Physiology of pain addiction; behavioural effects
Addiction is a condition that arises when a being consumes substances or engages in activities that can be pleasurable at first, but the prolonged ingestion or act of which becomes a necessity. It emerges by the search of the ‘euphoric’ feeling a substance or activity brings with it. This feeling is the cause of the increase of the level of the striatal dopamine neurotransmitter. Users may not be aware that their compulsive behaviour is out of control and also once a being is addicted an entirely separate set of events or stressors may sustain and maybe amplify the addiction. Addiction can eventually lead to abuse.
When relating addiction to pain, it is actually the endorphins released in the system which aid the dopamine release and gets a being addicted, forming a dependency on their release.
Contents
Pain
Pain is a feeling of discomfort, distress or even agony depending on how severe it is. It has been defined as a biopsychosocial phenomenon that includes sensory, emotional, cognitive, developmental, behavioral, spiritual, and cultural components (Salsitz, 2015). It is part of the body's defense system, producing a reflexive retraction from the painful stimulus, and protects the affected body part while it heals, and also avoid that harmful situation in the future. Pain can be either acute or chronic. Both types can be intense but chronic is the type of pain that lasts much longer, while acute pain is short lived.
Pain stimuli starts from an electrical impulse from sensory receptors of the skin - nociceptors - to the spinal cord, acting as a relay center. The electrical impulse can be suppressed or enhanced before going to the brain. The brain then, produces several different neuroreceptors - such as glutamate-receptor - which then cause an impulse and reaches the thalamus and after the brain cortex.
Pain management
Pain management can be natural or artificial:
Natural pain management
One of the main types of these endogenous opioids are beta endorphins. These are neuropeptides, which possess morphine like effects and are involved in the processes which bring happiness to a being - maybe even give a euphoric feeling. This is the part of the process which can get addicting.
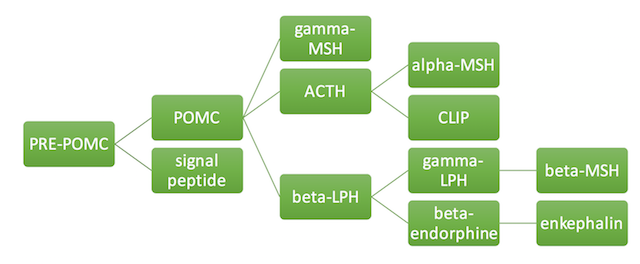
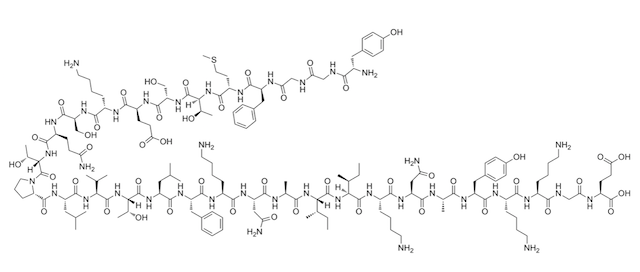
Physiological stressors such as pain, stimulate the synthesis of the the corticotroponin-releasing hormone (CRH) in the hypothalamus. This hormone is the one which triggers the anterior pituitary gland to synthesise the beta-endorphins. They are synthesised from their precursor protein proopiomelanocortin (POMC) along with other hormones such as the alpha-melanocyte stimulating hormone (MSH) and the adrenocorticotropin (ACTH). Beta-endorphins are also stored in the anterior pituitary. When there are enough beta-endorphins a negative feedback inhibits the further production of CRH (Sprouse-Blum et al., 2010).
|
Beta-endorphins act in both the peripheral and the central nervous system. They produce analgesia by binding to opioid receptors (usually the mu subtype). They bind to the receptors at both the presynaptic and postsynaptic nerve terminals but they mostly exert their effect through the presynaptic binding. In the peripheral nervous system (PNS), a cascade of reactions is induced after binding, which result in the inhibition of tachykinins release. These proteins - an example being substance P - are involved in the transmission of pain. In the central nervous system (CNS) the beta-endorphins inhibit the release of GABA, an inhibitory neurotransmitter, which then results in the overproduction of dopamine - a compound associated with pleasure (Sprouse-Blum et al., 2010).
|
Artificial pain management
Opioid therapy is regarded as necessary in the treatment of acute and chronic pain. These artificial opioids resemble the functions of endogenous opioids by relieving pain and giving the sense of a ‘high’ to the user - described as analgesia. These do so by binding to the same receptors of the endogenous opioids (mostly the mu-receptors) and so a sense of competition between the endogenous and the external opioids evolves when they are administered to the body. The external opioids can also inhibit the production of the endogenous opioid (Sprouse-Blum et al., 2010; Cheatle, 2016).
