, a cause of sleep deprivation is also linked in patients developing heart disease. During sleep, there is a natural loss in musculature tone including muscles which encapsulate the pharynx. The pharynx and upper airspace is composed of muscles and soft tissue. With this loss of tone, in some patients, it can cause the airway to “collapse” , thus obstructing the airway. This airway occlusion results in decreased intrathoracic pressure, which therefore leads to an increased afterload of venous return, causing right ventricle distention and the interventricular septum to shift. Combination of these invents causes a decrease in left ventricular stroke volume which decreases the cardiac output significantly (Latina et al. 2013). Cardiac output decrease causes pulmonary stretch receptors to activate the sympathetic nervous system. Also hypoxia and hypercapnia caused by airway obstruction, stimulate peripheral and central chemoreceptors, also resulting in sympathetic activation. This sympathetic activation increases blood pressure by causing vasoconstriction in an effort to overcome these adverse effects. In a patient suffering with obstructive sleep apnea, they can encounter these surges hundreds of times per night, resulting in huge fluctuations in heart rate and blood pressure. In the long term, hypertension results, which can then lead to heart disease. Obesity Chronic sleep loss has a huge impact on neuroendocrine function and glucose metabolism, both which are underlying risk factors in obesity development. Sleep deprivation causes alterations in both metabolic and endocrine mechanisms. Such as; Decrease glucose tolerance and insulin sensitivity, Increased cortisol concentrations in the evening, Increased ghrelin concentration, Decreased leptin levels. These factors result in increased appetite and therefore at a higher risk of developing obesity. The brain, requires a constant glucose supply, even when food intake that provides the glucose does not occur. During sleep, this supply must be maintained. Studies have found that tolerance to glucose and insulin differed following sleep deprivation. Lack of sleep resulted in an increase in blood glucose level, lower insulin response and a slower glucose tolerance. Prolonged sleep deprivation may result in insulin resistance and development of type 2 diabetes by its affect on mechanisms of blood glucose level regulation. Or it may also indirectly result in type 2 diabetes by causing an increased appetitie (Morsell et al., 2010). Ghrelin is a stomach-derived peptide which has a primary role in energy balance by increasing food intake and bodyweight along with reduction in body fat utilization. Ghrelin has been identified as a sleep inducing factor by inducing slow-wave sleep and night time release of growth hormone, adrenocorticotropic hormone (ACTH) and cortisol. Ghrelin concentration was seen to increase individuals in the morning following sleep deprivation (Leproult, et Cauter, 2010; Russel et al 2012). Leptin, an adipocyte derived hormone is involved in energy metabolism and fat utilization. Under normal circumstances, leptin is involved with reducing feed intake. Leptin is involved in a insulin containing reflex mechanism in which, an increase in insulin following feed intake causes an increase in leptin. Leptin levels decrease following a night a sleep deprivation, which causes an increase in feed intake Sleep derived increase in ghrelin levels and decreased insulin result in a remarkable increase in appetite as there is a strong correlation between increased ghrelin-to-leptin ratio and increased appetite (Sharad et al, 1999). Orexin Neurons Orexin-containing neurons of the lateral hypothalamus have a crucial role in sleep and are involved in the regulation of energy homeostasis. Their site of action is in the same are as the leptin and ghrelin hormone response region, and they partake in its synthesis and secretion. As mentioned above leptin and ghrelin are the main hormones involved in feed intake. Decrease in leptin and increase in ghrelin, following sleep deprivation, suppress the activity of orexin neurons which also leads to increase in feed intake, but orexin also affects energy expenditure. Decreased orexin activity, causes a decrease in energy expenditure, causing an increased body mass index (BMI) from increased fat storage and less fat store energy utilisation. Growth Hormone The release of growth hormone from the adenohypophysis is stimulated by hypothalamic derived Growth Hormone Releasing Factor (GHRF) and is inhibited by somatostatin (growth hormone inhibition factor, GHIF). GHRF is also involved with inducing slow-wave-sleep, but its release is highly dependent upon the duration and quality of sleep (Redwine et al., 2000). GH has a circadian rhythm, meaning the majority of GH pulses occur shortly after the onset of sleep (figure 2). GH exerts its effects on various organs and tissues, while also stimulating release of further hormones in the liver. It is referred to as an anabolic hormone, as its involved in increasing amino acid uptake, protein synthesis which leads to increased growth. {{attachment:ghnew.png}} '''Fig 1.''' ''The Ciracadian Pattern of Growth Hormone. Diurinal levels are minimal in comparison with nocturnal levels. Sleep deprivation results in decreased growth hormone levels, affecting the circadian rhythm of growth hormone.'' |
Introduction
Stress is the body’s response towards daily life, in terms of noxious stimuli. There is a correlation between the severity of the stress response, due stimulus intensity, with the length of sleep. The process of sleep is a function of the body by which several hours are used to act on the regulatory systems of the internal environment; balancing out hormone production and breakdown and maintaining a healthy immune system. The average human can survive several days of sleeplessness but the reduction of sleep periods can result in diminishing heath and functioning. (David T. Derrer, 2014)
This essay attempts to look at the various causes and subsequent outcomes of sleep deprivation.
