|
Size: 43
Comment:
|
Size: 9595
Comment:
|
| Deletions are marked like this. | Additions are marked like this. |
| Line 2: | Line 2: |
| = Physiology of pain addiction; behavioural effects = Addiction is a condition that arises when a being consumes substances or engages in activities that can be pleasurable at first, but the prolonged ingestion or act of which becomes a necessity. It emerges by the search of the ‘euphoric’ feeling a substance or activity brings with it. This feeling is the cause of the increase of the level of the striatal '''dopamine''' neurotransmitter. Users may not be aware that their compulsive behaviour is out of control and also once a being is addicted an entirely separate set of events or stressors may sustain and maybe amplify the addiction. Addiction can eventually lead to abuse. When relating addiction to pain, it is actually the endorphins released in the system which aid the dopamine release and gets a being addicted, forming a dependency on their release. <<TableOfContents(3)>> == Pain == Pain is a feeling of discomfort, distress or even agony depending on how severe it is. It has been defined as a biopsychosocial phenomenon that includes sensory, emotional, cognitive, developmental, behavioral, spiritual, and cultural components. (Salsitz, 2015) It is part of the body's defense system, producing a '''reflexive retraction''' from the painful stimulus, and protects the affected body part while it heals, and also avoid that harmful situation in the future. Pain can be either acute or chronic. Both types can be intense but chronic is the type of pain that lasts much longer, while acute pain is short lived. Pain stimuli starts from an electrical impulse from sensory receptors of the skin - nociceptors - to the spinal cord, acting as a relay center. The electrical impulse can be suppressed or enhanced before going to the brain. The brain then, produces several different neuroreceptors - such as glutamate - which then cause an impulse and reaches the thalamus and after the brain cortex. === Pain management === Pain management can be natural or artificial ==== Natural pain management ==== One of the main types of these endogenous opioids are '''beta endorphins'''. These are neuropeptides, which possess morphine like effects and are involved in the processes which bring happiness to a being - maybe even give a euphoric feeling. This is the part of the process which can get addicting. Physiological stressors such as pain, stimulate the synthesis of the the corticotroponin-releasing hormone (CRH) in the '''hypothalamus'''. This hormone is the one which triggers the '''anterior pituitary gland''' to synthesise the beta-endorphins. They are synthesised from their precursor protein proopiomelanocortin (POMC) along with other hormones such as the alpha-melanocyte stimulating hormone (MSH) and the adrenocorticotropin (ACTH). Beta-endorphins are also stored in the anterior pituitary. When there are enough beta-endorphins a negative feedback inhibits the further production of CRH. ||<tablebgcolor="#eeeeee" tablestyle="float:center;font-size:0.85em;margin:0 0 0 0; "style="padding:0.5em; ;text-align:center"> {{attachment:Synthesis of beta-endorphins1.png|pop-up text}} <<BR>>'''Fig 1.'''<<BR>>''Synthesis of beta-endorphins'' || Beta-endorphins act in both the peripheral and the central nervous system. They '''produce analgesia''' by binding to opioid receptors (usually the mu subtype). They bind to the receptors at both the presynaptic and postsynaptic nerve terminals but they mostly exert their effect through the presynaptic binding. In the peripheral nervous system (PNS), a cascade of reactions is induced after binding, which result in the inhibition of tachykinins release. These proteins - an example being substance P - are involved in the transmission of pain. In the central nervous system (CNS) the beta-endorphins inhibit the release of GABA, an inhibitory neurotransmitter, which then results in the overproduction of dopamine - a compound associated with pleasure (Sprouse-Blum et al., 2010). ||<tablebgcolor="#eeeeee" tablestyle="float:center;font-size:0.85em;margin:0 0 0 0; "style="padding:0.5em; ;text-align:center"> {{attachment:be.png|pop-up text}} <<BR>>'''Fig 2.'''<<BR>>''Structure of a beta-endorphin'' || === Artificial pain management === Opioid therapy is regarded as necessary in the treatment of acute and chronic pain. These artificial opioids resemble the functions of endogenous opioids by relieving pain and giving the sense of a ‘high’ to the user - described as analgesia. These do so by binding to the same receptors of the endogenous opioids (mostly the mu-receptors) and so a sense of competition between the endogenous and the external opioids evolves when they are administered to the body. The external opioids can also inhibit the production of the endogenous opioid (Sprouse-Blum et al., 2010; Cheatle, 2016). '''Morphine''' is the most commonly used pain reliever in medicine and quite effective for post-operation pain and for cancer pain. However, in order for the morphine (and any other artificial