Morphine is the most commonly used pain reliever in medicine and quite effective for post-operation pain and for cancer pain. However, in order for the morphine (and any other artificial opioids) to work, they have to be injected into inflamed tissue (Akural et al., 2015).
Getting addicted to these opioids is quite easy, especially for people who have a history of opioid and drug abuse. Research has shown that patients with no prior use and abuse of opioids, being presently treated with opioid pain medications do not experience a sense of euphoria. For those that do get addicted to opioids substitution medications such as methadone and buprenorphine are the current pharmacotherapy used. These also bind to the opioid receptors of the brain but do not produce an analgesic effect (Ling et al., 2011).
Cannabinoids are another, relatively new way of treating pain. They are mostly being used amongst young people who have a history of Substance Use Disorder (SUD). Research conducted to compare medical cannabis to the traditional pain treatment opioids shows that medical cannabis can also reduce the amount of pain to the same certain level as the other opioids. However it has been resulted that medical cannabis users, consume other types of pain treatment in comparison to the non-medical cannabis users (Ashrafioun et al., 2014).
Pain Addiction
Self-harm
|
Self-harm is defined as a repetitive, intentional, direct injury to one’s body. It is has been stated that the reason of these behaviours happen in certain individuals, as a way of regulation when one undergoes an emotional degradation occurring due to stressful events and social situations.
Examples of self-harm include:
- Cutting (for example with a razor blade)
- Burning one’s own body
- Bruising
- Punching objects (for example a wall)
- Pulling out of hair
Suicidal and non-suicidal self-harm
There are two types of self-harm, that is suicidal (SSI) and non-suicidal self-harm (NSSI). NSSI has been a clinical problem with high prevalence rates in young individuals mostly.
Even though there are many cases of NSSI, the neurobiological background of this is still poorly understood. In current classificatory systems, Non-suicidal self-injury is regarded as a symptom of borderline personality disorder (BPD). When one does self-harm consciously - a behaviour which can include suicidal intent, it is widely described as “An act with a non-fatal outcome in which an individual deliberately did one or more of the following: initiated behaviour (for example, self- cutting, jumping from a height), which they intended to cause self-harm; ingested a substance in excess of the prescribed or generally recognised therapeutic dose; ingested a non-ingestible substance or object”. However since NSSI is still in risk of developing a suicidal attempt, the neurological background of these clinical phenomena may be comparable (Groschwitz and Plener, 2012).
The risk of both SSI and NSSI can be both influenced by intrapersonal factors (existing within the mind) which make an individual more vulnerable, such as high aversive emotions and cognitions as well as poor distress tolerance. These could be due to genetic susceptibility causing high emotional and high cognitive reactivity which could also happen due to environmental adversities. (Groschwitz and Plener, 2012)
Emotional and physiological states causing self-harm
The following describes differences in physiological concentrations of natural chemicals found in the body, comparing those who self-harm and those who don't. There is mixed evidence concerning differing physiological states in individuals with some kind of psychopathology, however a decrease in physiological tension in acts of NSSI has been reported many times.
Nock and Mendes (2008) compared 62 adolescents with a history of NSSI to 30 matched controls without NSSI. Physiological hyperarousal when confronted with a distressing task was found in the adolescents with NSSI (hyperarousal is measured by skin conductance).
There is mixed evidence concerning differing physiological states in individuals with some kind of psychopathology, however a decrease in physiological tension in acts of NSSI has been reported many times.
In the experiment of Kaess (2012) did not find any differences in the heart rate of adolescents with NSSI and healthy ones, while either finding any differences in skin conductance.
Two studies reported that imagining an act of self injury can decreases physiological tension, as measured example per skin conductance and heart rate in individuals with self injurious behaviours (Brain et al.,1998; Haines et al.,1995).
A rapidly lowered heart rate was discovered when rhesus monkeys repeatedly self injured themselves, for example when biting themselves (Novak 2003).
Neuroimagining
A number of studies have found abnormalities in brain morphology and neuronal activity in patients with NSSI and BPD. Hyperarousal in limbic structures like the amygdala and the anterior cingulate cortex were found to be repeated outcomes of fMRI studies. Individuals which were associated with parasuicidal behaviours had an increased pituitary gland volume which showed higher levels of post-dexamethasone cortisol that could be caused by a hyperactive axis.
