|
Size: 11742
Comment:
|
Size: 11837
Comment:
|
| Deletions are marked like this. | Additions are marked like this. |
| Line 10: | Line 10: |
| Lysophosphatidic acid is a phospholipid derivative that can act as a signalling molecule. It has the ability to stimulate cell proliferation and has been linked to cancer and cardiovascular diseases. LPA acts on many parts of the vascular system including platelets, monocytes, endothelial wall and smooth muscle cells In this essay we will discuss the role of LPA in relation to different areas surrounding the vascular system. The positive and negative effects of LPA can be seen through biological processes that occur in the body, angiogenesis and vasculogenesis, Atherosclerosis and atherothrombosis and G protein signalling.In relation to G protein signalling Five mammalian cell-surface LPA receptors have been identified to date, which have been appointed LPA1-LPA5. LPA1 is the most common of the five receptors, with high mRNA levels in the brain, colon, small intestine, placenta, and heart, and to some extent expression is seen in the pancreas, ovary, and prostate. 1 (Hecht, J.H., et al, 1996). |
Lysophosphatidic acid is a phospholipid derivative that can act as a signalling molecule. It has the ability to stimulate cell proliferation and has been linked to cancer and cardiovascular diseases. LPA acts on many parts of the vascular system including platelets, monocytes, endothelial wall and smooth muscle cells In this essay we will discuss the role of LPA in relation to different areas surrounding the vascular system. The positive and negative effects of LPA can be seen through biological processes that occur in the body, angiogenesis and vasculogenesis, Atherosclerosis and atherothrombosis and G protein signalling.In relation to G protein signalling Five mammalian cell-surface LPA receptors have been identified to date, which have been appointed LPA1-LPA5. LPA1 is the most common of the five receptors, with high mRNA levels in the brain, colon, small intestine, placenta, and heart, and to some extent expression is seen in the pancreas, ovary, and prostate. 1 (Hecht, J.H., et al, 1996). |
| Line 14: | Line 13: |
Figure 1 |
|
| Line 18: | Line 19: |
| Research today shows there are many strong links between Lysophosphatidic Acid and its role in angiogenesis. Angiogenesis is the growth of blood vessels from the existing vasculature. It occurs throughout life in both health and disease, beginning in-utero and continuing through to old age. No metabolically active tissue in the body is more than a few hundred micrometres from a capillary, the process of angiogenesis being responsible for this. (Adair and Montani, 2010). Therefore, its role in vessel generation could be seen as one of the most important ''beneficial'' aspects of LPA on the vascular system. | Research today shows there are many strong links between Lysophosphatidic Acid and its role in angiogenesis. Angiogenesis is the growth of blood vessels from the existing vasculature as seen in Figure 2. It occurs throughout life in both health and disease, beginning in-utero and continuing through to old age. No metabolically active tissue in the body is more than a few hundred micrometres from a capillary, the process of angiogenesis being responsible for this. (Adair and Montani, 2010). Therefore, its role in vessel generation could be seen as one of the most important ''beneficial'' aspects of LPA on the vascular system. Figure 2 |
| Line 30: | Line 33: |
| The correlation between LPA (lysophosphatidic acid) and Atherosclerosis can be seen through the description of Figure 1. Low density lipoproteins that have been modified by oxidation play an important role in atherosclerosis by increasing the amount of monocyte adhesion. | The correlation between LPA (lysophosphatidic acid) and Atherosclerosis can be seen through the description of Figure 3. Low density lipoproteins that have been modified by oxidation play an important role in atherosclerosis by increasing the amount of monocyte adhesion. Figure 3 |
| Line 36: | Line 41: |
| The mox-LDL increases the production of LPC (Lysophosphatidylcholine). The LPC is then converted into LPA by endothelial-derived ATX (autotaxin) into LPA. LPA causes the release of the chemokine CXCL1 (chemokine ligand 1) from the endothelial cells when both the LPA1 and LPA3 receptors are activated. CXCL1 is released on the surface of the endothelial surface and this begins the process of monocytes binding to the vessel wall. The monocytes can then enter the subendothelial space and change into macrophages, which are the primary cells of atherosclerotic plaques. | The mox-LDL increases the production of LPC (Lysophosphatidylcholine). The LPC is then converted into LPA by endothelial-derived ATX (autotaxin) into LPA as seen in Figure 4. LPA causes the release of the chemokine CXCL1 (chemokine ligand 1) from the endothelial cells when both the LPA1 and LPA3 receptors are activated. CXCL1 is released on the surface of the endothelial surface and this begins the process of monocytes binding to the vessel wall. The monocytes can then enter the subendothelial space and change into macrophages, which are the primary cells of atherosclerotic plaques. Figure 4 |
