Adverse Food Reactions In Canines
Contents
- Adverse food Reaction by definition
- How the Immunophysiology system works under normal physiological conditions
- The prevalence of dogs with lymphocyte proliferative responses to food allergens in canine allergic dermatitis
- Food hypersensitivity tests in dogs
- Patch testing and allergen-specific serum IgE and IgG antibodies in the diagnosis of canine adverse food reactions
- Evaluation of hydrolysed diets in dogs
- Conclusion
- References
Adverse food Reaction by definition
An adverse food reaction is any clinically abnormal response attributed to the ingestion of food or food additive. Adverse food reactions are categorized as either food allergies or food intolerance reactions. As the headline of the article indicates this essay will be only talking about food allergies. The difference between these two types is based on an immunologically immolated response, which occurs in food allergy. Therefore, food allergy can be defined as an immunologically mediated adverse food reaction to food unrelated to any physiological effect of the food or food additive.
How the Immunophysiology system works under normal physiological conditions
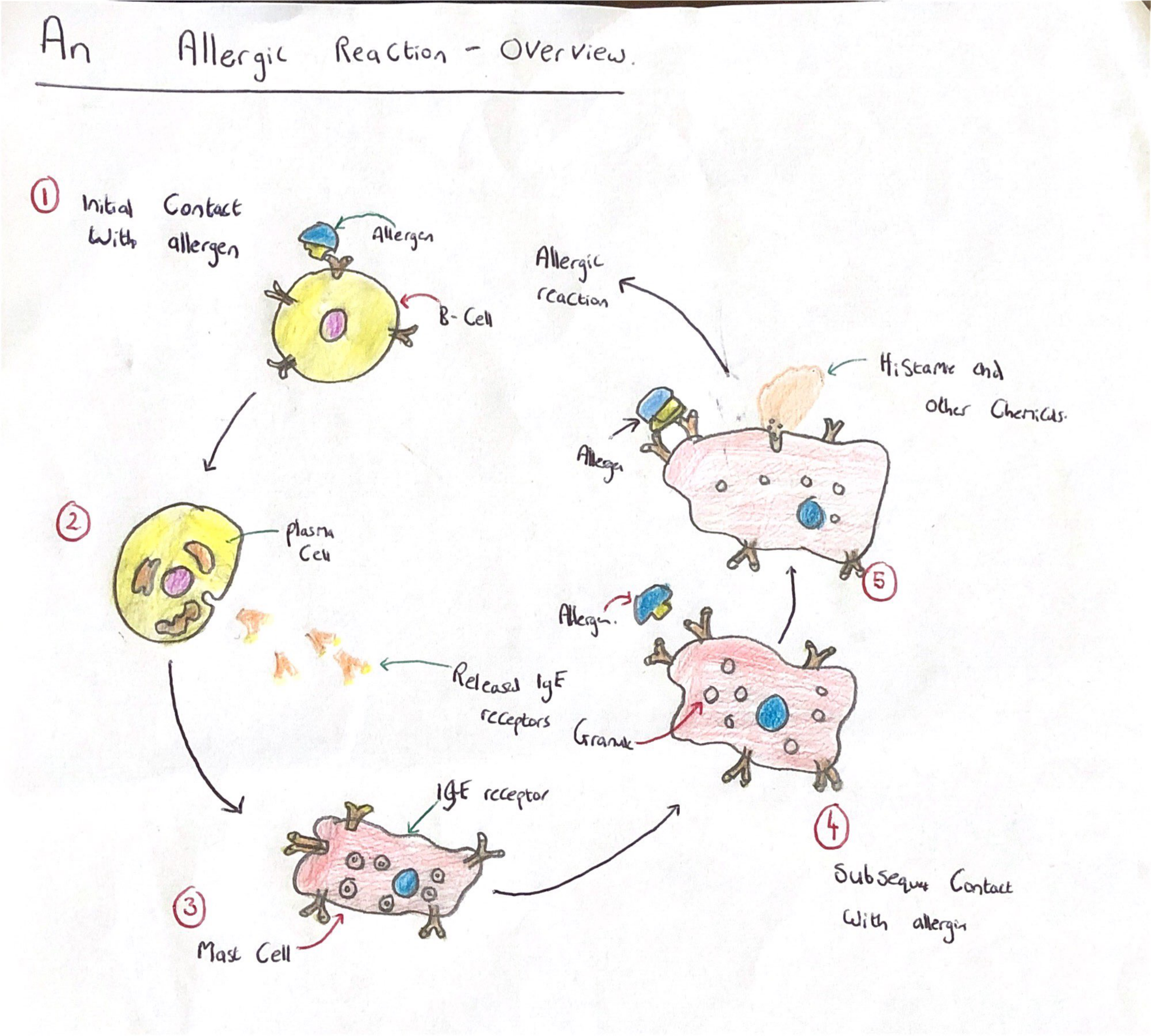
The immune system is linked to adverse food reactions in the body by causing an allergic reaction (Figure 1).