opioids) to work, they have to be injected into inflamed tissue (Akural et al., 2015). Getting addicted to these opioids is quite easy, especially for people who have a history of opioid and drug abuse. Research has shown that patients with no prior use and abuse of opioids, being presently treated with opioid pain medications do not experience a sense of euphoria. For those that do get addicted to opioids substitution medications such as methadone and buprenorphine are the current pharmacotherapy used. These also bind to the opioid receptors of the brain but do not produce an analgesic effect (Ling et al., 2011). '''Cannabinoids''' are another, relatively new way of treating pain. They are mostly being used amongst young people who have a history of Substance Use Disoder (SUD). Research conducted to compare medical cannabis to the traditional pain treatment opioids shows that medical cannabis can also reduce the amount of pain to the same certain level as the other opioids. However it has been resulted that medical cannabis users, consume other types of pain treatment in comparison to the non-medical cannabis users (Ashrafioun et al., 2014). == Pain Addiction == === Self-harm === Self-harm is defined as a '''repetitive, intentional, direct injury to one’s body'''. It is has been stated that the reason of these behaviours happen in certain individuals, as a way of regulation when one undergoes an emotional degradation occurring due to stressful events and social situations. Examples of self-harm include: Cutting (example with a razor blade) Burning one’s own body Bruising Punching objects (for example a wall) Pulling out of hair. ==== Suicidal and non-suicidal self-harm ==== There are two types of self-harm, that is '''suicidal (SSI)''' and '''non-suicidal self-harm (NSSI)'''. NSSI has been a clinical problem with high prevalence rates in young individuals mostly. Even though there are many cases of NSSI, the neurobiological background of this is still poorly understood. In current classificatory systems, Non-suicidal self-injury is regarded as a symptom of borderline personality disorder (BPD). When one does self-harm consciously - a behaviour which can include suicidal intent, it is widely described as “An act with a non-fatal outcome in which an individual deliberately did one or more of the following: initiated behaviour (for example, self- cutting, jumping from a height), which they intended to cause self-harm; ingested a substance in excess of the prescribed or generally recognised therapeutic dose; ingested a non-ingestible substance or object”. However since NSSI is still in risk of developing a suicidal attempt, the neurological background of these clinical phenomena may be comparable. The risk of both SSI and NSSI can be both influenced by '''intrapersonal factors''' (existing within the mind) which make an individual more vulnerable, such as high aversive emotions and cognitions as well as poor distress tolerance. These could be due to genetic susceptibility causing high emotional and high cognitive reactivity which could also happen due to environmental adversities. (Groschwitz and Plener, 2012) ==== Emotional and physiological states causing self-harm ==== The following describes differences in physiological concentrations of natural chemicals found in the body, comparing those who self-harm and those who don't. There is mixed evidence concerning differing physiological states in individuals with some kind of psychopathology, however a '''decrease in physiological tension''' in acts of NSSI has been reported many times. Nock and Mendes (2008): compared 62 adolescents with a history of NSSI to 30 matched controls without NSSI. Physiological '''hyperarousal''' when confronted with a distressing task was found in the adolescents with NSSI (hyperarousal is measured by skin conductance). In the experiment of Kaess (2012) did not find any differences in the heart rate of adolescents with NSSI and healthy ones, while either finding any differences in skin conductance. Two studies reported that '''imagining an act of self injury can decreases physiological tension''', as measured example per skin conductance and heart rate in individuals with self injurious behaviours (Brain et al.,1998, Haines et al.,1995). A '''rapidly lowered heart rate''' was discovered when rhesus monkeys repeatedly self injured themselves, for example when biting themselves (Novak 2003). |
Physiology of pain addiction; behavioural effects
Addiction is a condition that arises when a being consumes substances or engages in activities that can be pleasurable at first, but the prolonged ingestion or act of which becomes a necessity. It emerges by the search of the ‘euphoric’ feeling a substance or activity brings with it. This feeling is the cause of the increase of the level of the striatal dopamine neurotransmitter. Users may not be aware that their compulsive behaviour is out of control and also once a being is addicted an entirely separate set of events or stressors may sustain and maybe amplify the addiction. Addiction can eventually lead to abuse.