| Line 49: | Line 56: |
| 1. Teo, S.T., Yung, Y.C., Herr, D.R., Chun, J. (2009): Lysophosphatidic Acid (LPA) in Vascular Development and Disease. IUBMB LIFE 61: (8) 791-799 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4307796/]] 1. English, D., et al. (1999) Induction of endothelial cell chemotaxis by sphingosine 1-phosphate and stabilization of endothelial monolayer barrier function by lysophosphatidic acid, potential mediators of hematopoietic angiogenesis 8: (6) 627-634. 1. Rivera-Lopez, C.M., Tucker, A.L., Lynch, K.R. (2008): Lysophosphatidic acid (LPA) and angiogenesis. Angiogenesis 11: (3) 301-310. http://[[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2677190/]] 1. Stocker and Keaney, 2., & Levitan et al. (2004):Role of oxidative modifications in atherosclerosis. - NCBI - NIH: 1381-478 http://www.ncbi.nlm.nih.gov/pubmed/15383655 1. W. Siess, K. Z. (1999). Lysophosphatidic acid mediates the rapid activation of platelets and endothelial cells by mildly oxidized low density lipoprotein and accumulates in human atherosclerotic lesions. 6931-6936.http://www.ncbi.nlm.nih.gov/pubmed/10359816 1. J. Aoki, A. I. (2008). Two pathways for lysophosphatidic acid production. 513-518.http://www.ncbi.nlm.nih.gov/pubmed/18621144 |
1. Teo, S.T.; Yung, Y.C.; Herr, D.R.; Chun, J. (2009): Lysophosphatidic Acid (LPA) in Vascular Development and Disease. IUBMB LIFE 61: (8) 791-799 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4307796/]] 1. English, D.; et al. (1999): Induction of endothelial cell chemotaxis by sphingosine 1-phosphate and stabilization of endothelial monolayer barrier function by lysophosphatidic acid, potential mediators of hematopoietic angiogenesis 8: (6) 627-634. 1. Rivera-Lopez,; C.M.; Tucker,; A.L.; Lynch,; K.R. (2008): Lysophosphatidic acid (LPA) and angiogenesis. Angiogenesis 11: (3) 301-310. http://[[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2677190/]] 1. Stocker and Keaney, 2.,; & Levitan et al. (2004):Role of oxidative modifications in atherosclerosis. - NCBI - NIH: 1381-478 http://www.ncbi.nlm.nih.gov/pubmed/15383655 1. W. Siess,; K. Z. (1999): Lysophosphatidic acid mediates the rapid activation of platelets and endothelial cells by mildly oxidized low density lipoprotein and accumulates in human atherosclerotic lesions. 6931-6936.http://www.ncbi.nlm.nih.gov/pubmed/10359816 1. J. Aoki,; A. I. (2008); Two pathways for lysophosphatidic acid production. 513-518.http://www.ncbi.nlm.nih.gov/pubmed/18621144 |
| Line 56: | Line 63: |
| 1. E. Rother, R. B. (2003). Subtype-selective antagonists of lysophosphatidic Acid receptors inhibit platelet activation triggered by the lipid core of atherosclerotic plaques. 741-747.[[http://www.ncbi.nlm.nih.gov/pubmed/12885756.|http://www.ncbi.nlm.nih.gov/pubmed/12885756]] | 1. E. Rother,; R. B. (2003): Subtype-selective antagonists of lysophosphatidic Acid receptors inhibit platelet activation triggered by the lipid core of atherosclerotic plaques. 741-747.[[http://www.ncbi.nlm.nih.gov/pubmed/12885756.|http://www.ncbi.nlm.nih.gov/pubmed/12885756]] |
| Line 58: | Line 65: |
| 1. Schober, A., & Siess, W. (2012). Lysophosphatidic acid in atherosclerotic diseases. ''British Journal of Pharmacology, 167''(3), 465-482.http://www.ncbi.nlm.nih.gov/pubmed/22568609 | 1. Schober, A.; & Siess, W. (2012): Lysophosphatidic acid in atherosclerotic diseases. ''British Journal of Pharmacology, 167''(3), 465-482.http://www.ncbi.nlm.nih.gov/pubmed/22568609 |
Itt írjon a(z) lysophosphatidic_acid-ról/ről
The effect of lysophosphatidic acid on the vascular system
Catherine Dempsey, Geraldine Collins and Gráinne Gallagher
Contents
Abstract
Lysophosphatidic acid is a phospholipid derivative that can act as a signalling molecule. It has the ability to stimulate cell proliferation and has been linked to cancer and cardiovascular diseases. LPA acts on many parts of the vascular system including platelets, monocytes, endothelial wall and smooth muscle cells In this essay we will discuss the role of LPA in relation to different areas surrounding the vascular system. The positive and negative effects of LPA can be seen through biological processes that occur in the body, angiogenesis and vasculogenesis, Atherosclerosis and atherothrombosis and G protein signalling.In relation to G protein signalling Five mammalian cell-surface LPA receptors have been identified to date, which have been appointed LPA1-LPA5. LPA1 is the most common of the five receptors, with high mRNA levels in the brain, colon, small intestine, placenta, and heart, and to some extent expression is seen in the pancreas, ovary, and prostate. 1 (Hecht, J.H., et al, 1996).