|
Figure 1 Allergic Reaction Overview |
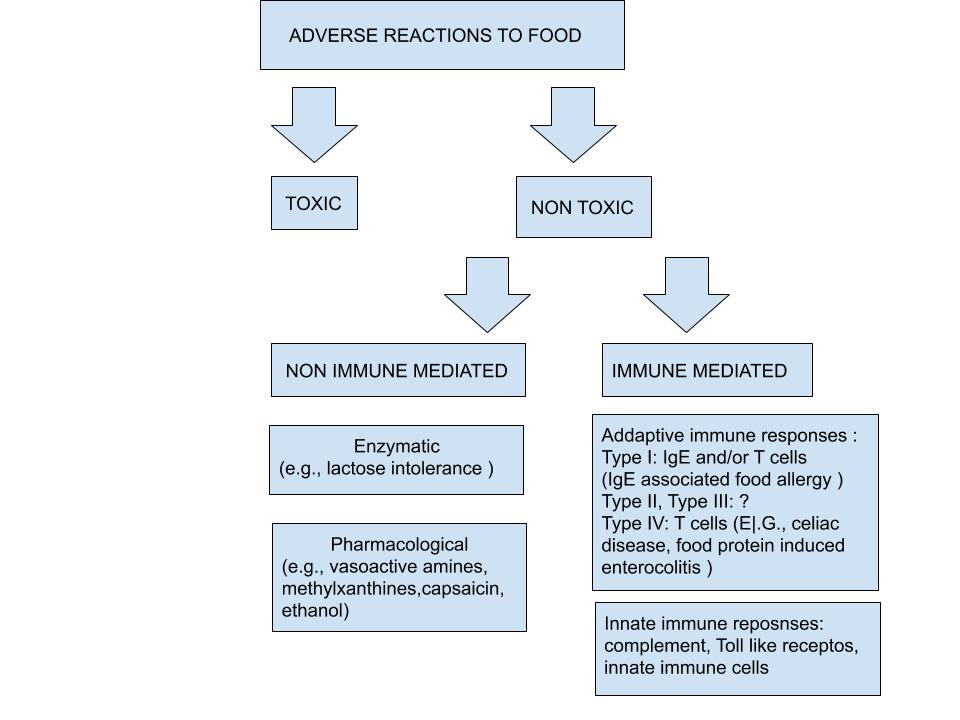
An allergic reaction occurs when the immune system overreacts to a harmless substance known as an allergen. These antibodies travel to the cells that release the chemicals and cause different symptoms.There are two basic pathways to remove pathogens (Figure 2); one is the natural immunity in which pathogens are removed by cellular and humoral elements. These are not antigen-specific but can react immediately. The second type of immunity requires the production of highly specific and very effective antibodies or immune cells against the non-self material. The response can be either cellular or humoral also in this case. This type is called acquired or specific or adaptive immune response. Materials triggering the immune response are called antigens. The specific defence molecules produced against these antigens are the antibodies (proteins either dissolved or bound to cells). Antigens are identified as non-self entities and are removed by the defence reactions of the body; the recognition of these foreign entities is due to the fact that the immune system produces immunoglobulins against almost an unlimited number of possible antigen structures by gene rearrangement.