Lipids
Low cholesterol concentrations and a low level of essential fatty acid content have both been linked to self-mutilating behaviours, even though the results on low cholesterol and suicide attempts are inconsistent. Example: Roaldset (2010) found significantly lower triglyceride levels in patients who showed suicidal and self-mutilating behaviour. A low high-density lipoprotein (HDL) concentration was a significant predictor for inpatient self-mutilation.
However due to a low sensitivity these measures cannot be considered too much because they are not truly accurate enough. Since serum cholesterol levels are influenced by natural factors like gender, age, diet etc., they might not serve as the right markers.
Neurotransmitters
|
Although inconsistent, evidence that serotonin deficiency may cause self-harming behaviours may be true (Groschwitz and Plener, 2012). Even though there has been more of a relation to aggressive behaviours rather than self-harm. There is evidence that decreases in 5-hydroxytryptamine (5-HT) receptors (serotonin receptors) is linked to aggressive behaviours, depression and suicide attempts. Monkeys performing self-injurious behaviour have also been diagnosed with a decreased function of the 5-HT system. In the experiment of Watson (2009) there was a different result, there were no differences in blood serum serotonin levels in bush babies with self-injurious behaviours and those without.
Only limited evidence has been found about the connection of dopamine with NSSI. From animal research, an increase in the mice biting themselves with dopamine agonists has been reported after the mice being exposed to amphetamine.
There have been consistent results from studies on cortisol concentration in individuals with self-harm and suicidal behaviour, the results were a decrease in the cortisol concentration. There is an interaction between the HPA- axis with endogenous opioids and serotogionic mechanisms which are involved in the level of secretion of cortisol (Heim et al., 2000). According to Heim (2000) a post-traumatic stress disorder may influence cortisol secretion negatively. Another study also reported a low level of cortisol in rhesus monkeys which were biting themselves, in opposition to those monkeys which were relocated and not biting themselves. The same situation was found in bush babies, the ones with the lower cortisol levels were associated with self injurious behaviours (Watson et al., 2009).
|
Endogenous opioids
Lower levels of endogenous opioids have been found in individuals which perform self-harm. This in fact could be a possibility to why the self-harm act itself is addictive (addiction to the pain). Endogenous opioids have been linked to several abnormal behaviours like BPD (Borderline Personality Disorder) or pervasive development disorders of which NSSI and self-mutilation are considered to be part of the symptoms. Opioids are released when a body feels pain, this causes addictive behaviours because it gives a euphoric feeling. Addictive qualities of NSSI have been suggested in past studies this therefore underlines the importance of endogenous opioids in self-injury.
Two studies reported that imagining an act of self-injury itself can also decrease physiological tension, as measured for example per skin conductance and heart rate in individuals with self-injurious behaviours (Brain et al.,1998; Haines et al.,1995).
According to a homeostasis model of NSSI (Stanley, 2010), childhood neglect and genetic vulnerability lead to a chronically lower level of endogenous opioids, which in the event of stress can be restored by engaging in NSSI.
Stanley (2010) found that cerebrospinal fluid beta-endorphin and met-enkephalin levels of endogenous opioids were significantly lower in patients with NSSI.
|
Concluding self-harm
The most accurate and consistent results about neurotransmitters affecting NSSI and self-harm are the reduced levels of cortisol and endogenous opioids in an individual, which cause an alteration in the stress response. The conclusions on other neurotransmitters like serotonin and dopamine are not consistent therefore further research is required in this field.
Addiction to exercise
Several studies show the relationship between exercise in an intensive way and blood plasma endorphin levels. Endorphins are endogenous opioids which are released from the pituitary gland and are believed to be responsible in mediating analgesia, induce euphoria and play a role in the reward system of the brain.
Exercise addiction is based on several criteria by Hausenblas and Downs (2002):
Tolerance: The individual starts pushing himself further in order to feel the desired effect.
Withdrawal: Negative effects such as anxiety, irritability and restlessness, starts to arise when the individual is not exercising.
Lack of control: The inability to cease or reduce the amount of exercise.
Intension Effects: Unable to stay with a routine as evidenced by exceeding the amount of time being devoted to exercise or consistently going beyond the intended amount.
Time: Dedicating a lot of time preparing for, engaging and recovering from exercise.
Reduction in other activities: Giving exercise priority above other social and recreational activities.