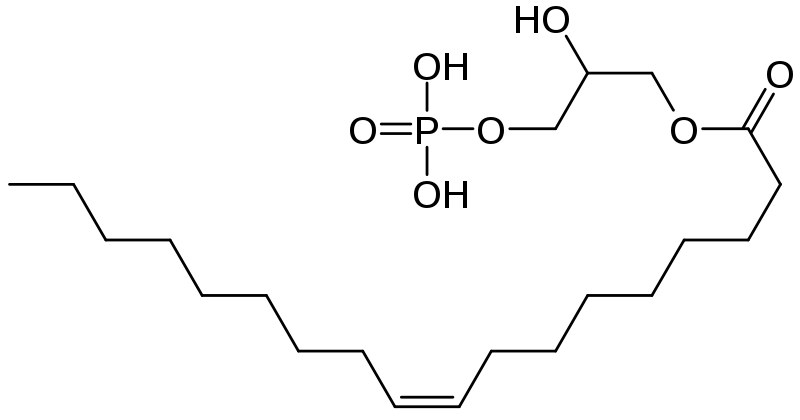
LPA is found in human plasma at a concentration of 0.4 – 0.5 µM 2 . According to Pages, C. et al (2001) it is synthesized through a number of different pathways including de-acylation of phosphatidic acid(PA), by phospholipases A1 and A2 (PLA1 and PLA2), acylation of glycerol 3-phosphate, by glycerophosphate acetyltransferase, phosphorylation of monoacylglycerol (MAG), by acylglycerol kinase (AGK), and hydrolysis of plasma lysophosphatidylcholine (LPC), by the lyso-phospholipase D (lyso-PLD), autotaxin. 3
Figure 1
Angiogenesis
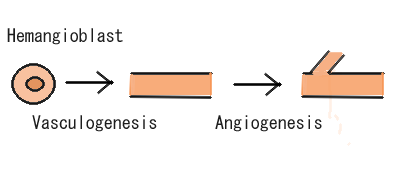
Research today shows there are many strong links between Lysophosphatidic Acid and its role in angiogenesis. Angiogenesis is the growth of blood vessels from the existing vasculature as seen in Figure 2. It occurs throughout life in both health and disease, beginning in-utero and continuing through to old age. No metabolically active tissue in the body is more than a few hundred micrometres from a capillary, the process of angiogenesis being responsible for this. (Adair and Montani, 2010). Therefore, its role in vessel generation could be seen as one of the most important beneficial aspects of LPA on the vascular system.
Figure 2
Teo, S.T., et al (2010) used adult bovine aortic cells and human umbilical vein endothelial cells, to observe how LPA aided the closure of wounded endothelial monolayers of the endothelial cells in vitro. This was due to a stimulation of both endothelial cell migration and proliferation, brought about by LPA treatment. In another study by English, D. et al (1999), LPA was shown to induce a chemotactic response in bovine pulmonary artery endothelial cells, similar in intensity to that observed with optimal levels of known endothelial cell chemo-attractants such as basic fibroblast growth factor (bFGF) and vascular endothelial growth factor (VEGF). Possibly the most interesting case we found in the course of our research was an experiment carried out by Rivera-Lopez, C.M. et al, on the chicken chorioallantoic membrane (CAM) assay (a well-established system for gauging the angiogenic activity of small molecules). They found that LPA had a strong angiogenic effect in-vivo compared to the control, and the vessels generated were considerably more robust than the VEGF-treated CAM. Furthermore, they deduced that synthetic LPA receptor agonists and antagonists mimic, or block this response, respectively. (They also revealed three avian receptor types that are orthologous to the mammalian LPA(1), LPA(2), and LPA(3) receptors.)