|
Figure 2 Adverse Food Reaction |
The prevalence of dogs with lymphocyte proliferative responses to food allergens in canine allergic dermatitis
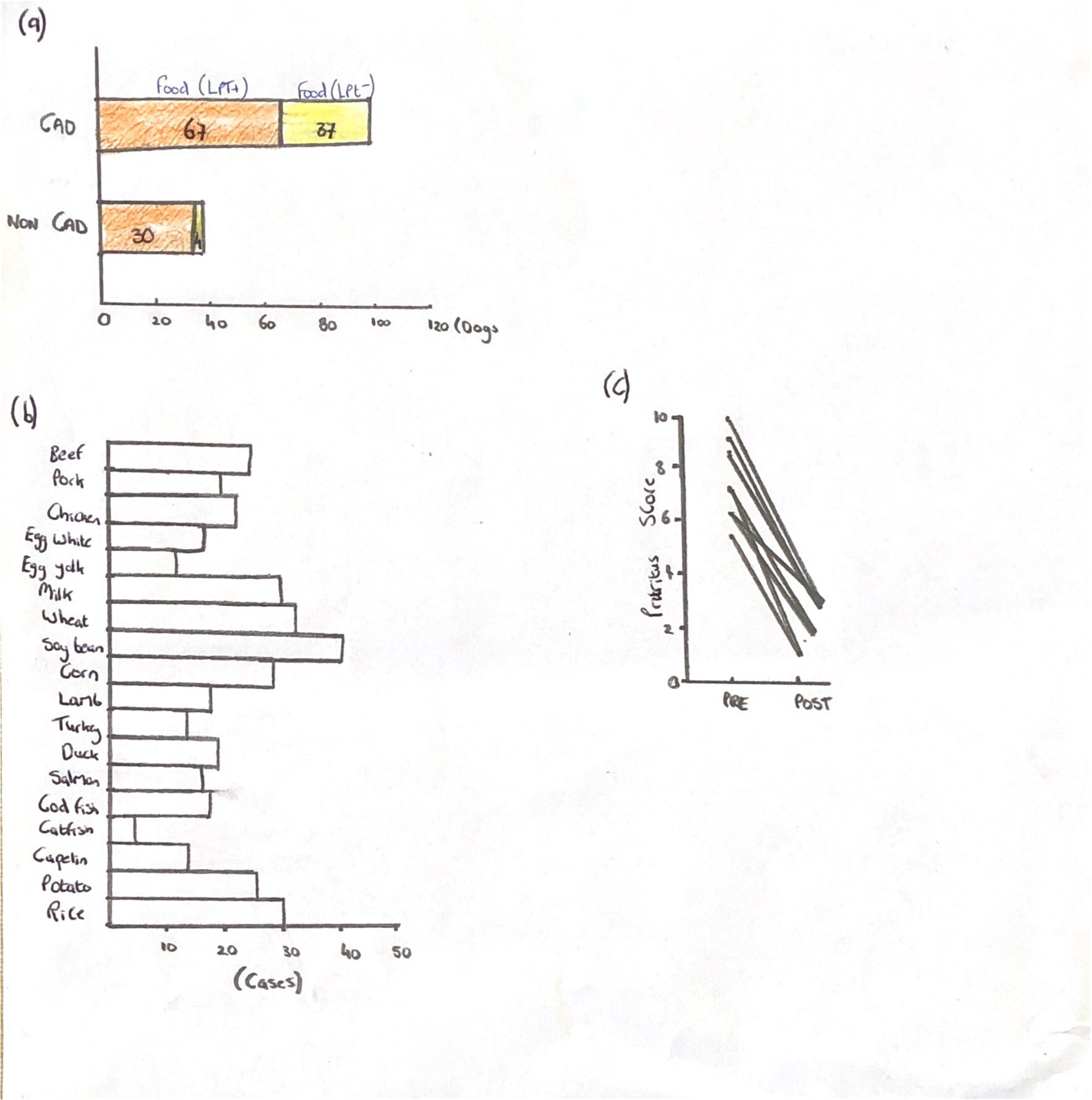
One way of identifying adverse food reactions in dogs is to examine the correlation between the results of lymphocyte proliferative test (LPT) specific to food allergens and allergic skin diseases in dogs. To prove this an investigation was conducted on allergic skin diseases in different dogs. Of the animals investigated, more than 75% cases had positive reactions in LPT specific to food allergens. Of these 97 dogs, 67 animals were diagnosed with canine atopic dermatitis (CAD) (Kawano et al., 2013)., some dogs do not have IgE antibodies due to environmental allergens (Favrot et al., 2010). Some dogs underwent an elimination diet trial based on the test results and all of them showed improvement in the pruritus (severe itching of the skin, as a symptom of various ailments). Therefore, we conclude that LPT is an effective diagnostic test for allergic skin disease. LTP is also useful in the identification of food allergens tested in elimination diets.