Types and Causes Sleep deprivation occurs when sleep is insufficient to support typical body functions, either as a result of an inefficient sleep period (quantity) or a disturbance in sleeping pattern (quality). It can be either acute; no sleep/ a reduction in total sleep time or it can be chronic; where an individual consistent sleep levels are less than that required for optimal functioning. (ORZEŁ-GRYGLEWSKA, 2010)
General sleep reduction- caused by daily sleep time reduction below level of optimum needs, absence of a single nights sleep or a shift in sleep in relation to circadian pattern. Examples include social eccentrics (partying), late shifts of work and general factors from contemporary lifestyle. Considerable sleep reduction- caused by lengthened insomnia over several days or complete sleep deprivation. Examples would include, experimental conditions or possible extreme situations, i.e., torture. Sleep reduction due to pathological processes- caused by depression, anxiety disorders, addiction/ chemical substance abuse, somatic/painful diseases or sleep disorders, i.e., subjective, idiopathic and psychophysiological insomnia. The sleep in these disorders is of low quality, delayed and shortened, and some genetic factors or enhanced by old age and chronic stress or traumatic experiences. (ORZEŁ-GRYGLEWSKA, 2010)
These different types of sleep deprivation can roll on to have an effect on the different systems inside the body as well as cognitive and general body function. Discussed below in more detail.
Effects
Physiological Cardiovascular Effects
- Sleep deprivation, like smoking is now noted as one of the main causes of developing heart disease. The possible reasoning for this, is that a decrease in sleep results in increased blood pressure, and sympathetic overactivity; known precursors for developing coronary heart disease. Sleep deprivation may be caused by sleep apnea which also can be a factor in developing heart disease (Quan 2009).
Increased Blood Pressure and Sympathetic Overactivity
Studies performed on healthy individuals, showed a significantly larger systolic blood pressure following one night of sleep deprivation, compared with non-sleep deprived individuals. One experiment examined the theory of this systolic increase being linked with stress induced reaction. They created a control, where subjects where not exposed to any form of stressful situation following sleep deprivation (Franzen et al., 2011). The same increase in systolic pressure was observed. Therefore highlighting a clear link between sleep deprivation and increased blood pressure. Without adequate rest periods sympathetic overactivity results. Normally, heart rate is controlled by a balance between the parasympathetic nervous system and the sympathetic nervous system. The parasympathetic innervation via the vagus nerve causes a decrease in heart rate by having a direct depressor effect on the sympathetic nervous system. Sympathetic nervous system elevates the heart rate by causing an muscarinic Acetylcholine activated elevation in cAMP, which causes elevation in heart rate Sympathetic overactivity, leads to inadequate depression via the parasympathetic vagus nerve and the heart rate remains increased as a result. Figure 1.1 highlights the parasympathetic suppressant effect on the heart rate. Long term sympathetic over-excitability results in hypertension, which leads to cardiovascular disease (Ayas et al., 2003).