As we know, angiogenesis is needed for normal embryo development, and for wound-healing, the beneficial angiogenic effects of LPA, but it is also a critical process for tumour growth. In order for effective tumour growth, the mass will attract new vessels to obtain its oxygen and nutrient supply. Teo, S.T. et al (2009) reported that elevated LPA levels have been detected in the ascites of 98% of ovarian cancer patients, with 90% of patients with stage 1for early events in carcinogenesis. To add to the effects of LPA on the vascular system having adverse angiogenic effects aiding tumour growth, ovarian cancer cells have been found to produce LPA, thereby maintaining an LPA-rich environment. Using their results, they predicted that LPA receptor antagonists are a possible therapeutic route to inhibit angiogenesis in the case of tumour growth. Thus, we can deduce that although LPA has a positive effect on the vascular system with regard to angiogenesis, the angiogenesis stimulated may not always be beneficial, but instead having pathological effects.
Atheroscsclerosis
The effects of lysophosphatidic acid on the vascular system with a in depth look at atherosclerosis. Atherosclerosis is the narrowing of the arteries due to the disposition of plaque. Atherosclerosis is a slowly progressing, multifocal, chronic arterial disease that is characterized by inflamma  tory and regenerative processes, which lead to matrix remodelling and large lipid deposits. The retention of low-density lipoproteins (LDL) and activation of endothelial cells initiate atherosclerotic lesion formation in the inner layer (intima) of medium and large-sized arteries, such as coronary arteries and cerebral arteries, predominantly at predilection sites, where the laminar blood flow is disturbed (Libby et al., 2011; Weber and Noels, 2011) As cardiac disease is a leading cause of death throughout the Western world, research into this area may prevent the influx in cardiovascular disease in further years to come.
tory and regenerative processes, which lead to matrix remodelling and large lipid deposits. The retention of low-density lipoproteins (LDL) and activation of endothelial cells initiate atherosclerotic lesion formation in the inner layer (intima) of medium and large-sized arteries, such as coronary arteries and cerebral arteries, predominantly at predilection sites, where the laminar blood flow is disturbed (Libby et al., 2011; Weber and Noels, 2011) As cardiac disease is a leading cause of death throughout the Western world, research into this area may prevent the influx in cardiovascular disease in further years to come.
LDL Deposition in Vessels
The correlation between LPA (lysophosphatidic acid) and Atherosclerosis can be seen through the description of Figure 3. Low density lipoproteins that have been modified by oxidation play an important role in atherosclerosis by increasing the amount of monocyte adhesion.
Figure 3
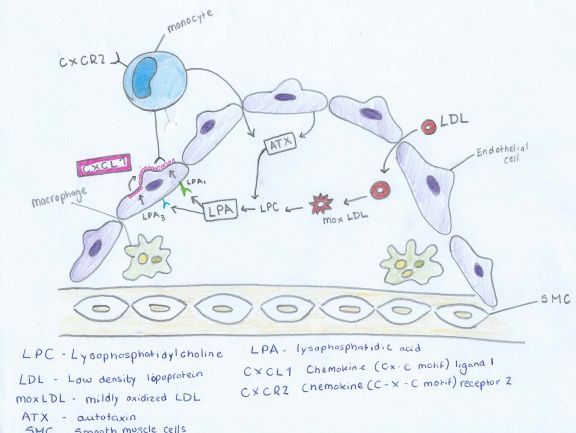
LDL (low density lipoprotein) enter thecells of the vessel wall. Here the LDL undergoes many modifications. Oxidation occurs. The degree of oxidation can occur in two different levels mildly oxidized LDL (mox - LDL) and extensively oxidized LDL (ox - LDL) (Stocker and Keaney & Levitan et al.)
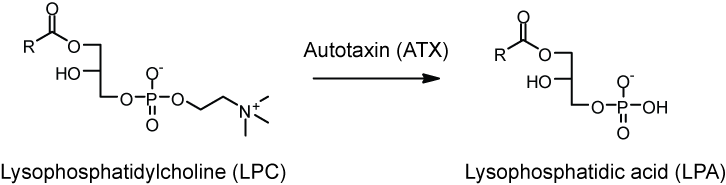
The mox-LDL increases the production of LPC (Lysophosphatidylcholine). The LPC is then converted into LPA by endothelial-derived ATX (autotaxin) into LPA as seen in Figure 4. LPA causes the release of the chemokine CXCL1 (chemokine ligand 1) from the endothelial cells when both the LPA1 and LPA3 receptors are activated. CXCL1 is released on the surface of the endothelial surface and this begins the process of monocytes binding to the vessel wall. The monocytes can then enter the subendothelial space and change into macrophages, which are the primary cells of atherosclerotic plaques.