Allergic skin diseases in dogs can be broadly classified into the following two groups: atopic dermatitis and food allergy. Canine atopic dermatitis can be diagnosed either by intradermal skin test (IDST) or the presence of allergen-specific immunoglobulin E (IgE). However Allergen-specific IgE test is neither sensitive nor specific enough to diagnose food allergy (Paterson et al., 1995). The diagnosis of a food allergy is often challenging and clinical symptoms of food allergy overlap with those of CAD, so we end up with the question "is there a relationship between canine atopic dermatitis and cutaneous adverse food reaction ?" There’s at least a subset of dogs with cutaneous adverse food reactions due to IgE mediated food allergy (Guildford,1993). However, the vast majority of dogs suffering from cutaneous clinical signs of food allergy show neither igE mediated hypersensitivity nor any other immunologic mechanism. It was found that 13 - 30 % of dogs with cutaneous adverse food reactions have CAD (White, 1986). While 30 % of dogs with CAD exhibit adverse food reactions (Criep, 1968). However, despite high prevalence of CAD in dogs with cutaneous adverse food reactions, it is concluded that there is insufficient evidence supporting the association between CAD and cutaneous adverse food reaction. Below (Figure 3) we analyse data studying the relationship between CAD and LPT as well as foods most likely to cause reactions and food elimination diets (Kawano et al., 2013).
|
Figure 3 Graph a, The correltion between LPT and CAD: The upper bar indicates the numbers of dogs with CAD and whether they had a positive LPT or a negative one. And the lower bar shows the number of dogs without CAD and if they had a positive or negative LPT. From this we can see that for both dogs with and without CAD a higher number still had a positive LPT outcome. Graph b, food antigens and teh resulting LTP test: The graph indicates the allergens found by the LPT. The graph shows that soybean was the most significant cause of food allergy that induced an increase in LPT against the food allergen. This was followed by rice, potato, and wheat. Corn and milk also cause an increase in LPT against the food allergen. It can also be seen that the best meats with the lowest cases were the catfish and turkey. Egg yolks also had a low amount of cases in the LPT. Graph c, elimination diets and improvements in pruritus score: It Shows the changes in pruritus score in 12 dogs between before and after food elimination test (Kawano et al., 2013). |
Food hypersensitivity tests in dogs
As well as CAD, another disease caused by allergic reactions in canines is food hypersensitivity. It provokes pruritic skin disease, diarrhea, and vomiting (Rosser, 1993). It is thought to be mediated by type I, III or IV hypersensitivity (White, 1986). Type I reactions are always associated with the formation of IgE against food allergens . There is evidence showing involvement of IgG in type II or type III reactions in immune-mediated adverse reactions to food. Type IV reaction involve T cells, and has an important role in disorders such as celiac disease. There is evidence that the natural immune system, which includes complement, Toll-like receptors, and natural immune cells, also mediates immune reactions against certain food components.