Continuance: Continues to exercise even though the individual is conscious of the physical, physiological and interpersonal problems.
These definitions are most closely aligned with the DSM-5 criteria for behavioural addiction, modelled after those for substance addiction.
Distinguishing exercise addiction
Like many other behavioural addictions, exercise addiction can be compulsive or impulsive (Freimuth et al., 2011). An addiction must be distinguished from other cases like an athlete devotes a lot of his time to exercise, have to reduce other activities and experience withdrawal when the amount of training Is reduced. Although in this case the athlete meets three of the above mentioned criteria, he is not necessarily addicted to his sport.
An impulsive behaviour consists of rapid and unplanned responses to an external or internal stimuli. In this type of behaviour, the individual is not thinking of the possible negative consequences and is driven by a desired positive reward. Exercise is this type, where it is an enjoyable activity but in its addictive form there is no consideration for any possible negative effects. Also, addictive behaviours unlike impulse-control disorders develop tolerance and withdrawal.
Exercise addiction is shown by research that like a compulsion, it is maintained by its mood-altering effects where it extends beyond reducing anxiety and lessening negative effects like anger, depression and boredom. There is an euphoric feeling generated by the endorphins resulting from intensive exercise which play a role in addiction (Freimuth et al., 2011).
Addictions co-occurring with exercise addiction
Research shows that around 15-20% of exercise addicts, also tend to be addicted to nicotine, alcohol or illegal drugs. For example, those athletes using stimulants to improve their athletic performance can become addicted to these substances. Eating disorders are the most common disorder that can co-occur with exercise addiction. This amounts to 39-48% of people suffering from eating disorders also suffering from exercise addiction. When these two co-occur, it can happen that only one problem is treated which is that of eating disorder since it is better known and therefore the patient’s secondary exercise addiction remains hidden. Evidence shows that appetite loss increases the endorphin release (Davis and Claridge, 1998). Davis and Claridge proposed a theory known as Auto-Addiction Opioid Model, suggesting that individuals with an eating disorder become addicted to the increase in endorphin activity and therefore restrict calories and exercise obsessively.
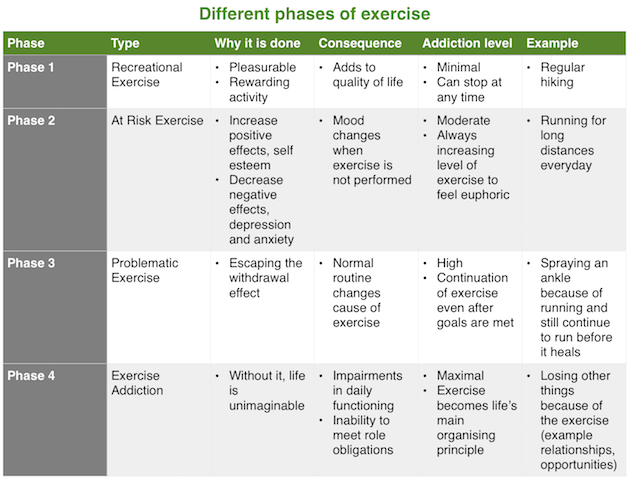
Phases of addiction
Freimuth’s (2008) constructed distinguishing phases of addiction which can be used to distinguish between recreational exercise and exercise addiction. With these phases, a clinician can decide when a normal behaviour is becoming addictive and vice versa.
|
Addiction to Sexual Masochism
Sexual masochism is defined by the consensual acts performed by a sexual masochist which involve pain as a central to the whole experience. These acts include being humiliated, bound or beaten amongst others. People being a submissive - being the ones experiencing the acts - in these kind of relationships describe the events as experiencing a ‘high’ and the euphoric feeling. This is in fact the cause of the endorphins released and the dopamine building up in their body. Submissives also say that the act leaves them with a unique and intense sensual gratification, making them want more the second they stop. Marks and pain that remain there after the session are said to make them happy as they bring back memories of the act. As the level of pain is adapted to by time, people in these acts say that they increase the pain threshold from time to time. This is as the pain is adjusted to, less endorphins are released in the brain and without the euphoric feeling these substances bring with them, the submissives will feel down and a really bad sense of withdrawal kicks in. (Kurt and Ronel, 2016)
Conclusion
Beta-endorphins are clearly the root to every pain addiction. The sense of euphoria they bring with them as an individual repeatedly performs acts of pain or from increasing the threshold of pain, upscales the unpleasant feeling of the act of pain itself. This is why pain is also easily to get addicted to. In order to achieve the ‘high’ one does not need any special resources (like for example drugs or some mechanisms); an individual can achieve an increase of endorphins basically everywhere at anytime and at no or little cost.