Figure 4
Platelet activation and mild oxidation of LDL leads to LPA biosynthesis ( (W. Siess, 1999) (J. Aoki, 2008)), and elevated LPA levels are present in the atherosclerotic lesion core (E. Rother, 2003). We also found that LPA accumulated in and was the primary platelet-activating lipid of atherosclerotic plaques. Notably, the amount of LPA within the human carotid atherosclerotic lesion was highest in the lipid-rich core, the region most thrombogenic and most prone to rupture. Given the potent biological activity of LPA on platelets and on cells of the vessel wall, our study identifies LPA as an atherothrombogenic molecule and suggests a possible strategy to prevent and treat atherosclerosis and cardio cerebrovascular diseases. (W. Siess, 1999) Through this repetitive cycle the plaque deposition increases and the width of the narrowing vessels decreases which in turn declines blood flow to the vital organs and back to the heart.
G protein signalling
Conclusion
During the course of our exploration into the subject of LPA and its vascular role, it has become clear to us that there are many research opportunities in this area, as it is an ongoing point of interest in medicine today. As we have highlighted in our essay, LPA has both beneficial and adverse effects on the vascular system. The investigation done by researchers thus far serves as valuable groundwork for future findings, that will no doubt aid our understanding of the relevant diseases, and hopefully open doors to preventative measures and possible cures to the pathological situations we have discussed. We have considered the vital role Lysophosphatidic Acid plays in angiogenesis, the subject we found to be the most beneficial aspect of LPA discovered to date. It is likely that an effective LPA receptor agonist/antagonist can be synthesised, to mimic or inhibit the angiogenic effects of LPA – the inhibitory possibility being a promising aspect in the control of tumour growth and invasion. On the other hand, we have researched the negative effects of LPA on the vascular system, its role in atherosclerosis as an atherothrombogenic molecule capable of oxidising LDL, being of interest to us.
References
Bibliography
Adair, T.H.; Montani, J.P. (2010): Angiogenesis. Colloquium Series on Integrated Systems Physiology: From Molecule to Function 2: (1) 1-84 http://www.ncbi.nlm.nih.gov/books/NBK53242/]]
Teo, S.T.; Yung, Y.C.; Herr, D.R.; Chun, J. (2009): Lysophosphatidic Acid (LPA) in Vascular Development and Disease. IUBMB LIFE 61: (8) 791-799 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4307796/]]
- English, D.; et al. (1999): Induction of endothelial cell chemotaxis by sphingosine 1-phosphate and stabilization of endothelial monolayer barrier function by lysophosphatidic acid, potential mediators of hematopoietic angiogenesis 8: (6) 627-634.
Rivera-Lopez,; C.M.; Tucker,; A.L.; Lynch,; K.R. (2008): Lysophosphatidic acid (LPA) and angiogenesis. Angiogenesis 11: (3) 301-310. http://[[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2677190/]]
Stocker and Keaney, 2.,; & Levitan et al. (2004):Role of oxidative modifications in atherosclerosis. - NCBI - NIH: 1381-478 http://www.ncbi.nlm.nih.gov/pubmed/15383655
W. Siess,; K. Z. (1999): Lysophosphatidic acid mediates the rapid activation of platelets and endothelial cells by mildly oxidized low density lipoprotein and accumulates in human atherosclerotic lesions. 6931-6936.http://www.ncbi.nlm.nih.gov/pubmed/10359816
J. Aoki,; A. I. (2008); Two pathways for lysophosphatidic acid production. 513-518.http://www.ncbi.nlm.nih.gov/pubmed/18621144
E. Rother,; R. B. (2003): Subtype-selective antagonists of lysophosphatidic Acid receptors inhibit platelet activation triggered by the lipid core of atherosclerotic plaques. 741-747.http://www.ncbi.nlm.nih.gov/pubmed/12885756
Schober, A.; & Siess, W. (2012): Lysophosphatidic acid in atherosclerotic diseases. British Journal of Pharmacology, 167(3), 465-482.http://www.ncbi.nlm.nih.gov/pubmed/22568609