When relating addiction to pain, it is actually the endorphins released in the system which aid the dopamine release and gets a being addicted, forming a dependency on their release.
Contents
Pain
Pain is a feeling of discomfort, distress or even agony depending on how severe it is. It has been defined as a biopsychosocial phenomenon that includes sensory, emotional, cognitive, developmental, behavioral, spiritual, and cultural components. (Salsitz, 2015) It is part of the body's defense system, producing a reflexive retraction from the painful stimulus, and protects the affected body part while it heals, and also avoid that harmful situation in the future. Pain can be either acute or chronic. Both types can be intense but chronic is the type of pain that lasts much longer, while acute pain is short lived.
Pain stimuli starts from an electrical impulse from sensory receptors of the skin - nociceptors - to the spinal cord, acting as a relay center. The electrical impulse can be suppressed or enhanced before going to the brain. The brain then, produces several different neuroreceptors - such as glutamate - which then cause an impulse and reaches the thalamus and after the brain cortex.
Pain management
Pain management can be natural or artificial
Natural pain management
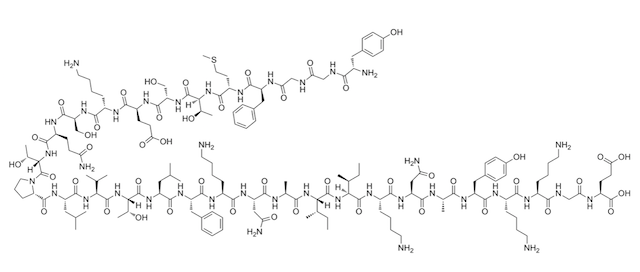
One of the main types of these endogenous opioids are beta endorphins. These are neuropeptides, which possess morphine like effects and are involved in the processes which bring happiness to a being - maybe even give a euphoric feeling. This is the part of the process which can get addicting.
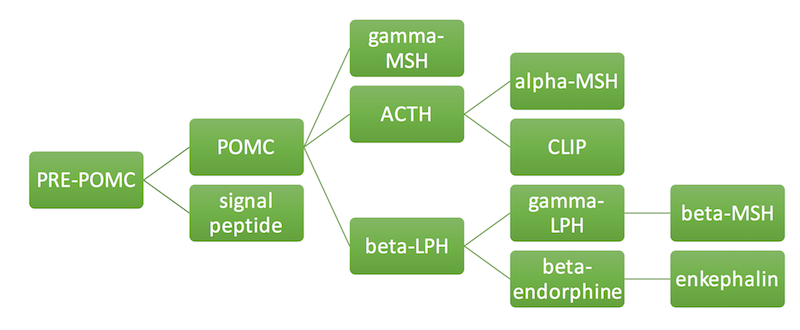
Physiological stressors such as pain, stimulate the synthesis of the the corticotroponin-releasing hormone (CRH) in the hypothalamus. This hormone is the one which triggers the anterior pituitary gland to synthesise the beta-endorphins. They are synthesised from their precursor protein proopiomelanocortin (POMC) along with other hormones such as the alpha-melanocyte stimulating hormone (MSH) and the adrenocorticotropin (ACTH). Beta-endorphins are also stored in the anterior pituitary. When there are enough beta-endorphins a negative feedback inhibits the further production of CRH.
|
Beta-endorphins act in both the peripheral and the central nervous system. They produce analgesia by binding to opioid receptors (usually the mu subtype). They bind to the receptors at both the presynaptic and postsynaptic nerve terminals but they mostly exert their effect through the presynaptic binding. In the peripheral nervous system (PNS), a cascade of reactions is induced after binding, which result in the inhibition of tachykinins release. These proteins - an example being substance P - are involved in the transmission of pain. In the central nervous system (CNS) the beta-endorphins inhibit the release of GABA, an inhibitory neurotransmitter, which then results in the overproduction of dopamine - a compound associated with pleasure (Sprouse-Blum et al., 2010).
|
Artificial pain management
Opioid therapy is regarded as necessary in the treatment of acute and chronic pain. These artificial opioids resemble the functions of endogenous opioids by relieving pain and giving the sense of a ‘high’ to the user - described as analgesia. These do so by binding to the same receptors of the endogenous opioids (mostly the mu-receptors) and so a sense of competition between the endogenous and the external opioids evolves when they are administered to the body. The external opioids can also inhibit the production of the endogenous opioid (Sprouse-Blum et al., 2010; Cheatle, 2016).