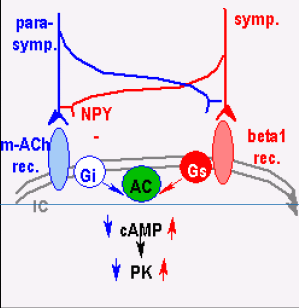
Fig 1. Sympathetic and Parasympathetic control of Heart Rate. This shoes the effect of the parasympathetic and sympathetic system on heart rate. Elevation in sympathetic activity counteracts the depressor effect of the parasympathetic system thus, resulting in increased heart rate. Sleep Apnea Obstructive sleep apnea, a cause of sleep deprivation is also linked in patients developing heart disease. During sleep, there is a natural loss in musculature tone including muscles which encapsulate the pharynx. The pharynx and upper airspace is composed of muscles and soft tissue. With this loss of tone, in some patients, it can cause the airway to “collapse” , thus obstructing the airway. This airway occlusion results in decreased intrathoracic pressure, which therefore leads to an increased afterload of venous return, causing right ventricle distention and the interventricular septum to shift. Combination of these invents causes a decrease in left ventricular stroke volume which decreases the cardiac output significantly (Latina et al. 2013). Obesity Chronic sleep loss has a huge impact on neuroendocrine function and glucose metabolism, both which are underlying risk factors in obesity development. Sleep deprivation causes alterations in both metabolic and endocrine mechanisms. Such as; Decrease glucose tolerance and insulin sensitivity, Increased cortisol concentrations in the evening, Increased ghrelin concentration, Decreased leptin levels. These factors result in increased appetite and therefore at a higher risk of developing obesity. The brain, requires a constant glucose supply, even when food intake that provides the glucose does not occur. During sleep, this supply must be maintained. Studies have found that tolerance to glucose and insulin differed following sleep deprivation. Lack of sleep resulted in an increase in blood glucose level, lower insulin response and a slower glucose tolerance. Prolonged sleep deprivation may result in insulin resistance and development of type 2 diabetes by its affect on mechanisms of blood glucose level regulation. Or it may also indirectly result in type 2 diabetes by causing an increased appetitie (Morsell et al., 2010). Ghrelin is a stomach-derived peptide which has a primary role in energy balance by increasing food intake and bodyweight along with reduction in body fat utilization. Ghrelin has been identified as a sleep inducing factor by inducing slow-wave sleep and night time release of growth hormone, adrenocorticotropic hormone (ACTH) and cortisol. Ghrelin concentration was seen to increase individuals in the morning following sleep deprivation (Leproult, et Cauter, 2010; Russel et al 2012). Leptin, an adipocyte derived hormone is involved in energy metabolism and fat utilization. Under normal circumstances, leptin is involved with reducing feed intake. Leptin is involved in a insulin containing reflex mechanism in which, an increase in insulin following feed intake causes an increase in leptin. Leptin levels decrease following a night a sleep deprivation, which causes an increase in feed intake Sleep derived increase in ghrelin levels and decreased insulin result in a remarkable increase in appetite as there is a strong correlation between increased ghrelin-to-leptin ratio and increased appetite (Sharad et al, 1999). Orexin Neurons Orexin-containing neurons of the lateral hypothalamus have a crucial role in sleep and are involved in the regulation of energy homeostasis. Their site of action is in the same are as the leptin and ghrelin hormone response region, and they partake in its synthesis and secretion. As mentioned above leptin and ghrelin are the main hormones involved in feed intake. Decrease in leptin and increase in ghrelin, following sleep deprivation, suppress the activity of orexin neurons which also leads to increase in feed intake, but orexin also affects energy expenditure. Decreased orexin activity, causes a decrease in energy expenditure, causing an increased body mass index (BMI) from increased fat storage and less fat store energy utilisation. Growth Hormone The release of growth hormone from the adenohypophysis is stimulated by hypothalamic derived Growth Hormone Releasing Factor (GHRF) and is inhibited by somatostatin (growth hormone inhibition factor, GHIF). GHRF is also involved with inducing slow-wave-sleep, but its release is highly dependent upon the duration and quality of sleep (Redwine et al., 2000). GH has a circadian rhythm, meaning the majority of GH pulses occur shortly after the onset of sleep (figure 2). GH exerts its effects on various organs and tissues, while also stimulating release of further hormones in the liver. It is referred to as an anabolic hormone, as its involved in increasing amino acid uptake, protein synthesis which leads to increased growth. 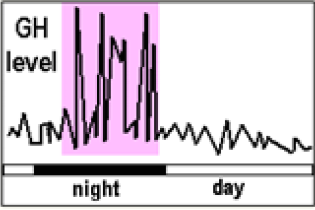 Fig 1.
Fig 1.