Intradermal and antigen specific serum IgE testing showed positive reaction to some food allergens in hypersensitivity of dogs. However, the oral food provocation test has a much higher sensitivity than the previously mentioned tests. Therefore, non IgE mediated hypersensitivity might be also associated with the pathogenesis of food hypersensitivity in dogs (Jeffers et al., 1991). It was seen that the beef antigen is the most common food allergen in dogs; it was discovered that 60% of dogs with hypersensitivity showed clinical symptoms to it (Paterson et al., 2004 ). Other allergens included : chicken, egg, soybean, milk, corn, and wheat (Jeffers et al., 1996).
Another study also investigated intradermal testing, antigen specific IgE tests and oral provocation tests, as well as lymphocyte stimulation tests, in relation to food allergens and hypersensitivity. In the study, 11 dogs which were suspected to be hypersensitive based on clinical signs, were used. Lymphocyte stimulation test was performed with 9 kinds of food ingredients (beef , chicken , mid, egg, rice , wheat , corn, cod, tuna).The results were as followed: In oral food elimination and provocation test it was seen that, again, beef was the most common allergen in 73% of dogs. Wheat and rice caused food allergens in 18% of the dogs. Antigen specific IgE against various kinds of food antigens were detected in 31% of the dogs. In intradermal testing, strong reactions against food antigens were found in 11% of the dogs and with moderate reactions in 3 dogs against different allergens. The result of intradermal testing and IgE testing shows low correlation due to presence of non IgE mediated mechanism such as type IV hypersensitivity. The LST showed 82% of positive reactions. LST was a better test than IgE testing and intradermal due to the fact that the result of LST reflects reactions of both type I and IV hypersensitivity (Daguillard, 1972). Lymphocyte blastogenesis to food allergens was increased in dogs with food hypersensitivity indicating the presence of circulating lymphocyte reactive to food antigens in the peripheral blood.
Patch testing and allergen-specific serum IgE and IgG antibodies in the diagnosis of canine adverse food reactions
A final way to diagnose adverse food reactions is an elimination diet of 6–8 weeks with a protein and a carbohydrate source not previously fed. In canines, serum food allergen-specific antibody testing is widely used to identify suitable ingredients for such diets. Different studies were done to determine sensitivity, specificity, negative and positive predictability of patch testing with and serum antibody testing for a variety of common food stuffs. In this study allergic dogs underwent an elimination diet and challenged with selected food stuffs, food patch testing and serum testing for food-antigen specific IgE and IgG. Based on these results, a positive reaction of a dog on these tests is not very helpful, but a negative result indicates that this antigen is tolerated well. From the results we could conclude that patch testing (and to a lesser degree serum testing) can be helpful in choosing ingredients for an elimination diet in a dog with suspected adverse food reaction.(Bethlehem et al., 2012).
Evaluation of hydrolysed diets in dogs
In this section we will a evaluate method in which to manage adverse cutaneous reactions in the long term. In the study 14 Maltese x Beagle dogs were examined; they were chosen as they were known to have clinical hypersensitivity to corn and soy. In the first 12 months of their life, the dogs were fed a diet (Diet 1) containing chicken, corn, barley and soy (Jackson et al., 2003). After this time baseline data was collected and each dog was given a cutaneous clinical score (CCS), which evaluated erythema, excoriations and evidence of infection (Jackson et al, 2002). According to Saunders Comprehensive Veterinary Dictionary (2012), erythema and excoriations are recognised by redness of skin and superficial abrasions, resulting in removal of some skin particles, due to scratching.