Morphine is the most commonly used pain reliever in medicine and quite effective for post-operation pain and for cancer pain. However, in order for the morphine (and any other artificial opioids) to work, they have to be injected into inflamed tissue (Akural et al., 2015).
Getting addicted to these opioids is quite easy, especially for people who have a history of opioid and drug abuse. Research has shown that patients with no prior use and abuse of opioids, being presently treated with opioid pain medications do not experience a sense of euphoria. For those that do get addicted to opioids substitution medications such as methadone and buprenorphine are the current pharmacotherapy used. These also bind to the opioid receptors of the brain but do not produce an analgesic effect (Ling et al., 2011).
Cannabinoids are another, relatively new way of treating pain. They are mostly being used amongst young people who have a history of Substance Use Disoder (SUD). Research conducted to compare medical cannabis to the traditional pain treatment opioids shows that medical cannabis can also reduce the amount of pain to the same certain level as the other opioids. However it has been resulted that medical cannabis users, consume other types of pain treatment in comparison to the non-medical cannabis users (Ashrafioun et al., 2014).
Pain Addiction
Self-harm
Self-harm is defined as a repetitive, intentional, direct injury to one’s body. It is has been stated that the reason of these behaviours happen in certain individuals, as a way of regulation when one undergoes an emotional degradation occurring due to stressful events and social situations.
Examples of self-harm include:
Cutting (example with a razor blade)
Burning one’s own body
Bruising
Punching objects (for example a wall)
Pulling out of hair.
Suicidal and non-suicidal self-harm
There are two types of self-harm, that is suicidal (SSI) and non-suicidal self-harm (NSSI). NSSI has been a clinical problem with high prevalence rates in young individuals mostly. Even though there are many cases of NSSI, the neurobiological background of this is still poorly understood. In current classificatory systems, Non-suicidal self-injury is regarded as a symptom of borderline personality disorder (BPD). When one does self-harm consciously - a behaviour which can include suicidal intent, it is widely described as “An act with a non-fatal outcome in which an individual deliberately did one or more of the following: initiated behaviour (for example, self- cutting, jumping from a height), which they intended to cause self-harm; ingested a substance in excess of the prescribed or generally recognised therapeutic dose; ingested a non-ingestible substance or object”. However since NSSI is still in risk of developing a suicidal attempt, the neurological background of these clinical phenomena may be comparable. The risk of both SSI and NSSI can be both influenced by intrapersonal factors (existing within the mind) which make an individual more vulnerable, such as high aversive emotions and cognitions as well as poor distress tolerance. These could be due to genetic susceptibility causing high emotional and high cognitive reactivity which could also happen due to environmental adversities. (Groschwitz and Plener, 2012)
Emotional and physiological states causing self-harm
The following describes differences in physiological concentrations of natural chemicals found in the body, comparing those who self-harm and those who don't. There is mixed evidence concerning differing physiological states in individuals with some kind of psychopathology, however a decrease in physiological tension in acts of NSSI has been reported many times. Nock and Mendes (2008): compared 62 adolescents with a history of NSSI to 30 matched controls without NSSI. Physiological hyperarousal when confronted with a distressing task was found in the adolescents with NSSI (hyperarousal is measured by skin conductance). In the experiment of Kaess (2012) did not find any differences in the heart rate of adolescents with NSSI and healthy ones, while either finding any differences in skin conductance.
Two studies reported that imagining an act of self injury can decreases physiological tension, as measured example per skin conductance and heart rate in individuals with self injurious behaviours (Brain et al.,1998, Haines et al.,1995). A rapidly lowered heart rate was discovered when rhesus monkeys repeatedly self injured themselves, for example when biting themselves (Novak 2003).