As a result, pain addiction is increasing and new ways of achieving the increase of beta-endorphins through some kind of pain are always being evolved.
References
Akural E.; Järvimäki V.; Alaniska K.; Oikarinen K.; Alahuhta S. (2015): Peripheral morphine reduces acute pain in inflamed tissue after third molar extraction: A double-blind, randomized, active-controlled clinical trial. Scandinavian Journal of Pain 11: 59-64.
Ashrafion L.; Bohnert K. M.; Jannausch M.; Ilgen M. A. (2014): Characteristics of substance use disorder treatment patients using medical cannabis for pain. Addictive Behaviors 42: 185-188.
Brain K. L.; Haines J.; Williams C. L. (1998): The psychophysiology of self-mutilation: Evidence of tension reduction. Archives of Suicide Research 4(3): 227-242.
Cheatle M. D. (2016): Facing the Challenge of Pain Management and Opioid Misuse, Abuse and Opioid-Related Fatalities. Expert Review of Clinical Pharmacology 1-4
Davis C.; Claridge G (1998): The eating disorders as addiction: a psychobiological perspective. Addictive Behaviors 23(4): 463-475.
Freimuth M.; Moniz S.; Kim S. R. (2011): Clarifying Exercise Addiction: Differential Diagnosis, Co-occurring Disorders, and Phases of Addiction. International Journal of Environmental Research and Public Health 8(10): 4069-4081.
Groschwitz R. C.; Plener P. L. (2012): The Neurobiology of Non-Suicidal Selj-injury (NSSI): A review. Suicidology Online 3: 24-32
Haines J.; Williams C. L.; Brain K. L.; Wilson G. V. (1995): The psychophysiology of selfmutilation. Journal of Abnormal Psychology 104(3): 471-489.
Hausenblas H.A.; Downs D.S. (2002): How much is too much? The development and validation of the Exercise Addiction scale. Psychology and Health 17(4): 387-404.
Heim C.; Ehlert U.; Hellhammer D. H. (2000): The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology 25(1): 1-35.
Kaess M.; Hille M.; Parzer P.; Maser-Gluth C.; Resch F.; Brunner R. (2012): Alterations in the neuroendocrinological stress response to acute psychosocial stress in adolescents engaging in nonsuicidal self-injury. Psychoneuroendocrinology 37(1): 157-161.
Kurt H.; Ronel N. (2016): Addicted to Pain: A Preliminary Model of Sexual Masochism as Addiction. International Journal of Offender Therapy and Comparative Criminology 1–15
Ling W.; Mooney L.; Hillhouse M. (2011): Prescription opioid abuse, pain and addiction: Clinical issues and implications. Drug Alcohol Review 30(3): 300–305.
Nock M. K.; Mendes W. B.(2008): Physiological arousal, distress tolerance, and social problem solving deficits among adolescent self-injurers. Journal of Consulting and Clinical Psychology 76(1): 28-38.
Novak M. A. (2003): Self-injurious behavior in rhesus monkeys: New insights into its etiology, physiology, and treatment. American Journal of Primatology 59(1): 3–19.
Roaldset O.; Bakken A. M.; Bjørkly, S. (2010): A prospective study of lipids and serotonin as risk markers of violence and self-harm in acute psychiatric patients. Psychiatry Research 186(2-3): 293-299.
Salsitz E. A. (2015): Chronic Pain, Chronic Opioid Addiction: a Complex Nexus. Journal of Medical Toxicology 12(1): 54-57.
Sprouse-Blum A. S.; Smith G.; Sugai D.; Don Parsa F. (2010): Understanding Endorphins and Their Importance in Pain Management. Hawai’i Medical Journal 69(3): 70-71.
Stanley B.; Sher L.; Wilson S.; Ekman R.; Huang Y.; Mann J. J. (2010): Non-suicidal self injurious behaviour, endogenous opioids and monoamine neurotransmitters. Journal of Affective Disorders 124(1-2): 134-140
Watson S. L.; McCoy J. G.; Fontenot M. B.; Hanbury D. B.; Ward C. P. (2009): L-Tryptophan and Correlates of Self-Injurious Behavior in Small-Eared Bushbabies (Otolemur garnettii). Journal of the American Association for Laboratory Animal Science 48(2): 185-191.