Next over a period of 5 days Diet 2, consisting of duck and rice, was integrated and eventually replaced Diet 1. During the time the dogs were fed Diet 2 each of them was challenged orally with corn, soy and corn starch allergens. Each allergen was administered twice with a 24 hour interval, and between the different allergens there was a number of rest days (Jackson et al., 2003). As stated by Cave (2006), an allergen is an antigen which can bind to specific immunoglobin E (IgE) antibodies on the surface of cells and thus elicit mast cell degranulation. An oral challenge is when food containing known allergens is consumed under medical conditions with the aim of diagnosing or ruling out that specific food allergy (Boyce et al., 2010). These challenges are considered to be ‘the gold standard’ test in regard to diagnosis of food allergies as they show a clear ‘yes or no’ result (Niggemann, 2009). After each allergen was tested the CCS was re-evaluated and serum was collected via jugular venepuncture and analysed. If the CCS had increased by a minimum of 50% from its previous score, the animal was concluded to have had an adverse reaction. In order to keep variables to a minimum the CCS examination was carried out by the same person each time, and to prevent being influenced, the previous scores were not available to the examiner. The serum IgE was measured using ELISA- enzyme-linked immunosorbent assay (Jackson et al., 2003).
Intradermal skin testing was performed on day 0 (Diet 1) and on day 83 (Diet 2). Intradermal skin testing is used by veterinarians to look for allergen specific IgE antibodies (Olivry et al., 2007). The positive control was a monoclonal antidog immunoglobulin E, while the negative control was saline. Soy and corn allergens were used, and every dog was given three 10-fold dilutions. 20 minutes after administration the diameters of the reactions were measured. The result was said to be positive if it was greater than or equal to 50% of the positive control.
The animals continued Diet 2 for a total of 147 days and similarly to before, Diet 3 was then incorporated over several days and then fed exclusively up until day 160 when the trial ended. Diet 3 was a hydrolysed soy protein canine diet, a hydrolysed protein is one which is broken down into its peptides (Jackson et al., 2003). The main aim of a hydrolysed diet is to eliminate existing allergens and therefore stop immune recognition in an individual already sensitized to the intact protein. A further aim could also be to disturb the protein to a level where no antigens have the ability to cause an immune response and therefore leading to sensitisation of an individual which is not previously sensitized (Cave, 2006).
The results of the trial showed that all treatments effected CCS. The corn, soy and corn starch from the oral challenges all caused a significant increase in the CCS. While Diet 2 alone caused a statistically significant reduction in CCS at all time points evaluated. 21% of dogs had an adverse reaction to corn starch, 71% to corn and 78% to soy. In addition to this there was also a significant increase in soy-specific and corn-specific IgE concentrations observed between the samples taken on day 0 and on day 83. The initial oral challenge with corn starch caused a significant increase in the mean IgE concentration and this increase was sustained during the entire challenge period. It was realised there is a positive statistically significant correlation between the cutaneous clinical scores and corn-specific serum IgE. There is also a second positive correlation between the serum allergen-specific IgE and total IgE, concentrations. Finally, after the introduction of Diet 3 most of the dogs which had adverse reactions to soy and corn showed no increase in cutaneous clinical score (Jackson et al., 2003). This evidence shows that a hydrolysed protein diet can be a long-term management option for dogs suffering with adverse cutaneous reactions to soy and corn.
Conclusion
In conclusion it can be seen that there are multiple foods which cause adverse food reactions in dogs, including; corn, soy and even beef. From our research we discovered that there are several tests used to diagnose these allergies; such as elimination diets and patch testing as well as immunoglobin E serum detection. We also found that hydrolysed diets can be an effective long-term solution in managing these allergies. Having said this, a huge amount of research still needs to be carried out in regard to treating and diagnosing allergies. Writing this essay gave us an insight into a side of veterinary medicine that we didn’t realize was of such great importance.
References
- Bethlehem, S.; Bexley, J.; Mueller, R.S. (2012) Patch testing and allergen-specific serum IgE and IgG antibodies in the diagnosis of canine adverse food reactions. Veterinary Immunology and Immunopathology, 145(3-4): 582-589.
