Itt írjon a(z) lysophosphatidic_acid-ról/ről
The effect of lysophosphatidic acid on the vascular system
Contents
Abstract
Lysophosphatidic acid is a phospholipid derivative that can act as a signalling molecule. It has the ability to stimulate cell proliferation and has been linked to cancer and cardiovascular diseases. LPA acts on many parts of the vascular system including platelets, monocytes, endothelial wall and smooth muscle cells In this essay we will discuss the role of LPA in relation to different areas surrounding the vascular system. The positive and negative effects of LPA can be seen through biological processes that occur in the body, angiogenesis and vasculogenesis, Atherosclerosis and atherothrombosis and G protein signalling.
Angiogenesis
Atheroscsclerosis
The effects of lysophosphatidic acid on the vascular system with a in depth look at atherosclerosis. Atherosclerosis is the narrowing of the arteries due to the disposition of plaque. Atherosclerosis is a slowly progressing, multifocal, chronic arterial disease that is characterized by inflamma  tory and regenerative processes, which lead to matrix remodelling and large lipid deposits. The retention of low-density lipoproteins (LDL) and activation of endothelial cells initiate atherosclerotic lesion formation in the inner layer (intima) of medium and large-sized arteries, such as coronary arteries and cerebral arteries, predominantly at predilection sites, where the laminar blood flow is disturbed (Libby et al., 2011; Weber and Noels, 2011) As cardiac disease is a leading cause of death throughout the Western world, research into this area may prevent the influx in cardiovascular disease in further years to come.
tory and regenerative processes, which lead to matrix remodelling and large lipid deposits. The retention of low-density lipoproteins (LDL) and activation of endothelial cells initiate atherosclerotic lesion formation in the inner layer (intima) of medium and large-sized arteries, such as coronary arteries and cerebral arteries, predominantly at predilection sites, where the laminar blood flow is disturbed (Libby et al., 2011; Weber and Noels, 2011) As cardiac disease is a leading cause of death throughout the Western world, research into this area may prevent the influx in cardiovascular disease in further years to come.