Boyce, J.A.; Assa'ad, A.; Burks, A.W.; Jones, S.M.; Sampson, H.A.; Wood, R.A.; Plaut, M.; Cooper, S.F.; Fenton, M.J.; Arshad, S.H.; Bahna, S.L.; Beck, L.A.; Byrd-Bredbenner, C.; Camargo, C.A.; Eichenfield, L.; Furuta, G.T.; Hanifin, J.M.; Jones, C.; Kraft, M.; Levy, B.D.; Lieberman, P.; Luccioli, S.; McCall, K.M.; Schneider, L.C.; Simon, R.A.; Simons, F.E.; Teach, S.J.; Yawn, B.P.; Schwaninger, J.M. (2010); Guidelines for the Diagnosis and Management of Food Allergy in the United States: Summary of the NIAID-Sponsored Expert Panel Report, 31(1): 61-75.
- Cave, N. J. (2006): Hydrolysed Protein Diets for Dogs and Cats. Veterinary Clinics Small Animal Practice, 36(6): 1251-1256.
- Criep, L.H. (1968): Allergy in veterinary medicine: Veterinary Medicine small animal clinic, 63(9): 855-9.
- Daguillard, F. (1972): Immunologic significance of in vitro lymphocyte responses. Med Clin North Am 56: 293–303.
- Favrot, C.; Steffan, J.; Seewald, W.; Picco, F. (2010): A prospective study on the clinical features of chronic canine atopic dermatitis and its diagnosis. Vet Dermatol 21: 23-31.
- Guildford, W.G. (1993): Experimental studies of gastrointestinal ischemia, reperfusion injury and food sensitivity in dogs, ph.D. thesis, University of California-Davis.
- Jackson, H. A.; Hammerberg, B. (2002): Evaluation of a spontaneous canine model of immunoglobulin E-mediated food hypersensitivity: dynamic changes in serum and fecal allergen-specific immunoglobulin E values relative to dietary change. Comparative Medicine, 52: 318–24.
- Jackson, H. A.; Jackson, M. W.; Coblentz, L.; Hammerberg, B. (2003): Evaluation of the clinical and allergen specific serum immunoglobulin E responses to oral challenge with corn starch, corn, soy and a soy hydrolysate diet in dogs with spontaneous food allergy. Veterinary Dermatology, 14: 181–187.
- Jeffers, J.G.; Meyer, E.K.; Sosis, E.J. (1996): Responses of dogs with food allergies to single-ingredient dietary provocation. Veterinary Medicine Association, 209: 608–611.
- Jeffers, J. G.; Shanley, K. J.; Meyer, E. K. (1991): Diagnostic testing of dogs for food hypersensitivity. Veterinary Association, 198: 245–250.
- Kawano, K.; Oumi, K.; Ashida, Y.; Horiuchi2, Y.; Mizuno, T. (2013): The Prevalence of dogs with lymphocyte proliferative responses to food allergens in canine allergic dermatitis: Polish Journal of Veterinary Sciences, 16(4): 735–739.
- Niggemann B. (2009): When is an oral food challenge positive? European Journal of allergy and clinical immunology 65: 2-6.
- Olivry, T.; Deboer, D.J.; Prelaud, P.; Bensignor, E. (2007) Food for thought: pondering the relationship between canine atopic dermatitis and cutaneous adverse food reactions. Veterinary dermatitis, 18(6): 390-391.
- Paterson, S. (1995): Food hypersensitivity in 20 dogs with skin and gastrointestinal signs. Small Animal practice 36: 529–534.
- Paterson, S.; Olivry,; Jeffers, Ishida, (2004): Food hypersensitivity in 20 dogs with skin and gastrointestinal signs. J Small Animal Practice 36: 529-534.
- Rosser, E.J. (1993): Diagnosis of food allergy in dogs. J Am Vet Med Association 203: 259–262.
- Studdert, V. P.; Gay, C. C; Blood, D. C. (2012) Saunders Comprehensive Veterinary Dictionary, Fourth Edition, Saunders Ltd, ISBN-13: 978-0702047435.
- White, S.D.(1986): Food hypersensitivity in 30 dogs. J Am Vet Med Association, 188(7): 695–698.