LDL Deposition in Vessels
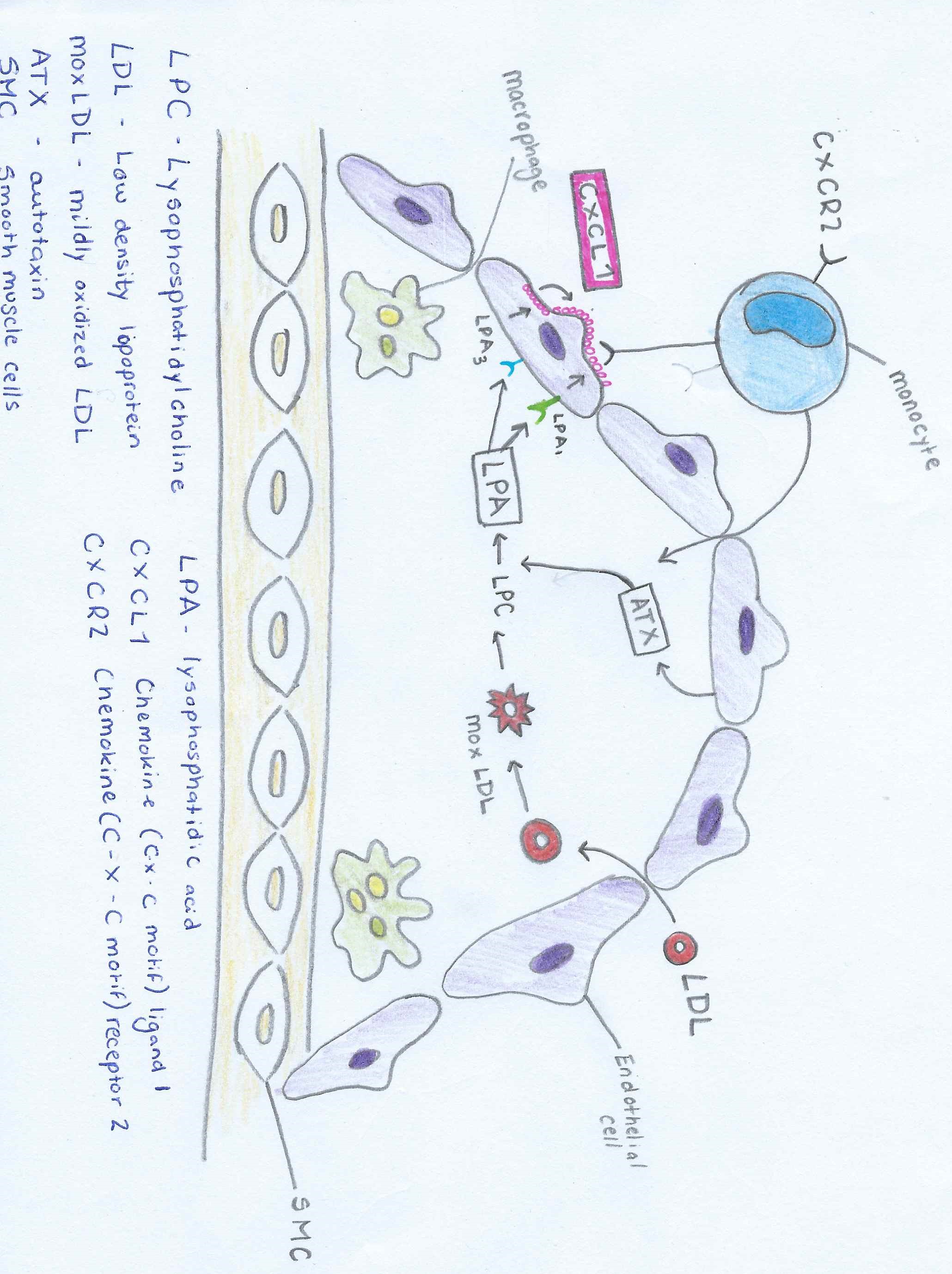
The correlation between LPA (lysophosphatidic acid) and Atherosclerosis can be seen through the description of Figure 1. Low density lipoproteins that have been modified by oxidation play an important role in atherosclerosis by increasing the amount of monocyte adhesion.
LDL (low density lipoprotein) enter thecells of the vessel wall. Here the LDL undergoes many modifications. Oxidation occurs. The degree of oxidation can occur in two different levels mildly oxidized LDL (mox - LDL) and extensively oxidized LDL (ox - LDL) (Stocker and Keaney & Levitan et al.)
The mox-LDL increases the production of LPC (Lysophosphatidylcholine). The LPC is then converted into LPA by endothelial-derived ATX (autotaxin) into LPA. LPA causes the release of the chemokine CXCL1 (chemokine ligand 1) from the endothelial cells when both the LPA1 and LPA3 receptors are activated. CXCL1 is released on the surface of the endothelial surface and this begins the process of monocytes binding to the vessel wall. The monocytes can then enter the subendothelial space and change into macrophages, which are the primary cells of atherosclerotic plaques.
Platelet activation and mild oxidation of LDL leads to LPA biosynthesis ( (W. Siess, 1999) (J. Aoki, 2008)), and elevated LPA levels are present in the atherosclerotic lesion core (E. Rother, 2003). We also found that LPA accumulated in and was the primary platelet-activating lipid of atherosclerotic plaques. Notably, the amount of LPA within the human carotid atherosclerotic lesion was highest in the lipid-rich core, the region most thrombogenic and most prone to rupture. Given the potent biological activity of LPA on platelets and on cells of the vessel wall, our study identifies LPA as an atherothrombogenic molecule and suggests a possible strategy to prevent and treat atherosclerosis and cardio cerebrovascular diseases. (W. Siess, 1999) Through this repetitive cycle the plaque deposition increases and the width of the narrowing vessels decreases which in turn declines blood flow to the vital organs and back to the heart.
G protein signalling
Conclusion